
A proactive approach to dry eye disease (DED) is essential in modern ophthalmology and optometry practices. Fortunately, eye care is experiencing a rapid expansion of ocular surface disease (OSD) services.
A dry eye center cannot be built overnight—at least mine wasn’t—but the rewards can be well worth the effort in terms of the improvements in patients’ quality of life and the fiscal well-being of the practice.
FIRST THINGS FIRST
DED is relatively high maintenance, chronic, and progressive. The foundation of a successful dry eye center is a genuine interest in treating patients with this disease.
The release of the first presbyopia- and astigmatism-correcting IOLs prompted my initial interest in OSD. I realized that keratometry readings and topographic maps might not be reliable if the tear film were unstable and that this could lead to inaccurate IOL power calculations. I became inspired to offer OSD services, and I recognized that success in this area would require a dedicated team.
I believe that a successful dry eye center at most practices requires the efforts of at least one physician and at least one technician. To encourage internal referrals, however, everyone at the practice should understand the OSD services offered. An office manager or lead technician can spearhead training for technicians and the front-office staff who answer incoming calls. Depending on the size of the practice, it may be helpful to enlist additional doctors for specific, dedicated services.
In terms of equipment, a basic DED service requires only a slit lamp and fluorescein and lissamine green vital dyes. The results of these tests and answers to a dry eye questionnaire such as the Ocular Surface Disease Index, Standard Patient Evaluation of Eye Dryness, or Symptom Assessment in Dry Eye can indicate how many of the practice’s existing patients have DED. Building a dry eye center starts from this point.
DIAGNOSIS
Efficiency. A common perception among providers is that offering DED services slows patient flow and impedes physician efficiency. I, however, would argue that DED is like other specialties within ophthalmology. Specific testing is required for DED management just as visual field testing, OCT imaging, and gonioscopy are required for glaucoma management and pupillary dilation, scleral depression, fluorescein angiography, and macular OCT are required for retinal care. Not every test associated with glaucoma or retinal pathology is performed during a single visit, and a similar approach can be taken to DED management. OSD testing may be performed in a stepwise manner and repeated as appropriate to document the effect of treatment, patient compliance, and disease progression.
The workups for DED and glaucoma have similarities. Both require a thorough history and a review of systemic medications. To save time in the clinic, patients can be asked to complete the DED questionnaire of choice at their convenience in advance of their visit.
Tests. In addition to vital dyes, point-of-care tests such as InflammaDry (Quidel) and the TearLab Osmolarity System (TearLab) have become indispensable in my practice. I find meibography helpful for explaining OSD to patients. For example, I use information from the LipiScan dynamic meibomian imager or the LipiView II interferometer (both from Johnson & Johnson Vision) to educate patients about the structural abnormalities of their meibomian glands. It is often by viewing these black-and-white images that patients begin to associate DED with their symptoms.
TREATMENT
DED treatment may be performed in the office and at home, but I find that a combination of the two typically delivers the most effective results.
In-office treatment. The three types of in-office treatment are heating and evacuation, intense pulsed light (IPL), and microblepharoexfoliation. All involve an out-of-pocket expense for patients. My patients have embraced these services, and their level of satisfaction with the results is high.
In my opinion, mechanical and manual expression of the meibomian glands after heating of the meibum is far more comfortable for patients than manual gland expression without prior thermal treatment. Several devices use thermal energy to liquefy impacted meibum and relieve clogged glands such as the LipiFlow Thermal Pulsation System (Johnson & Johnson Vision), iLux (Alcon), and TearCare system (Sight Sciences). Each device has its benefits, including the following:
- Patients who are claustrophobic may prefer an open-eye treatment such as TearCare;
- Individuals with tight lids or small interpalpebral fissures may benefit from treatment with the iLux; and
- Those who prefer an automated approach with uniform thermal pulsation may be best served by the LipiFlow.
IPL reduces inflammation by treating lid telangiectasia. When the correct wavelength is applied, this procedure helps close off abnormal blood vessels that may be leaking proinflammatory mediators. Patients typically begin with four IPL treatments scheduled approximately 2 weeks apart. Thereafter, one treatment performed every 6 months is recommended for maintenance. I often perform thermal treatment with gland evacuation and IPL in a sequential manner.
BlephEx (Alcon) can remove scurf and biofilm that may be blocking the meibomian gland orifices. Performing microblepharoexfoliation before thermal pulsation and IPL can make both of these procedures more effective. Some patients, however, choose to undergo microblepharoexfoliation as a standalone treatment. I find that microblepharoexfoliation appeals particularly to patients who prioritize good lid hygiene.
