CASE PRESENTATION
A 39-year-old man presents with a complaint of a gradual reduction in vision in the right eye and intermittent headache over the past 6 months. The patient is a professional fighter. He underwent LASIK 5 years ago, and the flap was created using an IntraLase FS laser (Johnson & Johnson Vision).
Upon examination, his UCVA is 6/12 OD and 6/7.5 OS. His BCVA is 6/6 with a manifest refraction of +3.50 -6.00 x 75º OD and 6/5 with a manifest refraction of +0.25 -2.00 x 90º OS. An anterior segment examination reveals meibomian gland dysfunction, decreased tear breakup time, and inferior punctate corneal staining in each eye. A LASIK flap is visible in each eye. No corneal scarring, dystrophy, or epithelial ingrowth is observed. No lens opacity is evident in either eye, and the posterior segment examination of each eye is within normal limits. Corneal topography of the right and left eyes is shown in Figures 1 and 2, respectively, and epithelial thickness maps are shown in Figure 3.
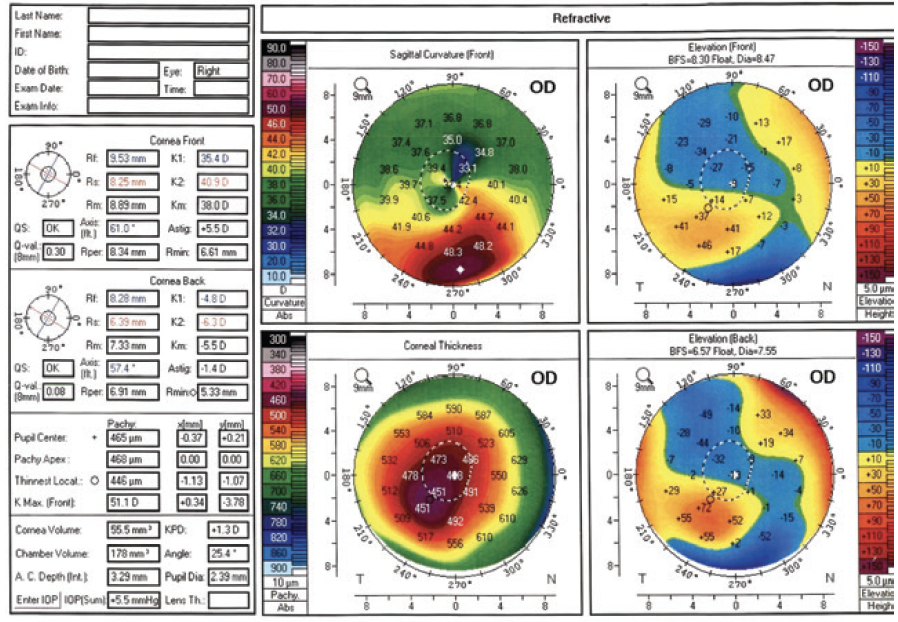
Figure 1. Corneal topography of the right eye.
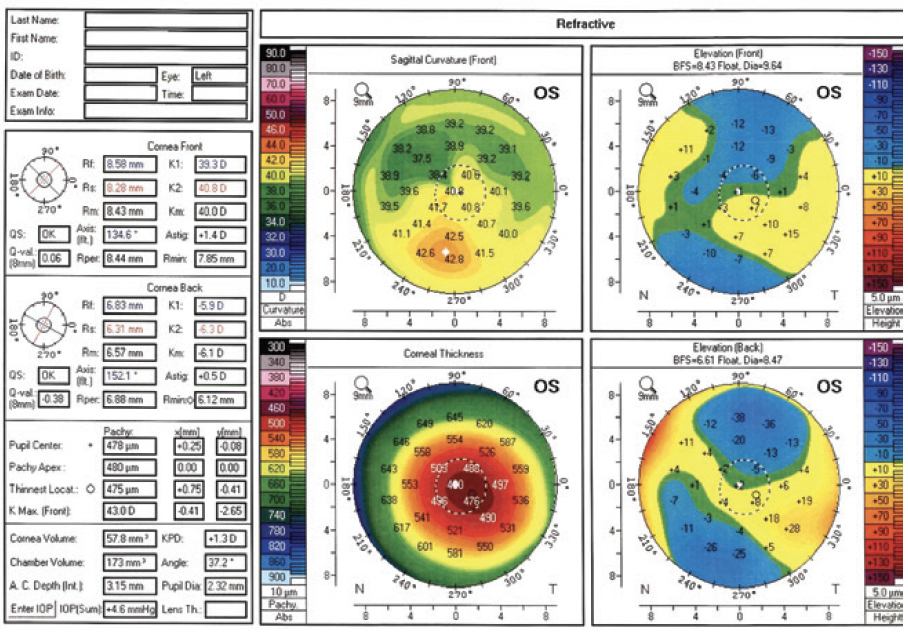
Figure 2. Corneal topography of the left eye.
