
A 35-year-old man from a neighboring state was referred for a corneal consultation, approximately 4 years after experiencing an explosion during firearm discharge. He reported that brass and steel fragments as well as gunpowder deposits made impact with his eyes and face. Since the incident, his vision had progressively worsened.
The patient noted that shifting his gaze away from central fixation occasionally enhanced image clarity. Spectacles and contact lenses produced no significant improvement in his visual function.
CLINICAL EXAMINATION AND FINDINGS
Upon examination, the patient’s BCVA was 20/20- OD with a refraction of -0.75 +0.50 x 140º and 20/25 OS with a refraction of -0.25 +0.25 x 160º. The IOP in each eye was within a normal range.
A slit-lamp examination of the right eye revealed a black foreign body in the medial conjunctiva near the limbus (Figure 1). The cornea exhibited multiple scars from foreign bodies, corneal bronzing, and sparkling copper-colored guttae in the central area (Figures 2 and 3). The iris displayed greenish-brown discoloration (Figure 1), and the crystalline lens showed mild yellowing (Figure 4). A dilated fundus examination of the right eye was normal.
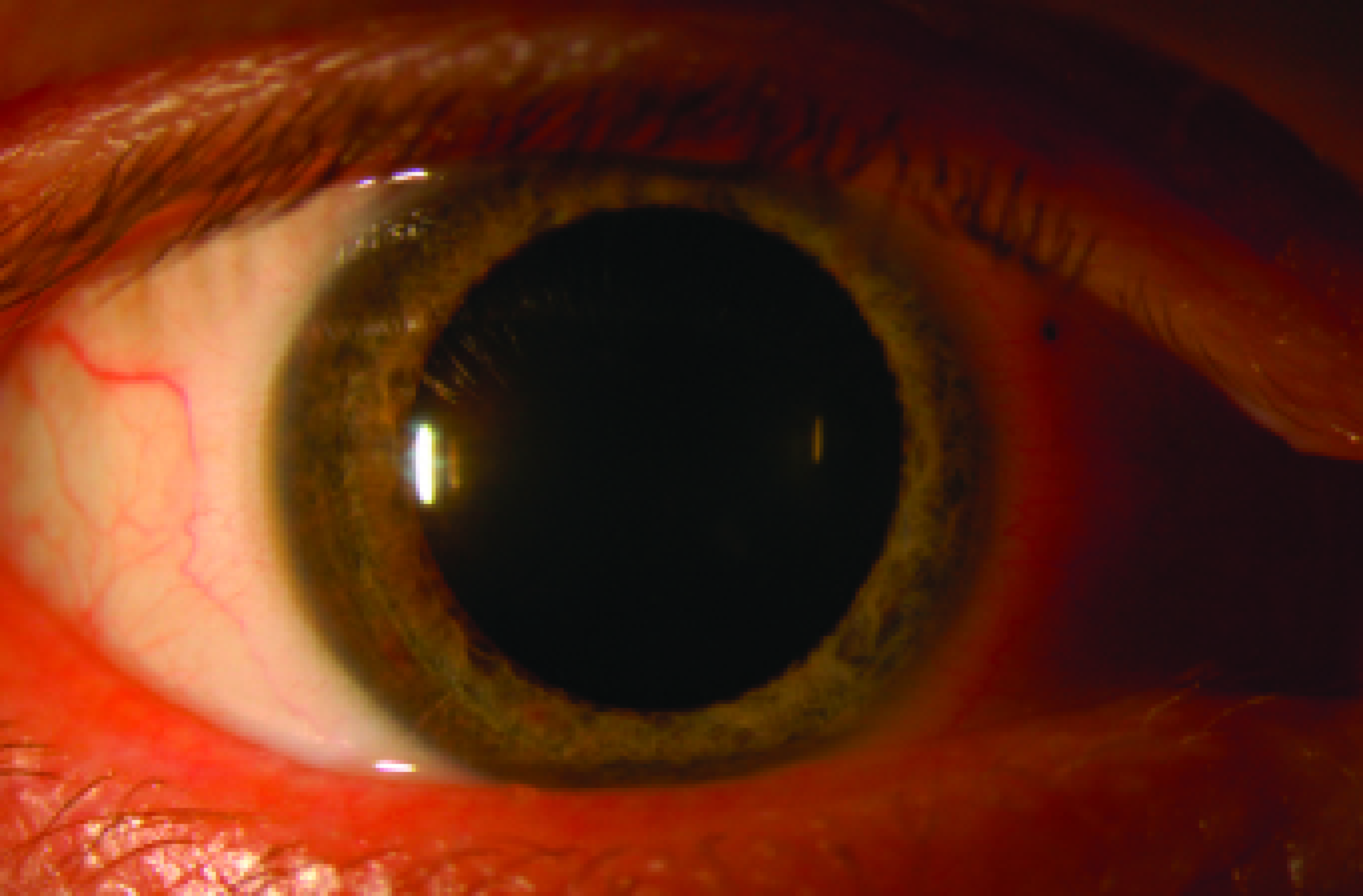
Figure 1. Black IOFB, likely gunpowder residue, is embedded in the conjunctiva of the right eye. Greenish-brown discoloration is observed in the right iris.