At-home treatment. Not only can DED treatment at home complement in-office procedures, but it may potentiate their effect.
Artificial tears alone cannot eliminate ocular surface inflammation. Practitioners who wish to specialize in DED management must develop a strong understanding of the drugs available. The objective is to tailor treatment to the presentation. This has become easier to achieve thanks to a growing roster of FDA-approved medications (Table).
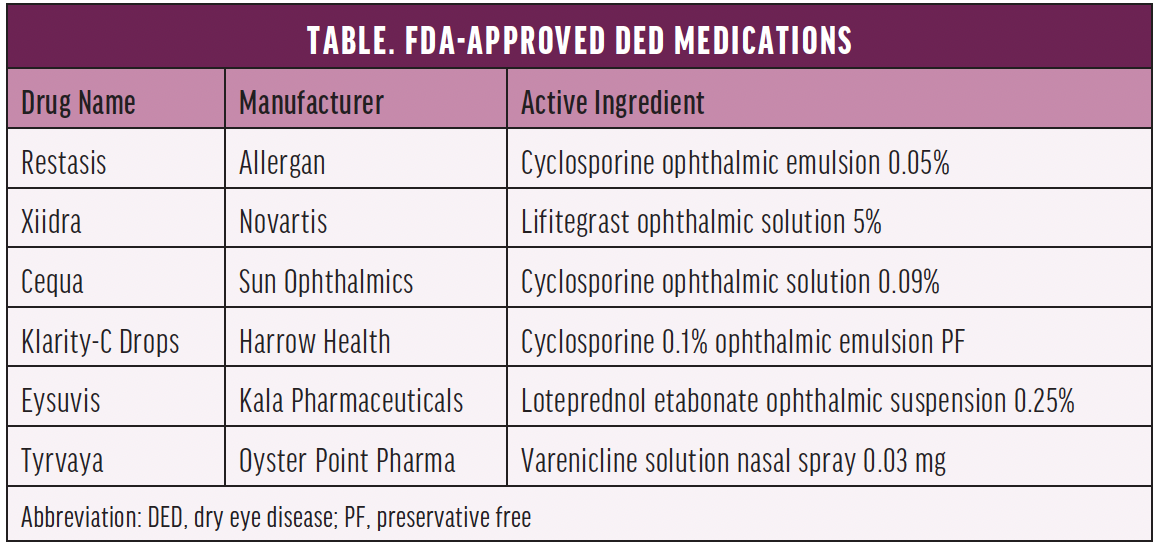
In mid-October, Oyster Point Pharma received FDA approval of varenicline solution nasal spray 0.03 mg (Tyrvaya) for the treatment of the signs and symptoms of DED. The parasympathetic nervous system controls tear film homeostasis partially via the trigeminal nerve, which is accessible within the nose. This novel nasal spray uses the parasympathetic nervous system to promote natural tear film production to reestablish tear film homeostasis.
Many nonpharmaceutical DED treatment options are available for use at home such as heated moisture masks (Bruder Healthcare), lid wipes and sprays, foam cleansers, and mechanical lid brushes (NuLids, NuSight Medical). Oral omega supplements (Physician Recommended Nutraceuticals and ScienceBased Health) can be prescribed to support the health of the meibomian glands and lipid layer. Another prescription treatment option is the iTear 100 (Olympic Ophthalmics), which is designed to stimulate tears through a vibratory approach when the device is applied externally to the side of the nose.
REVENUE
Patients with DED visit their eye doctor multiple times per year according to the severity of their disease. These visits are billed to the insurance carrier. Several diagnostic tests recommended for monitoring DED are also billed to insurance.
Because patients often become confused about which over-the-counter products to purchase at their neighborhood pharmacy, many dry eye centers make these products available for purchase onsite. This is a convenience for patients, and it helps to ensure proper product selection. Other at-home remedies can also be dispensed at the office, which can increase the practice’s overall revenue stream. (For more on this topic, see “Selling Cash-Pay Health Products in the Office.”)
The in-office procedures mentioned in this article are paid for mostly out of pocket by patients. Many patients undergo these treatments annually, semiannually, or more often depending on disease severity. Offering these services can therefore boost a practice’s bottom line.
Cultivating an OSD service can benefit patients and the practice.




