Premium Lens Technology Is an Important Part of Any Refractive Cataract Practice
Jorge L. Alió, MD, PhD, FEBOphth
Alicante, Spain

Presbyopia-correcting IOLs are an important part of any refractive cataract surgery practice, including mine. In my routine practice of lens surgery, which includes cataract surgery and refractive lens exchange, I implant a presbyopia-correcting IOL in about 70% of cases.
CURRENT AND POTENTIAL FUTURE PREFERENCES
I participate in many clinical studies of various models and types of multifocal and extended depth of focus (EDOF) lenses,1 and I therefore have my own outcomes for most of the available premium IOLs. I do not offer EDOF IOLs, with the exceptions of the Tecnis Eyhance (Johnson & Johnson Vision) and AcrySof IQ Vivity (Alcon) in my private practice because I have found that many so-called EDOF IOLs provide poor near vision and an inadequate quality of vision. My multifocal IOL preferences outside of clinical investigations are the diffractive AT LISA tri (Carl Zeiss Meditec) and the refractive Acunex Vario (Teleon Surgical) with a near vision add of +1.50 D and a new IOL hydrophobic material. I also frequently use the RayOne Trifocal (Rayner), FineVision (PhysIOL), and Intensity (Hanita).1
In the near future, my preference will become accommodating IOLs, as the Lumina (Akkolens International), implanted in the sulcus,2,3 will be the first accommodating IOL to truly work as designed. I was the investigator in the preliminary phase 1 and 2 studies and am currently the clinical director and one of the investigators in the phase 3 multicenter study in Spain and Colombia. Results to date have been impressive, and I look forward to using this lens in clinical practice once it has the CE Mark—to clarify, I am particularly interested in a group of lenses sometimes referred to as monofocal plus.
I am impressed by the results achieved with the Tecnis Eyhance in my independent clinical study. I am even more impressed by the superior near vision outcomes reported with the AcrySof IQ Vivity. I think that, in the future, these lenses will replace most of the monofocal lenses that I currently implant. (Editor’s note: For more on these and other new-technology monofocal IOLs, see the article on pg 24). I see no reason not to use IOLs that provide my patients with better intermediate vision without reducing contrast sensitivity, giving an inadequate quality of vision, or causing unwanted dysphotopsias such as occurs with current EDOF IOLs.4,5
PATIENT SELECTION
Many patients, when properly selected, do well with a multifocal IOL that is chosen to meet their conditions and needs. When I assess patients for cataract surgery, I start by asking myself the following question: “Why should this patient not have a multifocal or EDOF lens?” My first choice is always to consider a multifocal IOL for every patient.
I do not, however, implant presbyopia-correcting lenses in patients with maculopathy or poor macular function, retinal dystrophy, optic atrophy, and moderate to advanced glaucoma because the benefits of using a multifocal lens do not outweigh its cost for these patients.
When I implant multifocal and other presbyopia-correcting IOL designs, I use a capsular tension ring to guarantee centration and stability. I am also impressed with the CapsuLaser (Excel-Lens), which I routinely use in these cases to make a perfect capsulotomy. This device is much more cost-effective than a femtosecond laser, a technology I abandoned for cataract surgery due to its poor cost-effectiveness.
CONCLUSION
I forsee a new category of monofocal IOLs: monofocal plus IOLs, which actually is a new type of EDOF lens. (I am currently developing a classification for monofocal+ lenses, as there is confusion surrounding this topic.)
I also plan on integrating the Lumina into my armamentarium as soon as it becomes commercially available. If real accommodation can be achieved by this IOL, the approach of multifocality will be abandoned in clinical practice.
1. Alió JL, Pikkel J. Multifocal Intraocular Lenses: The Art and the Practice. Springer; 2014.
2. Alió JL, Simonov A, Plaza-Puche AB, et al. Visual outcomes and accommodative response of the Lumina accommodative intraocular lens. Am J Ophthalmol. 2016;164:37-48.
3. Alió JL, Simonov AN, Romero D, et al. Analysis of accommodative performance of a new accommodative intraocular lens. J Refract Surg. 2018;34(2):78-83.
4. Alió JL. Presbyopic lenses: evidence, masquerade news, and fake news. Asia Pac J Ophthalmol. 2019;8(4):273-274.
5. Kanclerz P, Toto F, Grzybowski A, Alió JL. Extended depth-of-field intraocular lenses: an update. Asia Pac J Ophthalmol. 2020;9(3):194-202.
