My Experience and My Advice
Deepinder K. Dhaliwal, MD, L.Ac

Repetitive tasks that require fine motor control and close visual focus—especially when performed under stressful circumstances—and those that entail maintaining awkward body positions for prolonged periods are associated with a high risk of musculoskeletal disorders (MSDs) of the back, shoulders, neck, and arms. It is therefore not surprising that ophthalmologists are at increased risk of developing MSDs.1
In a 2005 survey of ophthalmologists, 51.8% of respondents reported that they had experienced neck or back pain at some point in their careers, and approximately 15% had curtailed their work as a consequence.2
MY STORY
In 2015, I slipped on a puddle of water on the OR floor and fell. I subsequently developed a large L5-S1 disc herniation (Figure 1) that caused severe back pain and progressive weakness in my right leg that prevented me from working or traveling. I saw two neurosurgeons and one orthopedic surgeon, all of whom were ready to operate, but I was not ready to undergo surgery.

Figure 1. An MRI of Dr. Dhaliwal’s spine in December 2015 showing an L5-S1 disc herniation (red circle).
I decided instead to attempt to alleviate my back pain and leg weakness with daily physical therapy, acupuncture twice per week, and daily meditation. With this conservative treatment approach, I am now 90% recovered based on my ability to function pain free and hope to continue improving.
ADVICE FOR MY FELLOW OPHTHALMOLOGISTS
Slit lamp. Poor posture during the slit-lamp examination is not uncommon among ophthalmologists.3 Raise the exam chair so that the base of your stool can slide under the patient’s footrest. Ask the patient to move toward you: “Scoot forward in the chair.” This can allow you to maintain proper posture with your head over your shoulders and your shoulders back. During laser procedures, your arms can rest on the table or soft support. The key point is not to crane your neck at the slit lamp.
Operating microscope. Neck strain can also occur at the operating microscope.3 You can maintain proper posture by tilting the microscope and keeping your shoulders down while operating, no matter how difficult the case (Figure 2).4 Alternatively, a heads-up display may be used during surgery.5 Microbreaks in between surgical cases have been shown to help decrease musculoskeletal strain. I simply pull my shoulders back and stretch my arms back after each case.
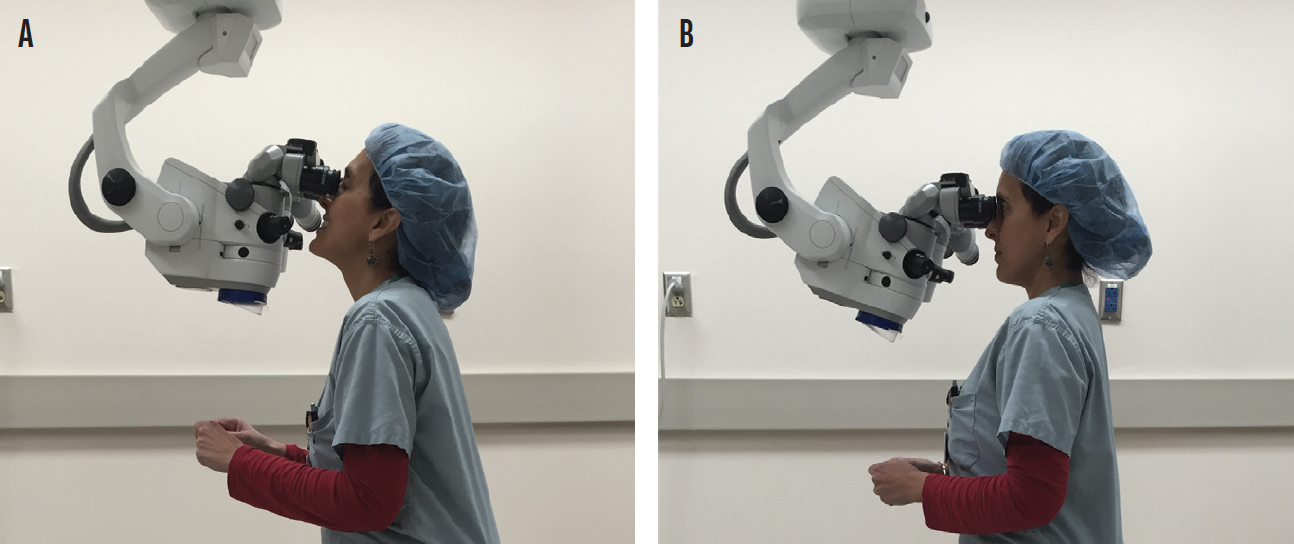
Figure 2. Dr. Dhaliwal demonstrating poor (A) and proper (B) posture at the operating microscope.
