Dry eye disease (DED) is a common condition that affects more than 38 million people in the United States.1 Identified by a loss of homeostasis of the tear film, DED can cause corneal discomfort and visual symptoms that negatively impact an individual’s quality of life.2 Recently, Jai G. Parekh, MD, MBA, FAAO, and Cynthia Matossian, MD, FACS, hosted a webinar to discuss current clinical approaches to identifying, diagnosing, and treating DED for ophthalmologists who seek to better understand this condition and help improve their patients’ outcomes. What follows is a summary of that discussion.
Etiology and Classifications of DED
Disrupting DED’s cycle of ocular surface damage, inflammation, and visual impairment depends on clinicians’ ability to determine the appropriate differential diagnosis and treatment.3 The etiology of DED is often multifactorial, potentially involving deficiencies in the aqueous, lipid, or mucin components of the tear film. Mixed-modal DED may contain various combinations of aqueous, lipid, or mucin deficiencies.3 DED is commonly classified as either aqueous-deficient dry eye (ADDE) or evaporative dry eye (EDE).3-5 Symptoms can be exacerbated by environmental conditions, wearing contact lenses, the presence of preservatives in ophthalmic drops, allergies, and/or eyelid or blink abnormalities.3
Meibomian gland dysfunction (MGD), which affects tear-lipid quantity and/or quality,3 is considered the leading cause of DED.4,5 Evaporation associated with MGD contributes to ocular surface damage and inflammation (Figure 1). In a retrospective study, Lemp et al6 sought to evaluate the numbers of patients with ADDE or EDE among a general clinic-based cohort (spread across 10 sites throughout the United States and European Union) of patients with DED. Of the 224 individuals who were classified with DED, 159 patients were categorized into 1 of 3 specific subtypes: 79 (50%) had MGD alone; 23 (14%) had pure aqueous deficiency; and 57 (36%) had both. In all, 136 of 159 patients (86%) had signs of MGD (Figure 2).6
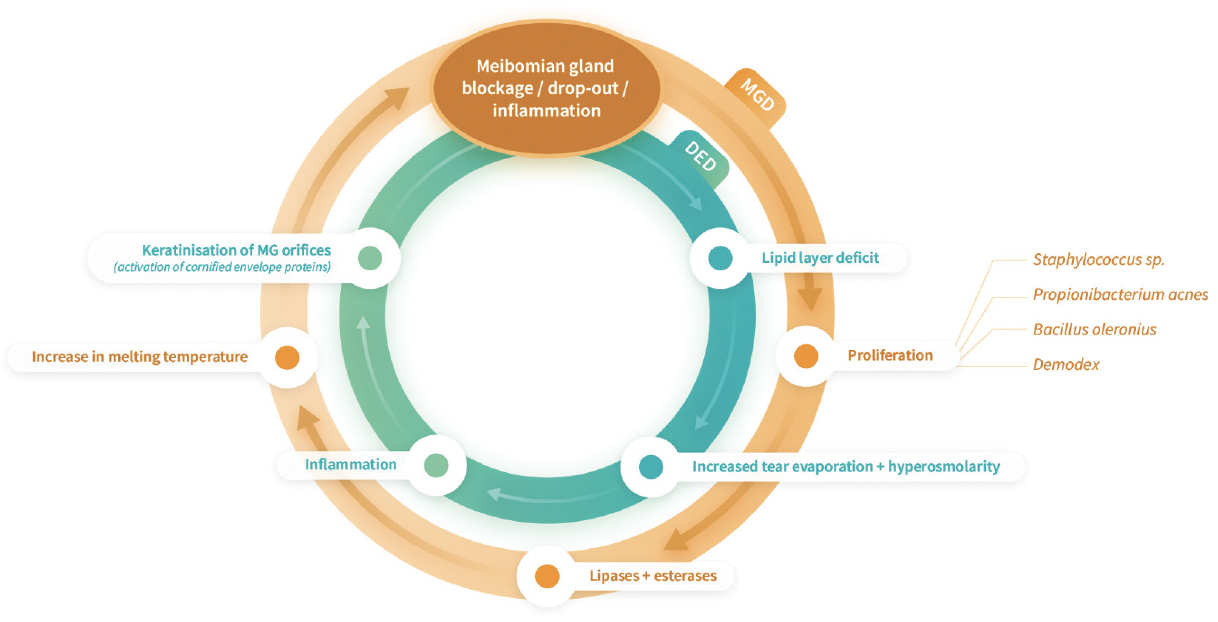
Figure 1. MGD-induced evaporation leads to ocular surface damage and inflammation.a,b Evaporation destabilizes the tear film and causes ocular surface desiccation and tear hyperosmolarity.9 Hyperosmolarity triggers inflammation that damages the ocular surface directly and indirectly.4,9 (Derived from a. Baudouin C et al. Br J Ophthalmol. 2016. b. Craig JP et al. Ocul Surf. 2017.)