Patients Want a Lens That Will Decrease Their Spectacle Dependence
Ashraf Armia Balamoun, MD, MSc, FRCS (Glasg), FACS
Cairo, Egypt

Over the 20 years I have been practicing ophthalmology, the expectations and needs of patients have changed. Today, patients who undergo cataract surgery expect spectacle independence. In my experience, some IOLs accomplish this goal better than others. Herein, I share my preferred lens technologies and discuss the technologies I am most excited to try next.
More than 70% of my patients receive some form of astigmatism correction. I typically use limbal relaxing incisions for eyes with less than 1.00 D of astigmatism, and I use either the AcrySof IQ Toric SN60T3 to SN60T9 IOLs (Alcon) or the Tecnis Toric IOL (Johnson & Johnson Vision) for eyes with more than 1.00 D of astigmatism. In eyes with regular corneal astigmatism, a toric IOL provides better distance UCVA, greater spectacle independence, and lower amounts of residual astigmatism compared with a nontoric IOL paired to limbal relaxing incisions. Postoperative astigmatism of 0.50 D or less is associated with improved visual function and increased patient satisfaction due to greater spectacle independence and a decreased need for a refractive enhancement.
Dr. Armia provides tips for intraoperative maneuvers with premium trifocal IOLs and showcases some of the tools he uses.
PREMIUM IOLS
I use multifocal and EDOF IOLs (Figure 1) in approximately 20% of my patients. I always ask patients about their work and recreational activities to get as complete a picture as possible of their predominant visual needs. For example, if manual labor or computer work is an integral part of a patient’s lifestyle, good intermediate vision is a priority with a multifocal IOL. If spectacle-free reading ability is strongly desired, a multifocal IOL with a corresponding near addition may be the best choice. If both distances are used equally, a trifocal IOL would be suitable. I always consider the defocus curves of various IOLs when deciding which one to recommend.
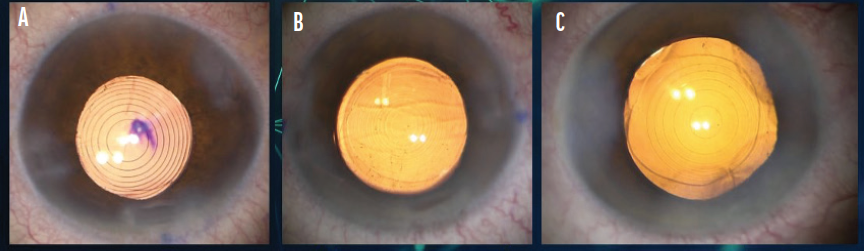
Figure 1. The Tecnis Symfony (A), FineVision (B), and AcrySof IQ PanOptix (C) IOLs in situ.
I like to use EDOF IOLs with a refractive segmental design such as the Tecnis Symfony (Johnson & Johnson Vision), and I use a blended vision strategy by targeting emmetropia in the dominant eye and -1.50 D in the nondominant eye. Patients with this form of blended vision generally achieve spectacle independence except for reading small print.1,2 Recently released diffractive lenses may perform better than refractive lenses in terms of near vision and quality of vision. Likewise, there seems to be less risk of halos with the latest premium IOL technologies compared with older diffractive and refractive lenses.
I find that the AcrySof IQ PanOptix (Alcon) and FineVision3 IOLs provide the best outcomes when the treatment plan takes into account preoperative diagnostics such as corneal topography, OCT of the macula, dry eye evaluation, and biometry measurements (Figure 2).4 I also use the Tecnis Eyhance. With this IOL, I target the dominant eye for distance and intermediate vision and the nondominant eye for less intermediate and more near vision.5 Regardless of the chosen IOL and strategy, I always compare two IOL power calculation formulas to ensure the best outcomes.