Figures 1 and 2 courtesy of Deepinder K. Dhaliwal, MD, L.AC
Indirect ophthalmoscope. The use of an indirect ophthalmoscope can require you to twist your neck and body into awkward positions.3 Choosing a lightweight model can decrease the shear load on and compression of the discs of your neck. Never bend over when using an indirect ophthalmoscope and try to keep your neck and back in a neutral position as much as possible. For example, elevate the patient’s chair so that their head is at eye level. To view the periphery of the retina, recline the patient’s chair to a 45° angle and tilt their head in various directions. Limit your neck flexion to movements of less than 25º and limit sideways bending to movements of less than 10º. When performing a scleral depression, support your hand with the patient’s head.6
Sitting. The vertebral bodies and discs normally carry about 80% of a person’s weight. Poor posture increases intervertebral pressure, thereby increasing the likelihood of disc injury. Sitting and standing erect helps displace the forces posteriorly and reduce the risk of disc injury. Compressive forces on discs are considerably less when standing than when sitting. Therefore, after a long day at work, go for a walk with your hands behind your back to reverse the forward posture instead of sitting on the couch.
To optimize your seated posture, consider using a lumbar support device and sit on a chair with adequate support for your back. Make sure you sit straight and have your computer screen at eye level so your neck can remain neutral.
Exercise. Performing exercises such as bridges, bird-dogs, side planks, clamshells, and planks are excellent ways to strengthen your core and reduce your risk of injury.
CONCLUSION
Proper ergonomic positioning can reduce your risk of injury. Be aware of your posture with every patient and take the time to adjust your equipment as needed. If you experience pain or radiculopathy, seek help immediately. Do not wait for the problem to become debilitating—a real risk given the requirements of our line of work.
1. Kitzman AS, Fethke NB, Baratz KH, Zimmerman MB, Hackbarth DJ, Gehrs KM. A survey study of musculoskeletal disorders among eye care physicians compared with family medicine physicians. Ophthalmology. 2012;119(2):213-220.
2. Dhimitri KC, McGwin Jr G, McNeal SF, et al. Symptoms of musculoskeletal disorders in ophthalmologists. Am J Ophthalmol. 2005;139(1):179-181.
3. Masket S. Ergonomics is everything! American Academy of Ophthalmology. May 13, 2020. Accessed October 11, 2021. https://www.aao.org/senior-ophthalmologists/scope/article/ergonomics-is-everything
4. Wallace BR 3rd. The 45 degree tilt: improvement in surgical ergonomics. J Cataract Refract Surg. 1999;25(2):174-176.
5. Eckardt C, Paulo EB. Heads-up surgery for vitreoretinal procedures: an experimental and clinical study. Retina. 2016;36(1):137-147.
6. Mehta S, Hubbard GB III. Avoiding neck strain in vitreoretinal surgery: an ergonomic approach to indirect ophthalmoscopy and laser photocoagulation. Retina. 2013;33(2):439-441.
Your Back, In Action
Alison D. Early, MD

I was a junior ophthalmology resident when I first became aware of nagging soreness in my neck and upper back at the end of a long day. I recall suspecting that my computer station was the problem because the sensation occurred primarily at the end of clinic when I routinely spent an hour or so completing the day’s charts. I adjusted the position of my keyboard, the height of my chair, and my seated posture and never considered that the activities of an entire day spent examining patients could be contributing to my discomfort.
