INTRODUCTION
In a previous installment of Glaucoma Today and Cataract & Refractive Surgery Today, I sat down with a group of glaucoma surgeons to discuss the confines of surgeons’ visualization into the recesses of the eye with modern MIGS procedures. We focused on why clear visualization is foundational to successful outcomes for surgeons performing MIGS. We characterized the limitations of current visualization techniques and outlined how bimanual surgery (which would be enabled by a truly hands-free visualization platform) would unlock the full potential of MIGS.
Here, we continue the conversation by turning our focus to the GONIO ready® (OCULUS Surgical). The GONIO ready® is a single-use gonioscopy system that attaches to the surgical microscope, thereby freeing the hand a surgeon typically uses for viewing the angle during a MIGS procedure. The device debuted earlier this year.
In this final part of our conversation, we consider how a hands-free visualization system could affect training young surgeons, compare and contrast the merits of disposable and reusable technology, and share our initial impressions and pearls of this new technology for new users. Readers seeking to learn more about the device can visit oculussurgical.us/gonioready for more details.
—Iqbal “Ike” K. Ahmed, MD, FRCSC
Dr. Ahmed: I’d like to pick up where we left off in our previous installment of this roundtable by continuing our discussion on the potential benefits of true bimanual surgery during MIGS.
Edward Yung, MD: It’s easy to imagine the benefits of bimanual approaches in the current MIGS landscape: we’ve all been in a situation where we wished for a free hand. But it’s easy to overlook how a bimanual approach might allow the emergence of novel MIGS technology that requires both hands to use. Sometimes emerging MIGS technologies have stunning potential but are limited by difficult placement. By having a free hand, we can mitigate the challenges of a device’s difficult application.
Dr. Ahmed: Some surgeons favor reusable visualization platforms, while others prefer single-use technology during MIGS procedures. What are the benefits of using one over the other?
Ahmad Aref, MD, MBA: As someone who works in a hospital system that closely monitors costs, I use reusable devices. Visualization is very clear early in a reusable device’s lifecycle, but the quality of the view deteriorates over time—a frustrating reality that may contribute to inefficiency while performing surgery.
Leonard K. Seibold, MD: Busier surgical settings may benefit from single-use devices that eliminate the need for sterilization and autoclaving. Streamlining processes in an ASC that faces high patient turnover makes surgery more efficient, and single-use platforms have an advantage over reusable technology in these situations.
Dr. Yung: I sometimes find that reusable devices are defective out of the package. Maybe they’re not so defective that they’re unusable—say, they have a smudge or a scratch on the lens that interferes with perfect visualization but still allows an adequate view—but when that happens, it ultimately undercuts the argument for reusables.
Dr. Ahmed: The GONIO ready® is a single-use microscope-integrated gonioscopy system that allows glaucoma surgeons to free one of their hands during MIGS procedures. To those on the panel who have experience with the GONIO ready®, what would you advise new users to keep in mind when first using this technology?
Paul Harasymowycz, MD: The good news is that the overall learning curve is low, and new users will adjust easily. I advise new users to consider the importance of presurgical placement of both the patient’s head and the microscope equipped with a GONIO ready®. It takes some practice, but after you get into a routine where you’re comfortable with a hands-off visualization approach, you’ll have a set of positioning protocols that you’ll use for future encounters. Also, prepare to use your foot pedal for visualization. It takes some getting used to.
Ticiana De Francesco, MD: I’ve noticed that the GONIO ready® does not have a flange that interferes with visualization, which makes it distinct from some so-called hands-free lenses. When a flange covers the limbus or an incision, it’s easy to become frustrated.
Dr. Seibold: New users should know that the design has been tweaked with real-world applications in mind. For example, the patented Flex System on the GONIO ready® has been key to maintaining dynamic lens positioning during surgery. The earliest iterations of the GONIO ready® did not have a flexible arm connected to the lens, which meant that I sometimes lost contact with the eye when moving laterally. That’s no longer an issue.
Dr. De Francesco: Also, new users should remember that very little pressure is placed on the eye when using the GONIO ready® (Figure). This introduces a new—and welcome—dynamic to MIGS procedures.
