
You may prioritize the diagnosis and treatment of ocular surface disease (OSD) in your practice, but the daily cosmetic and skincare practices of your patients at home can interfere with your hard work in the clinic. The good news is that most of these individuals are open to your guidance and willing to purchase products that promote rather than harm their ocular health. By recommending and offering a carefully selected range of products at the point of care, you can support your patients’ desire to look and feel their best in their ocular surface restoration journey. I call this the DAO, or the dermatologic, aesthetic, and ophthalmologic overlaps that, in synchrony, can result in beautiful, healthy eyes.
A comprehensive clinician mindset that focuses on the DAO can improve your ability to address patients’ daily habits that contribute to OSD, increase patient satisfaction and engagement, and create a unique revenue stream from money that patients would otherwise spend on (the potentially wrong) products on Amazon, at the drug store, or the luxury department store.
DERMATOLOGIC CONSIDERATIONS
Intense pulsed light. The OptiLight (Lumenis) is the only intense pulsed light (IPL) device approved by the FDA for the treatment of dry eye disease (DED) associated with meibomian gland dysfunction (MGD). IPL treatment with this device can also address dermatologic and aesthetic changes of the face and eyelids such as rosacea, sun damage, and age-related skin color, texture, and tone issues. Patients often notice that, as their eyelid inflammation and symptoms of MGD and DED improve with IPL treatment, their eyelids also look and feel healthier. This is a win-win.
Unless your patient is currently using tretinoin to treat a precancerous skin condition, I recommend skipping this medication in favor of offering a rejuvenating strategy such as IPL, radiofrequency (Figure 1), radiofrequency microneedling, nonsurgical blepharoplasty with a plasma pen, or CO2 laser skin resurfacing. Midface and tear trough fillers can be used to enhance the patient’s appearance, improve the lower eyelid position, and support the lower eyelid mechanics, thereby improving DED symptoms, addressing nocturnal lid-seal insufficiency, and decreasing daytime blink insufficiency.

Figure 1. Appearance of the eye before IPL treatment and ThermiEyes (ThermiGen) radiofrequency treatment (A). Appearance of the eye 1 month later, after two IPL and ThermiEyes treatments (B).
Skincare. Because dermatologic and ophthalmic conditions often overlap, you may wish to consider stocking and dispensing compounded pharmaceutical-grade skin treatments for rosacea and seborrheic dermatitis, as my practice does. Cosmeceutical-grade skin care systems to improve skin color, texture, and tone of the face and eyelids are another potential offering. These systems can also be used after IPL to enhance improvements in rosacea, seborrheic dermatitis, and photoaging. When applied inside the orbital rim, however, many formulations can contribute to OSD. Ingredients and application patterns can significantly exacerbate OSD in some patients. At present, I am carefully evaluating several high-quality lines from manufacturers such as Epionce and Oculaire Skincare.
Lastly, you may wish to recommend and offer specific sunscreen products to your patients. The most universally tolerated product in my experience is Kinesys unscented (Kinesys); it works well for athletes and for patients with rosacea, and it can be applied under makeup. The top-selling zinc oxide formulation at my practice is manufactured by EltaMD Skincare.
AESTHETIC CONSIDERATIONS
Aesthetic. Depending on the technique used to administer them, injectable neuromodulators can benefit or harm the ocular surface. Avoid injecting these products in the crow’s feet area in patients with OSD unless they also experience blepharospasm. OSD-friendly injections are in the glabellar complex, frontalis (avoiding brow ptosis), prelacrimal sac area (to slow but not obstruct tear clearance), and masseters (if the patient experiences bruxism).
In one study, injecting a small amount of a neuromodulator into the pretarsal orbicularis oculi muscle cleared filaments in more than 90% of patients with filamentary keratitis.1 I also use this approach to reduce friction symptoms between the eyelid and conjunctiva and improve ocular surface staining in patients with superior limbic keratitis (Figure 2).