Before starting my first “real” job, I had the opportunity to observe Michael E. Snyder, MD, in the OR. While excitedly taking notes on surgical techniques and absorbing dozens of pearls of wisdom, I noticed the attention he paid to his posture and positioning during surgery. Never before had I heard surgeons mention positioning themselves in a particular way rather than focus on only the patient’s position under the microscope.
A few short weeks into running my own practice, that familiar discomfort in my neck and back recurred. I first attributed the ache to carrying stress in my shoulders and dismissed it as an inevitable consequence of working on my own for the first time. (Even small patient management decisions feel big when there is no attending to give the final nod of approval.) On top of the general stressors of navigating a new practice, I had to figure out an electronic medical record system, find reliable childcare, and combat decision fatigue, among other things. It then occurred to me that poor ergonomics in the clinical setting could be contributing to my pain.
I began to research ways to improve my ergonomics in the clinic and the OR. To my surprise, I discovered that ophthalmologists have higher rates of MSDs than physicians in other specialties, such as family medicine, likely because of the static postures and repetitive positions ophthalmologists undertake.1 Computer stations in the clinical setting are not typically designed with ergonomics in mind, and surgeons must consider their posture and positioning during patient examinations and surgery. It is true that ophthalmologists are frequently seated, but repetitive strain from poor posture can lead to career-limiting cumulative trauma injuries.
CHANGES IN THE EXAM LANE AND OR
Exam lane. To achieve a straight, upright spine during patient examinations, I move the footrest of the patient’s exam chair out of the way. This can be achieved by slightly raising the patient’s chair so that the casters of the examination stool can fit underneath (Figure 3). For the occasional patient who does not need the footrest, it can be flipped up and out of the way to achieve the same spinal posture. I credit this small change with almost immediately relieving the upper spinal discomfort I had as the result of forward extension and reaching my neck toward the slit-lamp oculars.
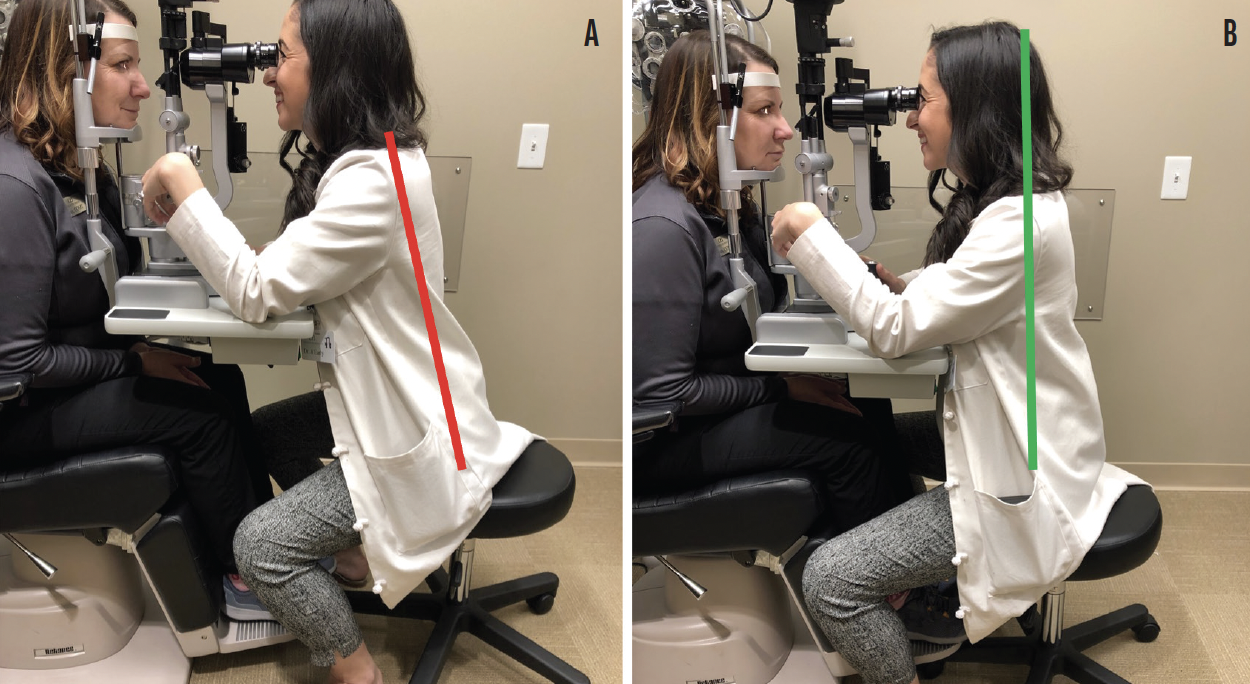
Figure 3. Forward extension to reach the slit-lamp oculars caused Dr. Early to experience upper spinal discomfort (A). She found that moving the footrest of the patient’s exam chair out of the way by raising the chair to allow the casters of her examination stool to fit underneath almost immediately relieved this discomfort (B).