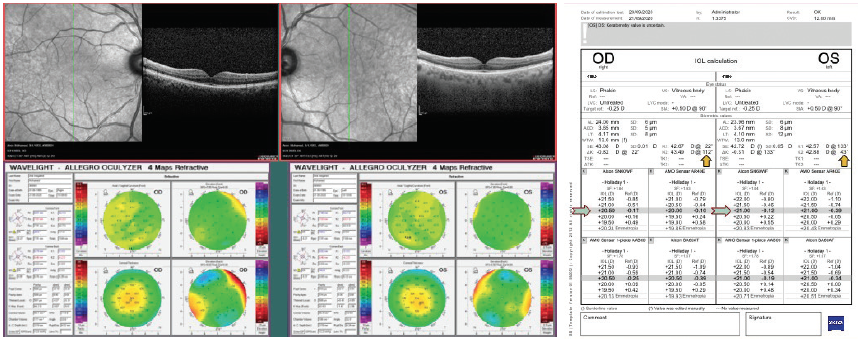
Figure 2. Measurements and IOL power calculation for an eye implanted with the AcrySof IQ PanOptix IOL.
Figures 1 and 2 courtesy of Ashraf Armia Balamoun, MD, MSc, FRCS (Glasg), FACS
FUTURE OUTLOOK
I am waiting for the Vivity, the IsoPure and Triumf EDOF IOLs (both from FineVision), and the Tecnis Synergy (Johnson & Johnson Vision) to become available in Egypt, where I practice.
1. Nivean M, Nivean PD, Reddy JK, et al. Performance of a new-generation extended depth of focus intraocular lens—a prospective comparative study. Asia Pac J Ophthalmol. 2019;8:285-289..
2. Kessel L, Andresen J, Tendal B, et al. Toric intraocular lenses in the correction of astigmatism during cataract surgery: a systematic review and meta-analysis. Ophthalmology. 2016;123:275-286.
3. Sigireddi RR, Weikert MP. How much astigmatism to treat in cataract surgery. Curr Opin Ophthalmol. 2020;31:10-14.
4. Cochener B, Boutillier G, Lamard M, Auberger-Zagnoli C. A comparative evaluation of a new generation of diffractive trifocal and extended depth of focus intraocular lenses. J Refract Surg. 2018;34(8):507-514.
5. Breyer DRH, Kaymak H, Ax T, Kretz FTA, Auffarth GU, Hagen PR. Multifocal intraocular lenses and extended depth of focus intraocular lenses. Asia-Pac J Ophthalmol. 2017;6:339-349.
Determine the Value of the IOL for Each Patient
Francesco Carones, MD
Milan, Italy

Almost all patients can take advantage of presbyopia-correcting IOLs. It is just a matter of understanding what the best technology is for each of them.
CATEGORIES
The broad availability of IOLs that perform differently allows surgeons to customize visual results to each patient’s needs at the time of cataract surgery or refractive lens exchange. The main parameters to consider when counseling patients are spectacle independence and dysphotopsias.
When considering the former, there are at least four IOL categories, listed here in order of increasing performance:
- Standard monofocal;
- EDOF monofocal;
- Partial range-of-distance;
- Presbyopia-correcting IOLs (EDOF technologies); and
- Full range-of-distance presbyopia-correcting IOLs (trifocal and hybrid technologies).
Regarding dysphtopsias, IOLs can be grouped into three categories, listed in order of increasing likelihood of inducing visual disturbances:
- IOLs with a standard aspheric or spheric optic;
- IOLs with a nondiffractive, modified optic; and
- IOLs with a diffractive, modified optic.
At present, an IOL that provides full range-of-distance spectacle independence and has the dysphotopsia profile of a standard aspheric monofocal does not exist.
MY PRACTICE
I am partial to the use of presbyopia-correcting IOLs. Herein I describe why.
Mindset. In my practice, lens replacement is always considered to be a purely refractive procedure regardless of whether a cataract is present. More than 50% of lens replacement procedures are performed solely for refractive purposes. For this reason, presbyopia-correcting IOLs are my standard type of lens implant, and all eyes for which greater than 0.50 D of residual astigmatism is anticipated receive a toric version of the selected lens. Approximately 80% to 85% of the lens procedures performed at my practice involve a presbyopia-correcting IOL, and 50% of all procedures involve a toric lens of some kind. Approximately 10% of eyes receive an EDOF monofocal lens, and less than 5% of eyes receive a standard, nontoric monofocal IOL.
IOL selection. Our counseling process focuses on determining the value of the procedure for each patient. The value represents the difference between the benefits delivered and the patient’s willingness to compromise (ie, having a full range of spectacle independence with some degree of dysphotopsia in dim lighting or enjoying partial range-of-distance spectacle independence with almost uncompromised night vision).