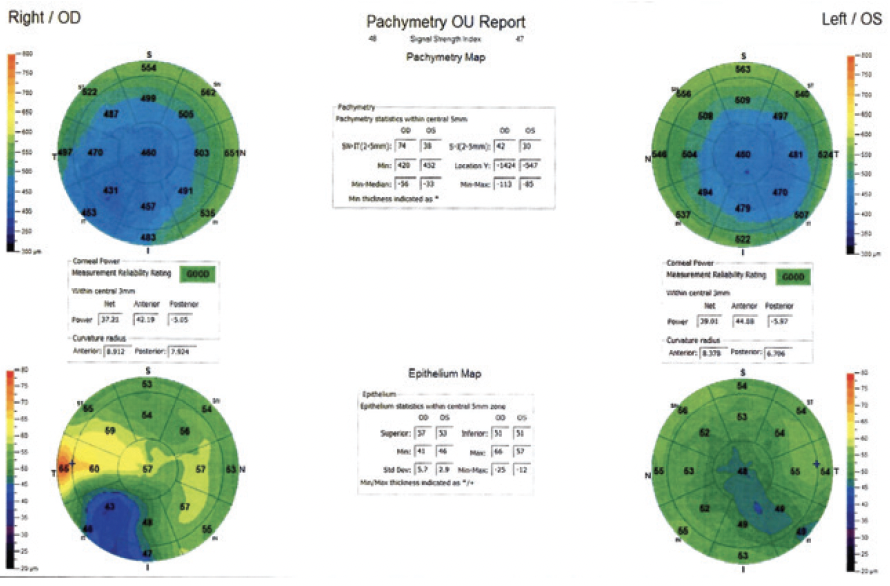
Figure 3. Epithelial thickness maps of both eyes.
The patient is keen to improve his vision and resolve the headache, and he wishes to remain spectacle independent. How would you approach this case? One year later, corneal topography is repeated in the left eye (Figure 4). How would you proceed?
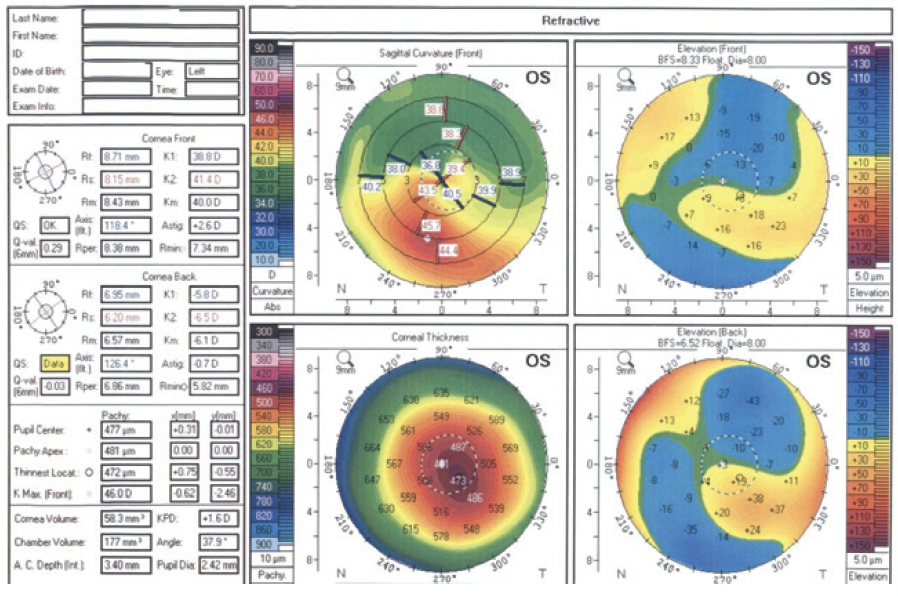
Figure 4. Corneal topography of the left eye 1 year after initial presentation.