OR. I protect my neck and spine in the OR by tilting the microscope oculars toward myself to allow a neutral neck position. Using the back support of the operating stool and the entire seat cushion and extending my legs to allow a wider range of ankle motion than can be had with knees at a right angle is another good practice. Footpedal elevators can also be used to position the footpedals similarly to in a car (Figure 4).

Figure 4. Nonergonomic positioning in the OR (A). Ergonomic positioning uses the entire seat cushion and back support of the operating stool with the physician’s legs extended to allow a wider range of ankle motion. Footpedal elevators are used to position the pedals similarly to the pedals in a car (B).
Figures 3 and 4 courtesy of Alison D. Early, MD
DAILY ATTIRE
When my practice reopened following the COVID-19 shutdown, I began to wear well-tailored scrubs and athletic shoes to work each day. They have become my permanent uniform. Wearing a skirt required me to assume awkward positions when examining patients.
Streamlining my wardrobe has also noticeably reduced stress for me overall because I no longer have to put together an outfit each day. Many highly successful people wear the same thing every day for just this reason.
CONCLUSION
Ophthalmologists are disproportionately affected by MSDs owing to repetitive strain and cumulative trauma incurred through long days spent in static, repetitive postures. By improving ergonomics and caring for their bodies, surgeons may be able to prolong their careers and overall well-being. Based on my experience, I recommend that young physicians and trainees take a proactive rather than a reactive approach to their musculoskeletal health.
1. Kitzmann AS, Fethke NB, Baratz KH, Zimmerman MB, Hackbarth DJ, Gehrs KM. A survey study of musculoskeletal disorders among eye care physicians compared with family medicine physicians. Ophthalmology. 2012;119(2):213-220.
Don’t Wait Until It’s Too Late
Steven G. Safran, MD

At all stages of our careers, we ophthalmologists must be aware of the importance of proper posture and ergonomic equipment to avoid musculoskeletal injury and its potentially career-ending ramifications.
Unfortunately, we often don’t realize we are doing damage until it is too late.
MY INJURY
Six years ago, at age 55, I began experiencing neck pain. In an attempt to alleviate it, I went to a chiropractor for an adjustment. Immediately afterward, I started experiencing numbness down my left arm, and my neck pain got worse—I was suddenly experiencing numbness in my left hand and shooting pain and parathesias in my neck and shoulder blade that would travel down my left arm with most movement and posture changes. After a few weeks, the same symptoms developed on the right side as well. Because mine is a solo practice, I tried to continue seeing patients despite my extreme discomfort and the intermittent numbness of my hands. I eventually went for an MRI, which showed severe spinal stenosis and disc herniation in my C5-C6 and C6-C7 discs.