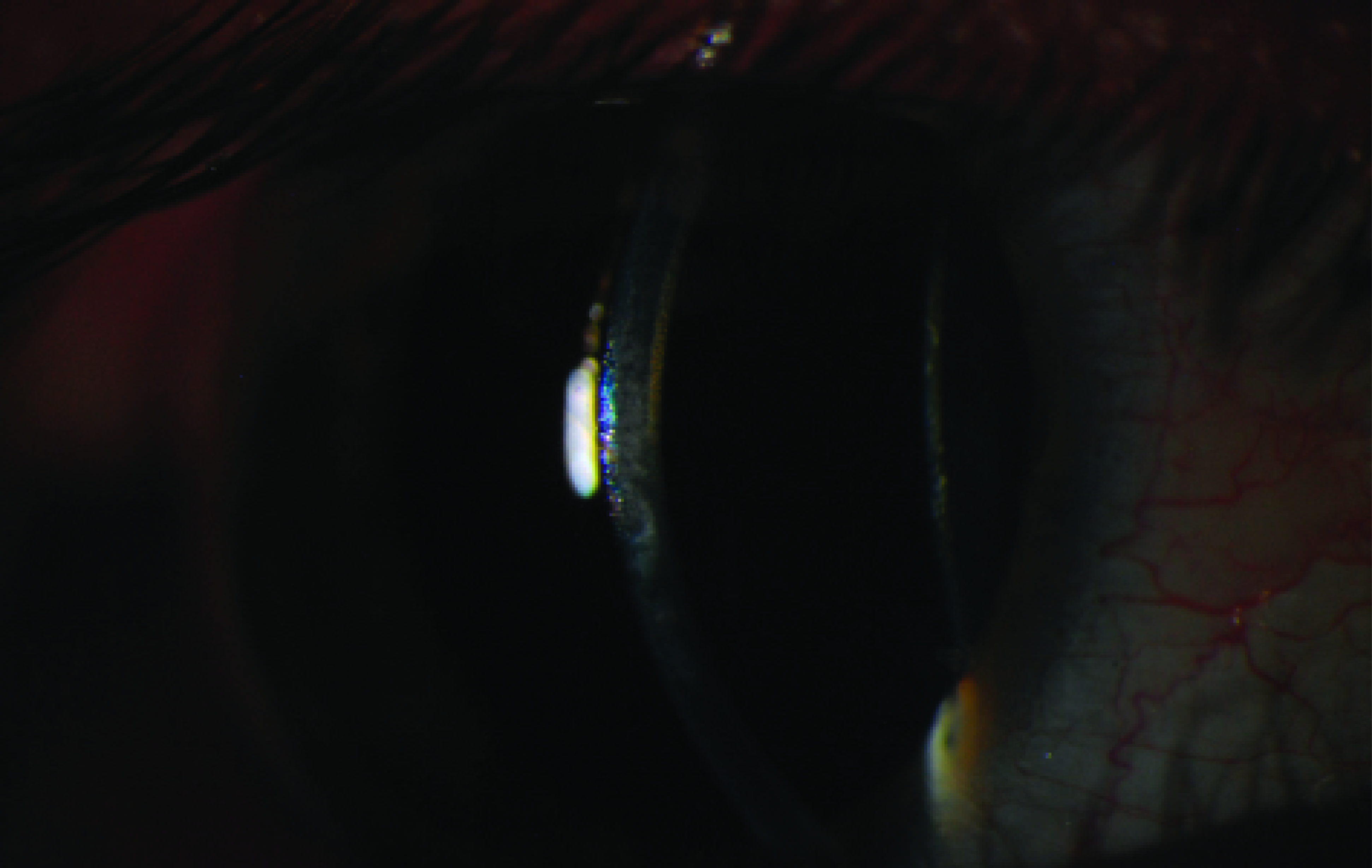
Figure 2. Multiple scars from IOFBs are present in the right cornea.

