
In the US alone, the total burden forecast for persons with visual impairments due to primary open-angle glaucoma is estimated to be more than 7 million by the year 2050.1 The overarching goal of all glaucoma interventions (surgical and medical) is to reduce IOP, prevent progressive ocular nerve damage, and alleviate the burden of multiple medications used to treat glaucoma.
Microinvasive Glaucoma Surgery
Over the last decade several novel surgical treatment options and devices for glaucoma have been developed. The term microinvasive glaucoma surgery (MIGS) was used for summarizing some of these new procedures.2
By definition, MIGS should require a small, sutureless, self-sealing incision that can be performed under topical anesthesia. The procedure should add minimal to no intraoperative or postoperative complications, including minimal impact to the patient’s postoperative lifestyle such as secondary surgical interventions (Figure 1).

Figure 1. iStent inject (Glaukos).
Targeting IOP
In mild glaucoma the initial target IOP range is often a 20% or more reduction in IOP with a target in the 19 to 21 mm Hg range. For moderate glaucoma, a lower IOP may be necessary such as 16 to 18 mm Hg. In the severe stage of glaucomatous damage we may target 13 to 15 or even 10 to 12 mm Hg.3 Lowering the IOP by 1 mm Hg reduces the risk of progressive field loss by 10%.4 A typical patient off all medications who has field damage due to glaucoma has a wash-out average IOP of 25 to 26 mm Hg. This is where we start.
Medication burden is an area that is often underestimated when it comes to impact on patient lifestyle. Studies have demonstrated as medication requirements increase, patient compliance decreases. In fact, once a patient reaches a fourth medication, the compliance rate goes to nearly zero.5 If we can get a patient off even one medication, or better yet, down to a single medication per day, for me, that is a success.
The iStent inject Procedure: A Complement to Cataract Surgery
Cataract surgery is one of the most opportunistic times we have to help a glaucoma patient. In the US alone, it is estimated as many as 20% of patients undergoing cataract surgery also have glaucoma. From a surgical perspective, we are already there making a small, self-sealing incision under local anesthesia to remove the cataract. We know that cataract surgery alone helps control glaucoma by lowering IOP and reduces the number of needed long-term medications, but what if we could do better? The patient is on the table, prepped, and draped; we are right there in the surgical area with the ability to use the same incision creating the perfect opportunity to add a MIGS procedure such as the iStent inject by Glaukos. iStent inject is the smallest known medical device to be implanted in the human body and is implanted in the trabecular meshwork (TM) (Figure 2). It is designed to work continuously, restoring natural physiologic outflow while minimizing unnecessary disruption to the eye’s natural anatomy.

Figure 2. iStent inject size comparison.
In the typical patient who sees a comprehensive ophthalmologist with cataracts and glaucoma, we want a solution that is microinvasive and does not increase the complication risk to the cataract surgery. The iStent inject pivotal trial demonstrated an overall safety profile that was similar to cataract surgery alone.6 That is not to say there haven’t been some complications reported with the iStent inject; it is possible for patients to have minor complications such as a small transient microhyphema or transient postoperative pressure elevation. But if you look at the multisite clinical trial with surgeons in the early learning curve stage, it showed tremendous efficacy and results with minimal adverse events.6 In addition, many other studies have confirmed the exceptional efficacy and safety profile of the iStent inject in patients with primary open-angle glaucoma. Postoperative complications noted with other trabecular devices such as peripheral anterior synechiae are minimized with the iStent inject.
For the patient, there is no additional pain involved with the procedure, no additional sedation, and the postoperative management remains unchanged. This procedure can be life-changing for patients and in my hands, iStent inject complements cataract surgery beautifully.
Is a Bigger or Smaller Device Better? An Industry Debate
The largest glaucoma drainage device that we use is the Baerveldt glaucoma implant (Johnson & Johnson Vision), and that is arguably also the most invasive glaucoma procedure we do. Just because a device is bigger does not necessarily mean it is better, especially in the delicate trabecular outflow pathway. I prefer to think of this debate as not being about the size of the implant as much as the combination of safety and efficacy—meaning how much pressure reduction we are able to achieve—and the safety and ease of the intraoperative surgery, the complication rate both intraoperatively and postoperatively, and a hassle-free postoperative course for the patient and surgeon.
The first-generation iStent is a very small device that increases the facility of outflow with even a single implant. The second-generation iStent inject uses two implants (Figure 3), which studies have shown provides increased efficacy and procedural elegance over a single stent.7
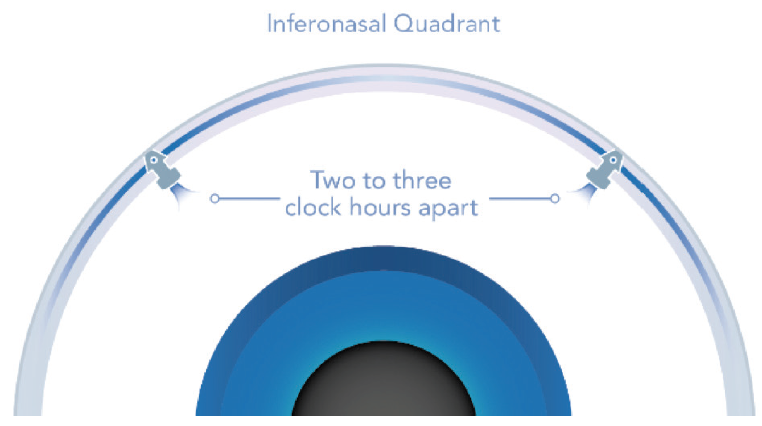
Figure 3. iStent inject device size with two stents 2 to 3 clock hours apart.
Conclusion
We all want to achieve the best and safest possible outcome to reduce IOP and the burden of multiple medications. For my patients, the iStent inject offers the best combination of features in a MIGS device, and it remains my preference. When I speak with a patient planning cataract surgery and they are on glaucoma medications already for IOP, I always offer the iStent inject as part of their cataract surgical care plan to lower IOP, reduce the risk of long-term progressive damage, and potentially reduce their medication burden.
1. American Academy of Ophthalmology. US eye disease statistics. American Academy of Ophthalmology. Available at: https://www.aao.org/eye-disease-statistics. Accessed July 24, 2019.
2. Pillunat LE, Erb C, Jünemann AG, et al. Microinvasive glaucoma surgery (MIGS): a review of surgical procedures using stents. Clin Ophthalmol. 2017;11:1583-1600.
3. Sihota R, Angmo D, Ramaswamy D, et al. Simplifying “target” intraocular pressure for different stages of primary open-angle glaucoma and primary angle-closure glaucoma. Indian J Ophthalmol. 2018;66(4):495-505.
4. Heijl A, Leske MC, Bengtsson B, et al. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2002;120(10):1268-1279.
5. Robin A, Grover DS. Compliance and adherence in glaucoma management. Indian J Ophthalmol. 2011;59: S93-S96.
6. Samuelson TW, Sarkisian SR, Lubeck DM, et al. Prospective, randomized, controlled pivotal trial of an ab interno implanted trabecular micro-bypass in primary open-angle glaucoma and cataract. Ophthalmology. 2019;126(6):811-821.
7. Guedes RAP, Gravina DM, Lake JC, et al. Intermediate results of iStent or iStent inject implantation combined with cataract surgery in a real-world setting: a longitudinal retrospective study. Ophthalmol Ther. 2019;8(1):87-100.