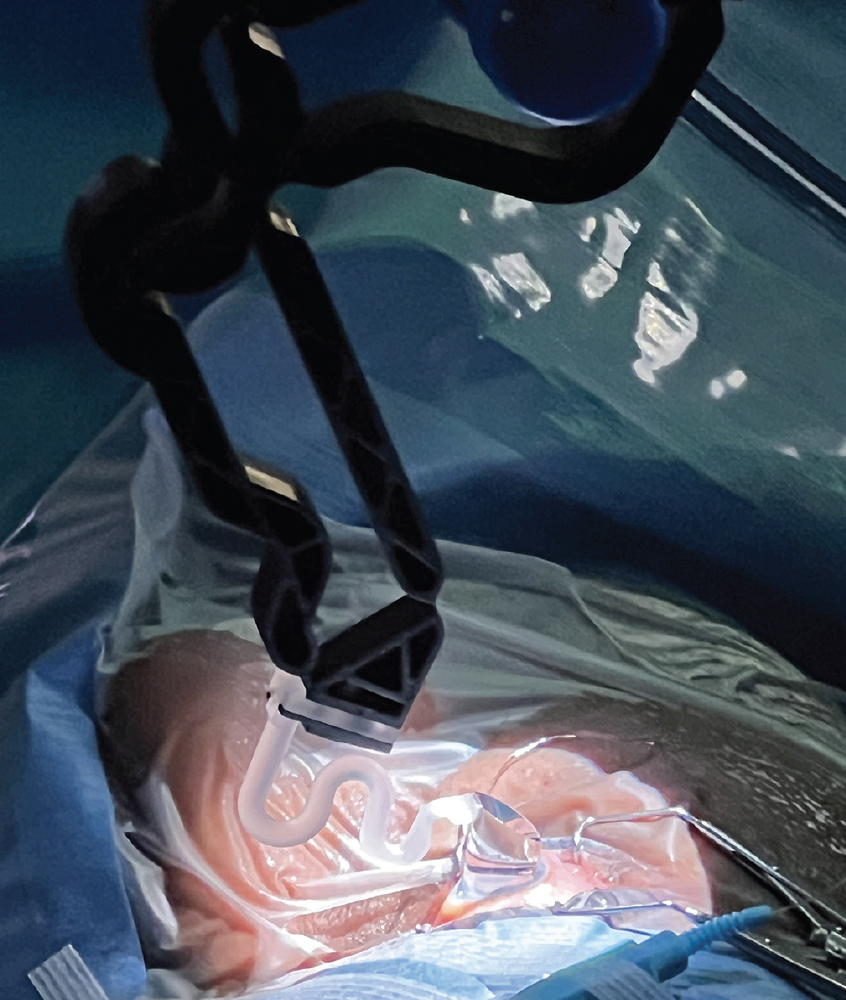
Figure. The GONIO ready® places little pressure on the cornea during a MIGS procedure, and surgeons may find that the anterior chamber depth is better maintained during surgery.
Dr. Ahmed: How might new technology such as the GONIO ready® affect the lives of surgical trainees?
Dr. Aref: I have performed about 15 to 20 MIGS teaching cases with a truly bimanual approach using GONIO ready®, and this visualization approach has been very helpful to my trainees. Those I have trained have picked up visualization with the device quickly, which speaks to the low learning curve Dr. Harasymowycz described earlier.
Preceptors and mentors must be careful to continue to educate fellows with other visualization technologies, both so those trainees can understand which device works best for their approach, and so they can learn how to perform surgery when a bimanual approach is not an option.
Dr. Yung: Dr. Aref makes a good point: We have a natural bias to become most comfortable with the systems on which we are trained, so we should be cautious about overexposing trainees to a single visualization method lest they become dependent on it. Still, early experience with the GONIO ready® is an important step forward in glaucoma surgery training, because if residents and fellows are exposed to such technology while they are still forming intellectual frameworks of our specialty, they may move our field forward in a way we have not yet conceptualized.
Dr. Ahmed: I’d like to thank the members of this panel for joining me in this conversation. I expect to hear more from you all—and from our peers in the MIGS space—as experience with the GONIO ready® increases.