Surgery was recommended, but I hesitated to proceed. I tried instead to work through the pain, but after 4 months without improvement—with symptoms worsening instead—I decided to undergo spinal fusion surgery. I was terrified.
My outcome was excellent, and because I am healthy and fit I was able to achieve fusion much faster than most people do (Figure 5). I was also fortunate to have one of the world’s best cervical spine surgeons perform my surgery. Not everybody is so lucky, and not all spinal fusion surgery outcomes are so positive. A far better situation is never to require surgery for an occupationally associated MSD; thus I strongly recommend taking steps to optimize ergonomics and posture in the clinic and OR to avoid these occupational strain injuries that can lead to permanent nerve damage.
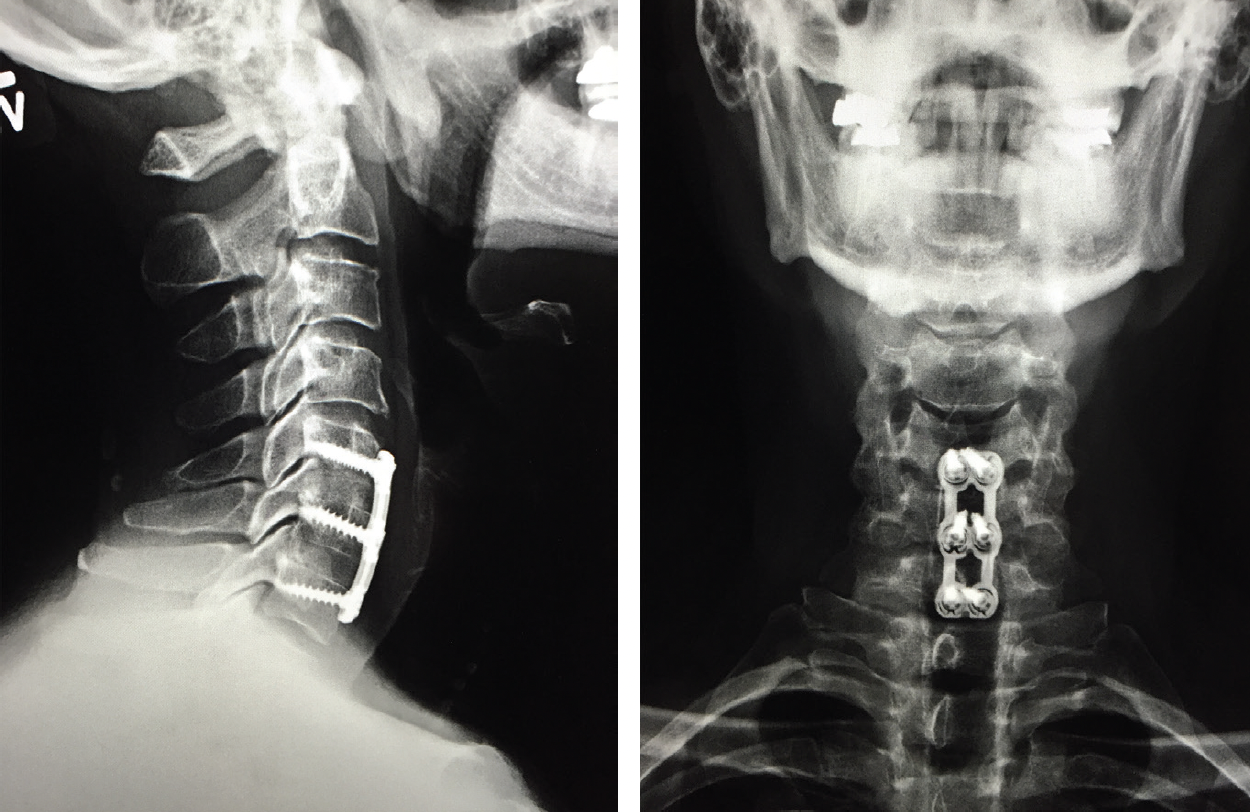
Figure 5. MRIs of Dr. Safran’s spine after his spinal fusion surgery.