—Case prepared by Masara Laginaf, MBBS BSc (Hons), FRCOphth, and Allon Barsam, MD, MA, FRCOphth

COLMAN R. KRAFF, MD
The patient appears to have developed corneal ectasia after LASIK. Without being able to view his preoperative corneal topography, it is unclear to me if the patient was at increased risk of developing this condition. Upon presentation, the corneal ectasia in the right eye is already significant, and in the left eye there are early potential signs of ectatic disease on topography. This is confirmed 1 year later with topography, which demonstrates significant progression. Post-LASIK corneal ectasia often progresses rapidly and then stabilizes. It appears that the patient’s ectasia is actively progressing, at least in the left eye. No topography is provided for the right eye from 1 year after presentation.
In this clinical situation, the first goal is to stabilize the ectasia. CXL would be the best option here. I would treat the left eye first, and I would subsequently treat the right eye regardless of whether recent ectatic progression has been documented. In the United States, where I practice, the only FDA-approved option is an epithelium-off (epi-off) procedure using the KXL System (Glaukos). I perform CXL on one eye at a time, usually starting with the eye that has more active or advanced ectasia. After reepithelialization has been achieved and visual acuity has returned to the pre-CXL level in the first eye, I perform CXL on the second eye.
Once clinical stability of the ectasia is documented in both of the patient’s eyes, I would discuss with him his options for achieving spectacle independence. I would wait until serial refractions have been stable and corneal topography has shown no signs of corneal steepening for at least 1 year before considering another procedure.
It may be difficult to achieve spectacle independence for the patient because of his clinical situation and profession. I would not offer surface ablation to someone who has recently experienced progressive ectasia. Given his prescription, I am concerned about removing a significant amount tissue from an already weakened cornea. Outside the United States, implanting a Visian Toric ICL (STAAR Surgical) might be an option for visual rehabilitation, and it is one that maintains accommodation. The patient’s profession, however, puts him at increased risk of ocular trauma, which could cause complications with a phakic IOL. This would require a detailed preoperative discussion.

MARGUERITE B. MCDONALD, MD, FACS
The patient’s history is typical of post-LASIK ectasia, which can occur in one or both eyes. In this case, there has been a slow decrease in vision in the right eye with increased astigmatism in the manifest refraction. The topographic maps show inferior corneal steepening in both eyes that has progressed in the left eye over 1 year. There is corresponding epithelial thinning over the inferior ectatic areas.
Without the patient’s preoperative manifest refractions or topographic maps, it is impossible to determine if he had preexisting keratoconus or other risk factors. CXL would likely regularize the cornea by flattening it and making it more spherical in shape. CXL should also vastly reduce the likelihood that the ectasia will progress to the point that a penetrating keratoplasty is required.
In this situation, some surgeons would offer to perform PRK in combination with, before, or after CXL. This is not an unreasonable strategy. I, however, would not offer it at this time and instead would perform CXL alone on each eye and offer to have the patient fitted for contact lenses if necessary. Once more long-term data on the safety and efficacy of combined CXL and PRK for the treatment of post-LASIK ectasia and more information on the optimal sequencing and timing of these treatments are available, patients similar to this one will have more options.
Because he is a professional fighter, this patient may elect to wear soft contact lenses during his bouts because these lenses are less apt to be dislodged during a match. Outside of the ring, he may benefit from wearing rigid gas permeable or scleral lenses.