Figure 3. Sparkling, copper-colored guttae are evident in the right cornea.
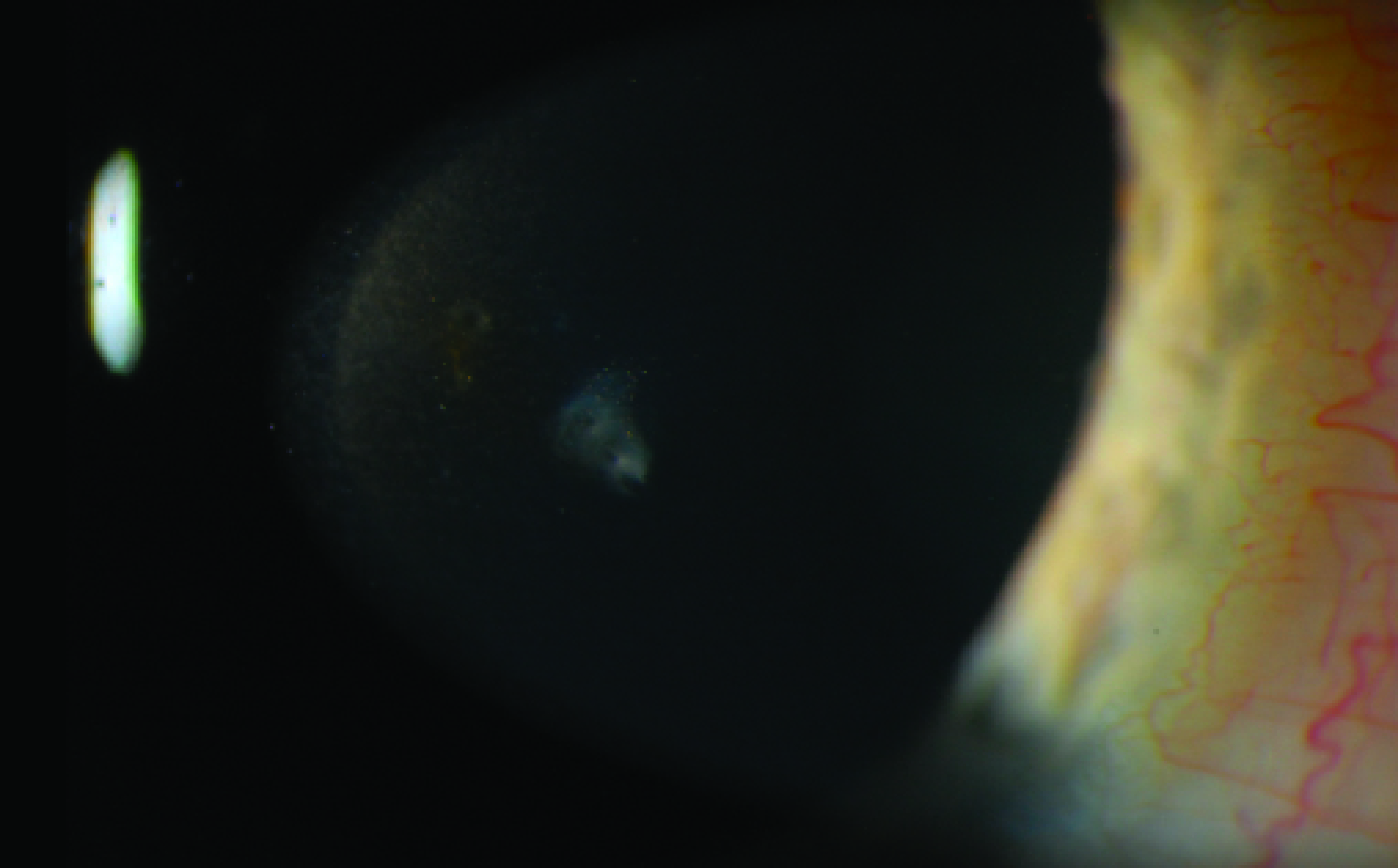
Figure 4. Yellowing is observed in the right lens.