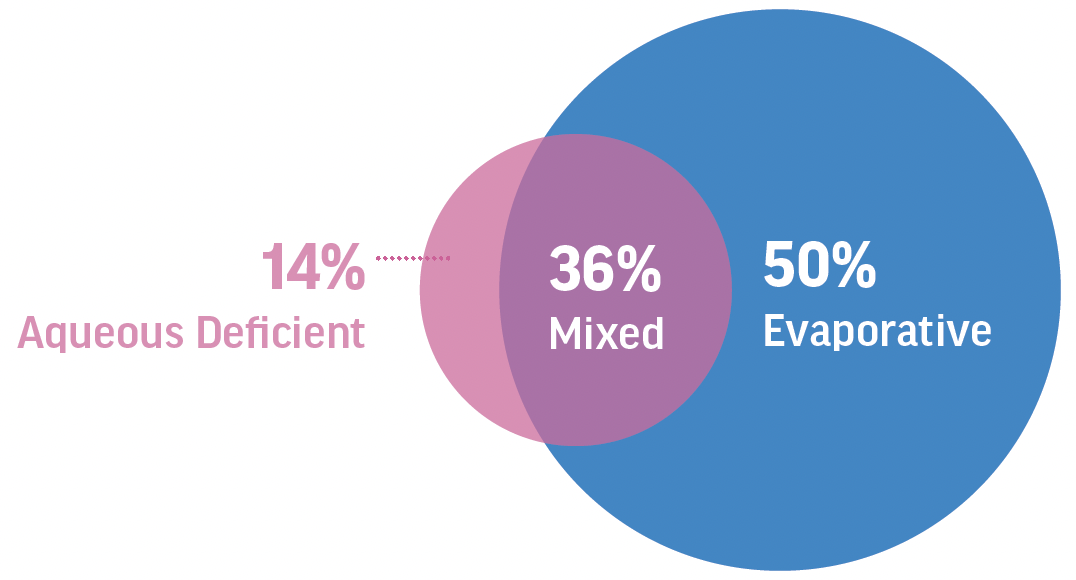
Figure 2. Excessive evaporation is the main consequence of MGD. In 86% of cases, DED has an evaporative etiology, with MGD as a major contributor. (Derived from Lemp M et al. Cornea. 2012.)
“The worse the MGD, the thinner the lipid layer is, which causes an increase in evaporation7 and tear film instability,”8 explained Dr. Matossian. “Tear evaporation and instability lead to ocular surface desiccation and tear hyperosmolarity, which in turn damage the ocular surface directly and indirectly by triggering inflammation.9 This all results in two vicious cycles that contribute to each other.”
Tailoring Treatment Options for DED
Drs. Matossian and Parekh noted that DED treatment is largely limited to topical lubricants, anti-inflammatory drugs, immunomodulators, tear stimulators, and in-office procedures, such as meibomian gland expression. Over-the-counter treatments can provide temporary relief by supplementing tears; however, they do not address the underlying causes of evaporative DED, leaving the cycle of surface damage and inflammation unbroken. “One of the challenges of treating DED is that current treatments can be associated with high rates of dissatisfaction and discontinuation,”10,11 said Dr. Parekh. “This is partly because no eye drops are specifically designed to target evaporation, which is a key factor in many cases of DED.”
Prescription medications, such as cyclosporine and lifitegrast, have been shown to be effective in treating DED, he continued, but onset of action is often delayed. As with all medications, side effects are a consideration. Dr. Parekh added that some non-pharmacological interventions, such as lid scrubs and massage, and certain alternative therapies (ie, omega-3 supplements), help improve meibomian gland function, reduce inflammation, and provide patients symptomatic relief.
Improving Patient Outcomes
Dr. Matossian stressed that DED’s complexity requires a multipronged treatment approach. “It is important to note that not all cases of DED are the same, and treatment should be tailored to the individual patient based on the underlying causes of their condition.” For example, she said, patients with aqueous-deficient DED may require different treatments than those with evaporative DED. In some cases, a combination of therapies may be necessary to achieve optimal outcomes.
“As eye care professionals, it is essential to diagnose and treat the underlying causes of the disease to stop the cycle of ocular surface damage and inflammation,” said Dr. Parekh. “Despite the availability of various treatments for DED, there is still a need for more effective and targeted therapies. New research is being conducted to identify innovative treatments that can help improve outcomes for patients with this condition.”
©2023 Bausch & Lomb Incorporated or its affiliates. NOV03.0005.USA.23
1. 2020 Dry Eye Products Market Report: A global analysis for 2019 to 2025. Market Scope. Available at: https://www.market-scope.com/pages/reports/250/2020-ophthalmic-landscape-report-global-analysis-for-2019-to-2025-april-2021#reports. Accessed April 12, 2023.
2. Dana R, Meunier J, Markowitz JT, et al. Patient-reported burden of dry eye disease in the United States: results of an online cross-sectional survey. Am J Ophthalmol. 2020;216:7-17.
3. McMonnies CW. Aqueous deficiency is a contributor to evaporation-related dry eye disease. Eye and Vis (Lond). 2020;7:6.
4. Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15(3):276-83.
5. Bron AJ, de Paiva CS, Chauhan SK, et al. TFOS DEWS II pathophysiology report. Ocul Surf. 2017;15(3):438-510.
6. Lemp M, Crews LA, Bron AJ, et al. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea. 2012;31(5):472-478.
7. Goto E, Endo K, Suzuki A, et al. Tear evaporation dynamics in normal subjects and subjects with obstructive meibomian gland dysfunction. Invest Ophthalmol Vis Sci. 2003;44(2):533-539.
8. Kim WJ, Ahn YJ, Kim MH, et al. Lipid layer thickness decrease due to meibomian gland dysfunction leads to tear film instability and reflex tear secretion. Ann Med. 2022;54(1):893-899.
9. Baudouin C, Messmer EM, Aragona P, et al. Revisiting the vicious circle of dry eye disease: a focus on the pathophysiology of meibomian gland dysfunction. Br J Ophthalmol. 2016;100(3):300-306.
10. White DE, Zhao Y, Ogundele A, et al. Real-world treatment patterns of cyclosporine ophthalmic emulsion and lifitegrast ophthalmic solution among patients with dry eye. Clin Ophthalmol. 2019;13:2285-2292.
11. Schaumberg DA, Uchino M, Christen WG, et al. Patient reported differences in dry eye disease between men and women: impact, management, and patient satisfaction. PLoS One. 2013: 8(9):e76121. doi: 10.1371/journal.pone.0076121.