MY ERGONOMIC ADJUSTMENTS
During the 4 months I spent trying to avoid surgery, I dedicated a lot of time to figuring out what had caused my neck problem, how to prevent it from worsening, and what I could do to avoid surgery. I discovered that poor posture is almost unavoidable in ophthalmology because of the way some equipment is designed and used. The ramifications, as in my case, can be severe.
Shorter slit-lamp table. One of the biggest problems I identified is slit-lamp design. The edge of the slit-lamp table often sticks out farther than the oculars, so the only way we ophthalmologists can look through the oculars is by craning our neck forward. This not only puts excessive strain on our neck, but it also affects our breathing.1 A forward head position is associated with dysfunctional shallow breathing with the upper thorax rather than the diaphragm. This can lead to hypocapnia that in turn causes decreased blood flow to the brain, respiratory alkalosis, and a shift of free calcium in the blood to bind with available negative charges on albumin due to the change in pH. Lower serum calcium levels can cause increased neuromuscular excitability, anxiety, paresthesias, and muscle cramps—not ideal for a surgeon.2-4
To reduce my head-forward posture at the slit lamp, I worked with a cabinet maker to make custom slit-lamp tables that are 1.5 inches shorter. The idea was to make the end of the slit lamp table facing me flush with the oculars so I would no longer have to crane my neck forward to look through them. We went through many prototypes until we had a design that allowed me to sit with correct posture, rest my arms on the table, and look through the oculars without craning my neck forward (Figure 6).

Figure 6. Dr. Safran’s custom slit-lamp table. The oculars are flush with the end of the table.
Figures 5 and 6 courtesy of Steven G. Safran, MD
Longer head straps. Another modification I made to the slit lamp is to use slightly longer head straps. This allows the patient to move farther forward and decreases the forward movement required of me to examine the patient. This modification allows the patient to get about 0.5 inches closer to me. When that is added to the 1.5 inches that we took off the end of the slit-lamp table, it’s a total of 2 inches less that I must crane my neck forward with every patient.
Optimized posture. I also made a conscious effort to optimize my seated posture when examining patients and operating. This involves sitting with my lower back slightly concave (arched forward), my shoulders back (without my leaning backward), my ears positioned in line with and over my shoulders, and my knees angled downward. This is basically a classic chair meditation pose, and I found that programming myself to assume this posture through actual meditation sessions three to four times a week made it easier for me to assume this posture in the clinic without thinking about it. This posture places the head in line with the spine over the shoulders instead of forward, reducing the problems associated with head-forward posture.
CONCLUSION
Adopting good posture and using ergonomically designed or modified equipment can help avoid the muscle strains, spasms, and MSDs that many of us and other medical professionals are prone to.5 It is important not to wait until something hurts to start paying attention to ergonomics in the clinic and OR. By then, it may be too late.
1. Koseki T, Kakizaki F, Hayashi S, Nishida N, Itoh M. Effect of forward head posture on thoracic shape and respiratory function. J Phys Ther Sci. 2019;31(1):63-68.
2. Bradley H, Esformes J. Breathing pattern disorders and functional movement. Int J Sports Phys Ther. 2014;9(1):28-39.
3. Kahlae AH, Ghamkhar L, Arab AM. The association between neck pain and pulmonary function: a systematic review. Am J Phys Med Rehabil. 2017;96(3):203-210.
4. Dimitriadis Z, Kapreli E, Strimpakos N, Oldham J. Hypocapnia in patients with chronic neck pain: association with pain, muscle function, and psychologic states. Am J Phys Med Rehabil. 2013;92(9):746-754.
5. Kitzman AS, Fethke NB, Baratz KH, Zimmerman MB, Hackbarth DJ, Gehrs KM. A survey study of musculoskeletal disorders among eye care physicians compared with family medicine physicians. Ophthalmology. 2012;119(2):213-220.