A slit-lamp examination of the left eye revealed multiple scars from coppery-looking foreign bodies embedded deep in the cornea (Figures 5 and 6), mild corneal bronzing, and no endothelial changes. A dilated fundus examination was normal.
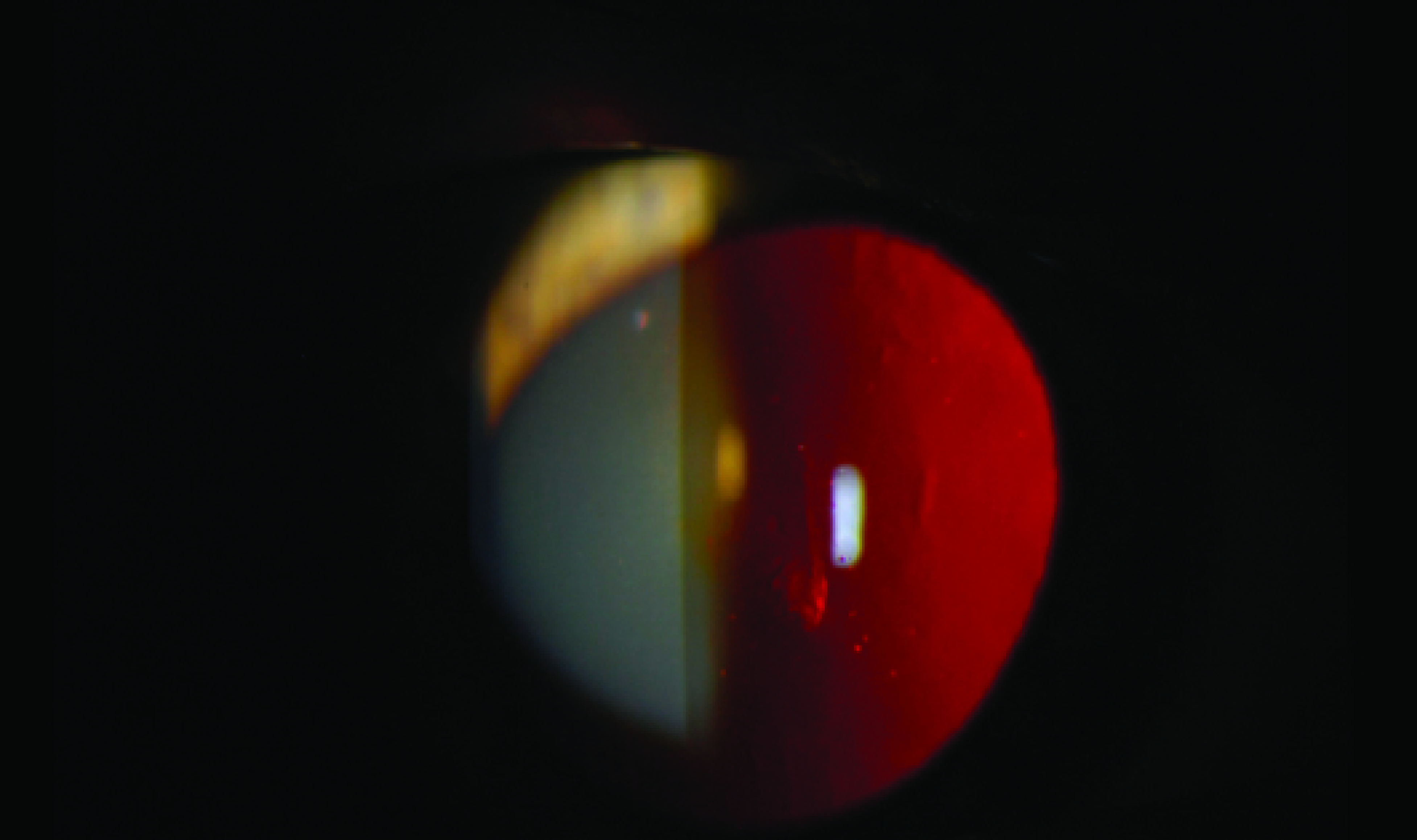
Figure 5. Copper-colored IOFBs are embedded in the left cornea.