MAJID MOSHIRFAR, MD, AND RACHEL HUYNH
There is evidence of dry eye disease, suggesting that the patient could benefit from ocular surface rehabilitation. His history, corneal topography, and epithelial thickness maps, however, are consistent with post-LASIK ectasia. Dry eye disease can be associated with corneal anterior surface abnormalities and even inferior steepening on topography, but with dry eye alone the eye would not exhibit posterior surface elevation or thinning with surrounding hyperplasia on epithelial maps that corresponds with the regions of steepening. Corneal thickness is greater than 400 µm and sufficient to allow epi-off CXL to be performed to stabilize the cornea using the standard Dresden protocol (UV irradiation 3 mW/cm2 for 30 minutes).
To improve the likelihood that spectacle independence can be achieved, intrastromal corneal ring segments (ICRSs; Intacs, Addition Technology) could be placed to flatten the cornea 3 months after CXL if refractive stability is demonstrated at that time. A nomogram could be used to determine whether an inferior ICRS or bilateral ICRSs on each side of the cornea should be placed. If refractive stability is demonstrated 3 months after ICRS placement, topography-guided PRK using Contoura Vision with the WaveLight EX500 excimer laser (Alcon) could be performed to regularize the topography and reduce any residual refractive error. Correcting more than 70% of the refractive error, however, is not recommended because it could lead to further thinning and corneal instability. It may not be possible for the patient to achieve spectacle independence, so it will be necessary to explain to him that he may need to wear glasses or specialty contact lenses after surgery. His refractive stability should be monitored, especially after 5 years, because of the decrease in CXL response.1
Some surgeons perform simultaneous CXL and PRK. We prefer, however, to perform the procedures sequentially so that the shape of the eye can be normalized and refractive stability ensured before additional tissue is removed.
In the future, other options may be available to patients similar to this one. Promising 6-month results have been reported with under-flap CXL. In this technique, the LASIK flap is fully retracted, the stromal bed is soaked with riboflavin solution, the flap is repositioned, and then UV irradiation is performed. Long-term stability with this technique, however, has yet to be demonstrated.2 Another technique under investigation is repeated CXL assisted by transepithelial double-cycle iontophoresis in patients who experience keratoconus progression after a primary CXL procedure. This epithelium-on technique demonstrated a greater number and depth of corneal crosslinks compared to baseline after primary CXL.3 For post-LASIK ectasia, this technique could be used to reduce recovery time compared with traditional epi-off CXL.


WHAT WAS DONE: MASARA LAGINAF, MBBS BSC(HONS), FRCOPHTH, AND ALLON BARSAM, MD, MA, FRCOPHTH
The initial approach was to optimize the ocular surface with the use of preservative-free artificial tears, the regular application of a heated eye mask, and oral flaxseed oil supplements 1 g administered twice daily. The post-LASIK ectasia in the right eye was treated with topography-guided transepithelial PRK combined with CXL and adjunctive mitomycin C. The ocular surface required close monitoring in the early postoperative period, with the addition of oral doxycycline 100 mg administered daily and intensive therapy with artificial tears to aid healing of the epithelium.
One year after surgery, progression of the post-LASIK ectasia was confirmed in the left eye. Transepithelial advanced surface laser ablation (epithelium-guided phototherapeutic keratectomy) combined with CXL and adjunctive mitomycin C was performed.
No corneal haze or scarring was observed in either eye postoperatively. The patient’s final UCVA was 6/6 OU. His BCVA was 6/5 OU with manifest refractions of +1.00 -1.00 x 80º OD and plano -2.00 x 110º OS.