Of the presbyopia-correcting IOLs I implant, 50% are full range-of-distance diffractive lenses (trifocals and hybrid technologies), usually the AcrySof IQ PanOptix and Tecnis Synergy. In my hands, the PanOptix provides a better balance between spectacle independence and dysphotopsia, with slightly weaker performance for reading in dim light. I find that the Synergy provides a superior quality of vision under bright light and better intermediate to near performance in dim light but at the cost of more significant dysphotopsia in dim light.
The remaining 50% of my presbyopia-correcting IOLs are partial range-of-distance (EDOF) nondiffractive lenses—almost exclusively the AcrySof IQ Vivity. This IOL provides most of my patients with spectacle independence (especially using a binocular mini-monovision strategy) with almost no nighttime dysphotopsias.
The EDOF monofocal IOLs I implant routinely are the IsoPure and the Tecnis Eyhance. These lenses are suitable choices when either a presbyopia-correcting IOL is not indicated or the patient is not interested in spectacle independence. Both IOLs provide some degree of useful range of vision, but neither is currently available in a toric version.
THE PIPELINE
I don’t expect revolutionary or game-changing IOL technologies to be released in the near term because most of the presbyopia-correcting IOLs soon to become available will likely fall into the categories described earlier. Currently available lenses deliver solid performance and meet the expectations I set for patients.
Will a true accommodating IOL capable of providing full range-of-distance spectacle independence without compromising quality of vision be a reality in the future? Only time will tell.
High Hopes for Two IOL Technologies in Development
Arturo Chayet, MD
Tijuana, Mexico

I currently use both monofocal and presbyopia-correcting IOLs, and in the future I hope to incorporate the use of two novel lens technologies that are still in development.
Adoption rates. In my practice, the adoption rates of monofocal and presbyopia-correcting IOLs are 60% and 40%, respectively. I do not consider toric IOLs to be premium IOLs. If I categorized them as premium lenses, then the adoption rates for premium and standard IOLs would be 72% and 28%, respectively.
The cost of IOL surgery is the same whether a patient receives a toric or nontoric IOL, whereas the price structures for presbyopia-correcting and monofocal IOLs differ. I use swept-source OCT technology and the ray-tracing software Oculix (Panopsis) that includes total corneal power to target 0.00 to -0.25 D of postoperative with-the-rule astigmatism. With this cost-related strategy, 60% of the IOLs I implant are toric models.
Preferred IOLs. I currently offer patients the AcrySof IQ monofocal IOL (Alcon), AcrySof IOL (model MA60, Alcon), enVista IOL (model MX60, Bausch + Lomb), AcrySof IQ PanOptix trifocal IOL, and Light Adjustable Lens (RxSight). Patient interest in the Light Adjustable Lens has become significant in my practice, so it is currently a key offering in my premium IOL armamentarium.
THE PIPELINE
The first of two IOL technologies in development that are of greatest interest to me is the Juvene IOL (LensGen). It has two components, a capsule-filling base that is implanted in the capsular bag and a fluid-optic lens. By fully filling the bag, the base provides a stable bag-IOL component, and in my experience this decreases the incidence of posterior capsular opacification. The fluid-optic lens is available in both a toric and a nontoric design. It provides distance and near visual acuity by changing curvature (Figure 3).
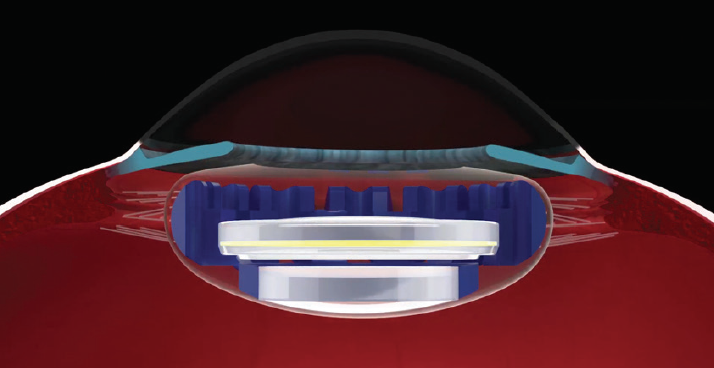
Figure 3. Depiction of the LensGen Juvene capsule-filling IOL in situ.