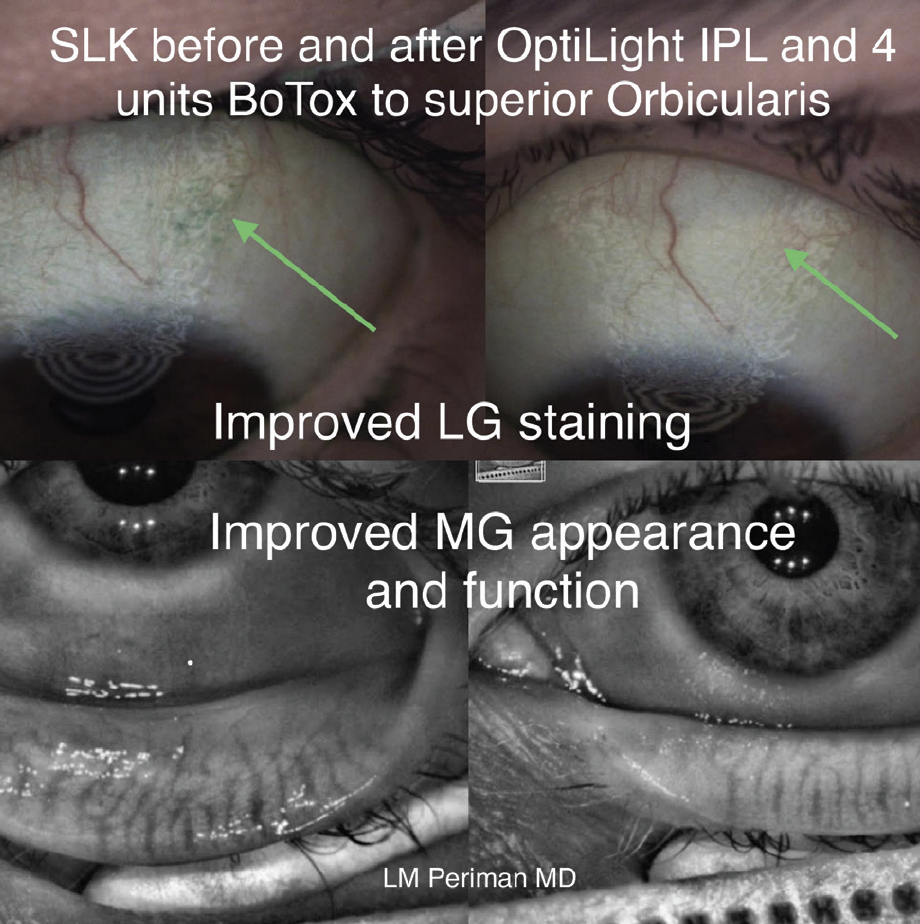
Figure 2. Lyssamine green (LG) staining (top) and meibomian gland (MG) appearance and function (bottom) improved after IPL and onabotulinumtoxinA (Botox Cosmetic, Allergan) treatment for superior limbic keratitis (SLK).
OPHTHALMOLOGIC CONSIDERATIONS
Prostaglandins. Prostaglandin analogues are a first-line treatment for glaucoma. Some patients may develop prostaglandin-associated periorbitopathy or MGD. In this situation, switching to another class of IOP-lowering medication is an option. Alternatively, laser trabeculoplasty and MIGS may be considered to reduce or eliminate a patient’s need for medical therapy. MGD treatment is appropriate.
Beware of patients who present with clear prostaglandin-induced side effects such as eyelid discoloration or dermatitis, abnormally thick and long eyelashes, periorbital fat atrophy, and MGD. Maintain your suspicion for possible self-administration of over-the-counter prostaglandin-adulterated eyelash growth serum (ELGS). Rodan + Fields faces two class action lawsuits alleging that it failed to disclose the risks associated with isopropyl cloprostenate, a prostaglandin analogue that is an ingredient in the company’s Lash Boost ELGS. Ironshore Specialty Insurance recently sued Rodan + Fields as well.2
Labels on ELGSs stating that the products are free of prostaglandins may be a marketing trick; look for chemical names containing the word fragment “prost” to signify the presence of a prostaglandin. ELGSs formulated without prostaglandin analogues are flooding the aesthetics market. These products may contain hair growth peptides, and the peer-reviewed research evaluating their impact on ocular surface health is scant.
Furthermore, the high preservative load of any water-containing formulation can harm the ocular surface. In my experience, the eyelash-lengthening performance of the few water-free ELGS products with simpler formulations has been lacking, and several water-free formulations I have tried caused prolonged blurriness of vision. I advise my patients to discontinue using over-the-counter ELGSs. When we double down on managing the inflammation, Demodex, and rosacea burdens of our blepharitis patients, the result is often healthier, naturally longer eyelashes.
Lid hygiene. This area of eye care has advanced beyond the use of baby shampoo, which can harm the ocular surface. Because most patients with MGD have a lipid deficiency, I offer them surfactant-free options such as NuLids (NuLids Medical) and ZocuShield (Okra), a polysaccharide product with antiinflammatory properties, for use at night and Optase tea tree oil eyelid cleansing gel (Scope) for fast application during a morning shower. Hypochlorous acid products such as Avenova (NovaBay Pharmaceuticals) and MyboClean (Danelli Ocular Creations) are additional options. Scope’s commercial formulation is a good value for patients and can be ordered online or sold in the clinic.
Nutraceuticals. Nutritional supplements are a component of comprehensive dry eye care that you may wish to make available in your practice. My practice offers HydroEye (ScienceBased Health) and CurcuOne (Wellness26). I explain to patients, however, that these products are not a substitute for a healthy diet. Many of my patients have achieved improved total ocular surface health and overall health with the Whole30 program.
CONCLUSION
There is significant overlap among dermatology, aesthetics, and ophthalmology. Think in terms of 3D overlaps instead of flat, binary algorithms. Keeping in mind where these fields overlap, confidently making recommendations to patients, and providing them with convenient access in your office to the best products can help these individuals achieve excellent DED and MGD outcomes.
1. Gumus K, Lee S, Yen MT, Pflugfelder SC. Botulinum toxin injection for the management of refractory filamentary keratitis. Arch Ophthalmol. 2012;130(4):446-450.
2. Voytko L. More trouble for embattled skincare firm Rodan + Fields: its insurer is suing. Forbes. July 8, 2021. Accessed October 25, 2021. https://www.forbes.com/sites/lisettevoytko/2021/07/08/more-trouble-for-embattled-skincare-firm-rodan–fields-its-insurer-is-suing/?sh=750dc0ce7a9e