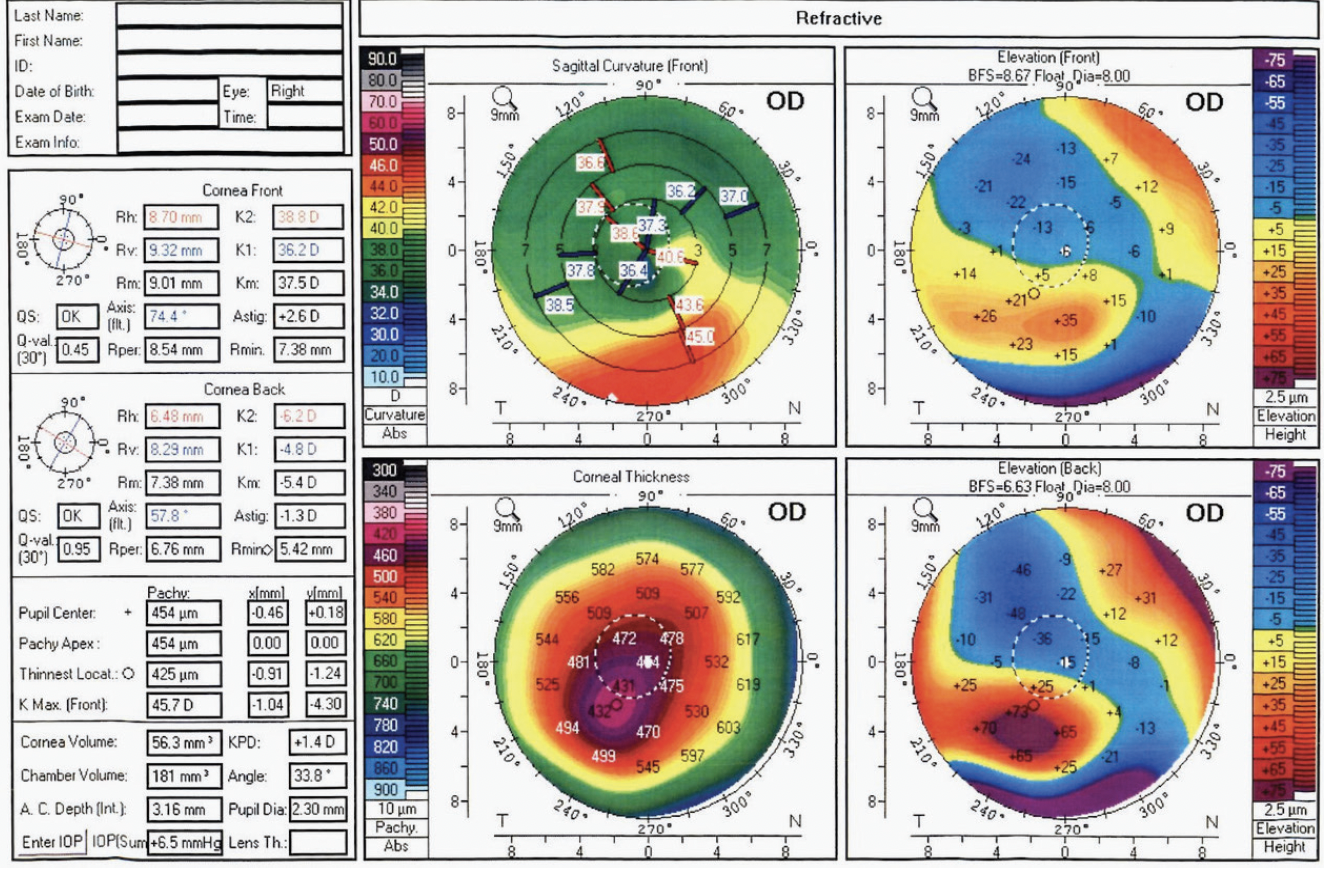
Figure 5. Postoperative corneal topography of the right eye.