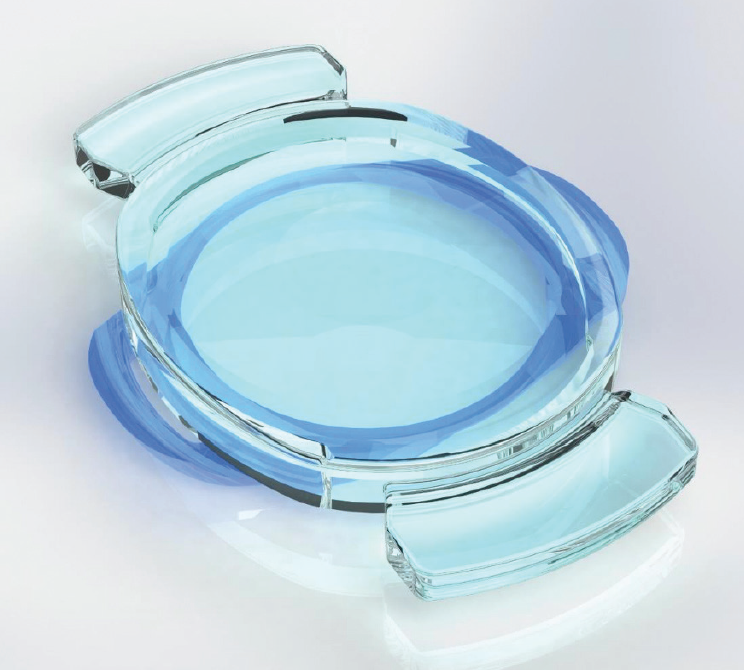
Figure 4. Design of the accommodating Opira AIOL.
Figures 3 and 4 courtesy of Arturo Chayet, MD
The second exciting pipeline technology is another accommodating IOL, the Opira AIOL (ForSight Vision6). This lens has a novel shape-changing mechanism of ciliary body–driven accommodation and capsular bag fixation (Figure 4). The clinical trial results have been impressive. In more than 30 patients, mean monocular corrected distance and intermediate visual acuities was 20/20, and distance-corrected near visual acuity was 20/25. These results have been maintained for 2 years, and safety has been excellent. Thus far in my experience, patients have enjoyed excellent functional vision at all distances without correction.
Monofocal IOLs Still Leading
Bruno M. Fontes, MD, PhD
Rio de Janeiro, Brazil

In my practice in Rio de Janeiro, Brazil, the majority of patients elect an aspheric monofocal IOL. This is largely because of the out-of-pocket costs associated with premium lens technologies. About 75% of patients with more than 1.00 D of astigmatism opt for a toric IOL, and the remaining 25% choose a standard monofocal IOL because of financial reasons. When I am implanting a standard aspheric monofocal, my preferred brands are Alcon, Johnson & Johnson Vision, and Hoya because of their lenses’ known stability in the capsular bag.1-8
Only about 10% to 15% of patients who undergo routine cataract surgery at my clinic elect a presbyopia-correcting IOL. These patients most often receive an AcrySof IQ PanOptix. The Tecnis Synergy is a close second, but because it is not yet available on a toric platform, its indications are limited.
I do not use EDOF IOLs for many patients, but most of those who have received this lens type are happy with their vision postoperatively.
Lastly, I am excited about the upcoming availability of the AcrySof IQ Vivity and Tecnis Eyhance IOLs in my country.
1. Lee BS, Chang DF. Comparison of the rotational stability of two toric intraocular lenses in 1273 consecutive eyes. Ophthalmology. 2018;125(9):1325-1331.
2. Gyöngyössy B, Jirak P, Schönherr U. Long-term rotational stability and visual outcomes of a single-piece hydrophilic acrylic toric IOL: a 1.5-year follow-up. Int J Ophthalmol. 2017;10(4):573-578.
3. Potvin R, Kramer BA, Hardten DR, Berdahl JP. Toric intraocular lens orientation and residual refractive astigmatism: an analysis. Clin Ophthalmol. 2016;10:1829‐1836.
4. Chua WH, Yuen LH, Chua J, Teh G, Hill WE. Matched comparison of rotational stability of 1-piece acrylic and plate-haptic silicone toric intraocular lenses in Asian eyes. J Cataract Refract Surg. 2012;38(4):620-624.