Figure 6. A slit-lamp examination reveals shimmering, copper-colored IOFBs in the left cornea.
Courtesy of James Gilman, CRA, FOPS
Specular microscopy indicated a significant reduction in endothelial cell count in the right eye only.
DISCUSSION
A bullet consists of a casing, a primer, gunpowder, and a projectile. The casing, which holds the ammunition components together, is typically made of brass, steel, copper, paper, or plastic.1 Brass is an alloy composed primarily of copper and zinc, whereas steel consists largely of iron.
Chalcosis is a chronic reaction to a copper-containing intraocular foreign body (IOFB). Alloys containing more than 85% copper can cause acute chalcosis,2 severe inflammation, and potentially grave complications such as suppurative endophthalmitis and phthisis bulbi. Prompt removal of the IOFBs is essential to prevent these outcomes.1,2
IOFBs containing less than 85% copper, such as brass and bronze, tend to cause chronic chalcosis. They result in classic ocular findings over time, such as a Kayser-Fleischer ring, a golden-brown metallic sheen on the cornea, guttae on the corneal endothelium, metallic aqueous particles, a greenish tinge to the iris, a sunflower cataract, a dull yellow glow over the anterior capsule of the lens, brown vitreous opacities, and metallic flecks on retinal vessels and the internal limiting membrane.2 If the IOFB is not removed, fibrosis may encapsulate the copper, reducing its spread to adjacent tissues. Most published studies discuss chalcosis in the context of open globe injuries with posterior involvement, where removal is often performed via a pars plana vitrectomy.3,4 Even in cases of corneal chalcosis, however, where patients may remain asymptomatic for long periods,5,6 it is crucial to remove the IOFBs to minimize the risk of progressive endothelial damage and further corneal discoloration.5
TREATMENT AND FOLLOW-UP
The IOFBs were removed from the conjunctiva and cornea with a 27-gauge needle. Baseline macular OCT and electroretinography assessments were performed. We advised the patient that an endothelial keratoplasty might be required in the future for his right eye, given the significant endothelial loss observed at presentation. At his 6-month follow-up visit, the patient’s vision, examination results, and cell counts remained stable in both eyes with no further corneal deterioration.
1. Ravani R, Kumar V, Kumar A, Kumar P, Chawla S, Ghosh S. Fleck-like deposits and swept source optical coherence tomography characteristics in a case of confirmed ocular chalcosis. Indian J Ophthalmol. 2018;66(11):1640-1642.
2. American Academy of Ophthalmology. Basic and clinical science course, section 12: retina and vitreous. 2019-2020 ed. American Academy of Ophthalmology; 2019:362.
3. Uplanchiwar B, Ambiya V, Pappuru RR, Jhingan M. Retinal chalcosis. Am J Ophthalmol Case Rep. 2020;20:100937.
4. Agarwal R, Goel Y, Anand K. Sunflower cataract in chalcosis bulbi. Indian J Ophthalmol. 2019;67(1):137-138.
5. Salman A, Erdahl S, Jannetto P, Baratz K. Corneal chalcosis secondary to a brass bullet casing fragment. Am J Ophthalmol Case Rep. 2022;26:101443.
6. Puranik C, Chaurasia S, Ramappa M, Sangwan V, Balasubramanian D. Corneal chalcosis following blast injury. Br J Ophthalmol. 2012;96(5):762.