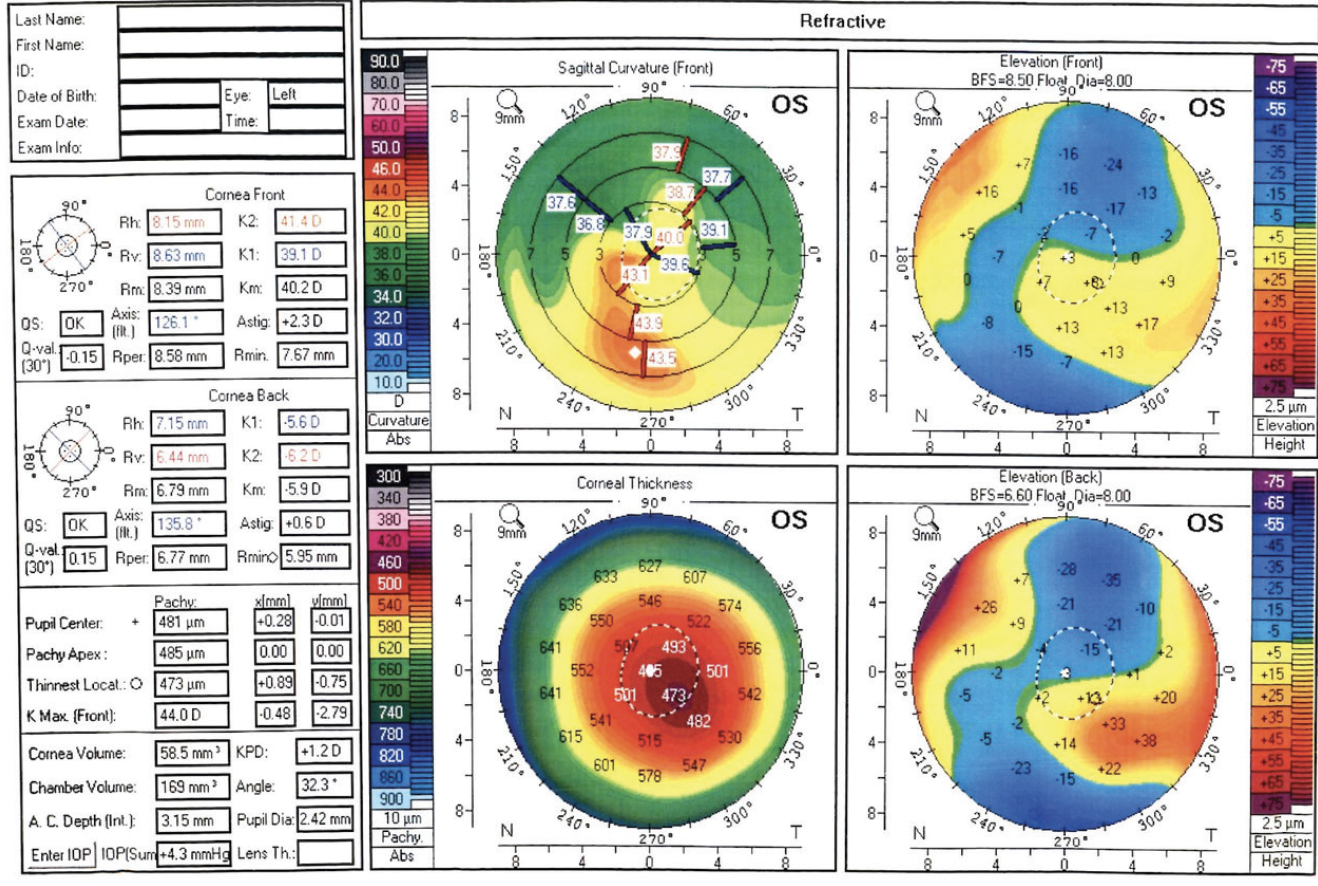
Figure 6. Postoperative corneal topography of the left eye.
The aim of topography-guided PRK and phototherapeutic keratectomy was to regularize the anterior corneal surface (Figures 5 and 6), and CXL was performed to stabilize the ectasia. There were no signs of ectatic progression 5 years after surgery. Close attention to the ocular surface was key to the patient’s successful outcome.
1. Seifert F, Seufert F, Hommes D, et al. Ten year results after corneal collagen crosslinking with riboflavin and UV-A irradiation (CXL) for keratoconus – when to repeat CXL? Invest Ophthalmol Vis Sci. 2019;60(9):339. Accessed September 10, 2021. https://iovs.arvojournals.org/article.aspx?articleid=2740988
2. Wallerstein A, Adiguzel E, Gauvin M, Mohammad-Shahi N, Cohen M. Under-flap stromal bed CXL for early post-LASIK ectasia: a novel treatment technique. Clin Ophthalmol. 2016;11:1-8.
3. Wu H, Li L, Luo S, et al. Safety and efficacy of repeated crosslinking assisted by transepithelial double–cycle iontophoresis in keratoconus progression after primary corneal crosslinking. Published January 7, 2021. Eye (Lond). doi:10.1038/s41433-020-01365-1