5. Holland E, Lane S, Horn JD, Ernest P, Arleo R, Miller KM. The AcrySof Toric intraocular lens in subjects with cataracts and corneal astigmatism: a randomized, subject-masked, parallel-group, 1-year study. Ophthalmology. 2010;117(11):2104-2111.
6. Kim MH, Chung TY, Chung ES. Long-term efficacy and rotational stability of AcrySof toric intraocular lens implantation in cataract surgery. Korean J Ophthalmol. 2010;24(4):207-212.
7. Zuberbuhler B, Signer T, Gale R, Haefliger E. Rotational stability of the AcrySof SA60TT toric intraocular lenses: a cohort study. BMC Ophthalmol. 2008;8:8.
8. Wirtitsch MG, Findl O, Menapace R, Kriechbaum, et al. Effect of haptic design on change in axial lens position after cataract surgery. J Cataract Refract Surg. 2004;30(1):45-51.
New IOLs Enhance Premium Lens Adoption and Patient Satisfaction
John A. Hovanesian, MD
Laguna Hills, California

The current global pandemic has caused dramatic shifts in how people spend their time, and many eye care practitioners have observed that consumers are more aware than ever of premium IOL technologies. In addition to the premium lens options that have been available for years, many recently FDA-approved IOLs and others in development can provide patients with greater spectacle independence and reduced dysphotopsia. These lenses can also be used in patients with a wide variety of needs and health conditions. Furthermore, recent software advances have helped practices with candidate selection and patient education. Use of this software helped to increase the premium IOL adoption rate at my practice significantly, and I have heard from others that it has increased their comfort with premium IOLs.
EXPANDING INDICATIONS
In the United States, the FDA’s approval of two premium IOLs, the AcrySof IQ Vivity and Tecnis Symfony Plus, and the availability of other select IOLs have expanded the indications for premium IOLs.
Vivity. With a wide, flat defocus curve, Vivity provides consistent distance and intermediate vision when targeted for plano and creates no more glare or other unwanted side effects than a monofocal lens, making it safe for any eye, in my experience. Its defocus curve creates a soft landing spot and forgives some residual refractive error. When used with a mini-monovision strategy, the Vivity lens can provide a full range of vision.
Symfony Plus. This IOL provides greater near vision and reduces glare and halos compared with its predecessor. It may also serve a wider range of patients than previous generations of EDOF IOLs.
enVista. Many clinicians have found that patients obtain a wide range of vision with the monofocal enVista and enVista Toric lenses. The nontoric enVista is not labelled as a premium lens; however, it is a valuable monofocal that, in my opinion, deserves a place in every surgeon’s OR.
LOOKING AHEAD
I look forward to the availability of two lenses specifically in the United States, and I am excited to see how much my premium conversion rates increase with use of a recent software advance.
IC-8. Among lenses that are not yet FDA-approved, the IC-8 small-aperture IOL (AcuFocus) has performed impressively with regard to astigmatism correction in the FDA trial. Internationally, the lens is widely used for patients who have irregular astigmatism and other corneal aberrations. The IC-8 will almost certainly occupy an important place in the US market once it is approved.
Juvene. Another highly anticipated lens is the Juvene IOL, a truly accommodating lens with optics that can be changed out as new technology becomes available.
MDbackline. This web-based software platform educates incoming cataract patients on refractive options and administers a questionnaire that generates a visual profile report (Figure 5) to provide clinicians with a look at the patient’s likelihood of choosing an upgrade. It also details which upgrade options would best suit the patient. Based on complex algorithms, the software’s predictive value has been proven in a number of practices, which have seen two- to threefold increases in premium technology adoption.
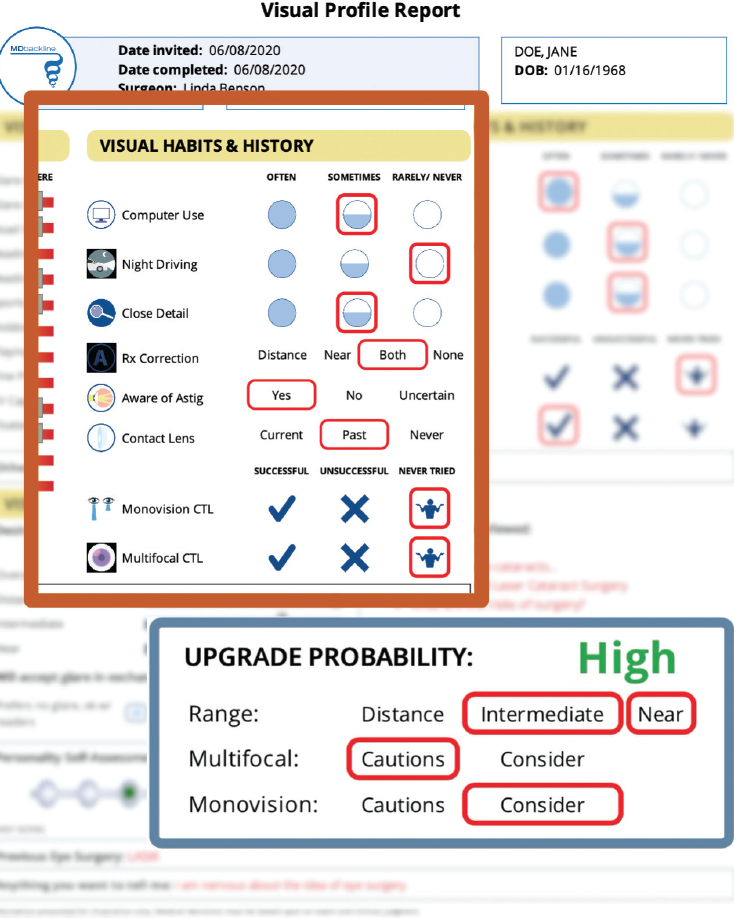
Figure 5. Sample MDbackline visual profile report showing a patient’s visual history and likelihood of upgrading to a premium IOL.
Courtesy of John A. Hovanesian, MD
CONCLUSION
New technologies are making it easier for surgeons to serve patients better with a greater range of vision and fewer IOL-related side effects. Future approvals will extend indications to include more irregular eyes and patients seeking true accommodation. Lastly, innovative software is available to assist practices in identifying the best candidates for premium IOLs and to help patients understand and accept these options.
Premium IOLs Make Up Only a Small Percentage of Lenses Implanted
Tetsuro Oshika, MD, PhD
Tsukuba, Japan

My preferred IOLs are currently the Vivinex iSert (model XY1, Hoya Surgical Optics) and the Lentis Comfort (model LS-313 MF15, Teleon Surgical).
The Vivinex is a monofocal IOL, and I find its preloaded delivery system to be extremely well-made, highly reliable, and user-friendly. The IOL itself is of high quality, and it can be implanted through a 2.2- to 2.4-mm incision.
The Lentis Comfort is a segmented, rotationally asymmetric, EDOF IOL with a +1.50 D near add. This IOL is categorized in the monofocal segment because its cost is completely covered by public insurance in Japan and the incidence of photic phenomena is very low.
At our center, premium IOLs account for approximately 10% to 20% of the lenses we implant. A majority of these are the AcrySof IQ PanOptix IOL and the Tecnis Synergy IOL.
Patient Satisfaction High With Premium Lenses
William F. Wiley, MD
Cleveland, Ohio

Premium IOL options continue to improve. As a result, indications for the use of these lenses are expanding, helping many of us increase value to our patients. Currently, our conversion rate to premium IOLs is around 35%.
THREE AREAS OF IMPROVEMENT
Ultimately, the uptick in the use of premium IOLs within my practice is due to three main areas of improvement in lens design.
Adjustability. We prefer the Light Adjustable Lens for challenging eyes (ie, those with a history of refractive surgery) and for patients who are unsure of their goals for distance vision or their monovision targets.
Trifocality. The FDA approval of the AcrySof IQ PanOptix IOL has helped us become more confident with counseling patients on premium lens technology because our patients’ satisfaction is high with this lens. We feel confident that patients will experience a full range of vision with minimal side effects.
EDOF. The newest premium IOL category that is gaining popularity within our practice is EDOF. In our experience with this type of lens design, distance vision is not compromised, and the additional intermediate vision provides patients with more function compared to traditional monofocal platforms. We have seen patient adoption of EDOF lenses increase as the technology improves.




