CASE PRESENTATION
A 27-year-old man with extreme myopia presented in late 2022 for a refractive surgery consultation. An evaluation with the Pentacam (Oculus Optikgeräte) revealed normal corneal anatomy and an anterior chamber depth (ACD) of 3.14 mm OD and 3.16 mm OS. Specular microscopy with the SP-300P (Topcon) found a healthy corneal endothelium in each eye. Both crystalline lenses were clear.

Figure 1. Anterior segment OCT of the right (A) and left (B) eyes.
The patient’s glasses prescription had been stable for 3 years, and he was contact lens intolerant. His BCVA was 6/7.5+3 OD with a manifest refraction of -17.50 -2.00 x 170º and 6/9.5+2 OS with a manifest refraction of -19.25 -2.00 x 35º. He reported not regularly rubbing his eyes. His IOP readings were 11 mm Hg OD and 13 mm Hg OS. The IOLMaster (Carl Zeiss Meditec) measured axial lengths of 32.45 mm OD and 32.37 mm OS.

Figure 2. OCT of the optic disc.
A posterior examination of each eye revealed myopic changes, including staphyloma with tilted discs and peripapillary atrophy; white without pressure; lattice degeneration but no breaks; and an epiretinal membrane that was more severe in the right eye.
After being counseled on his surgical options, the patient decided to delay intervention because of financial insecurity after the COVID-19 pandemic.
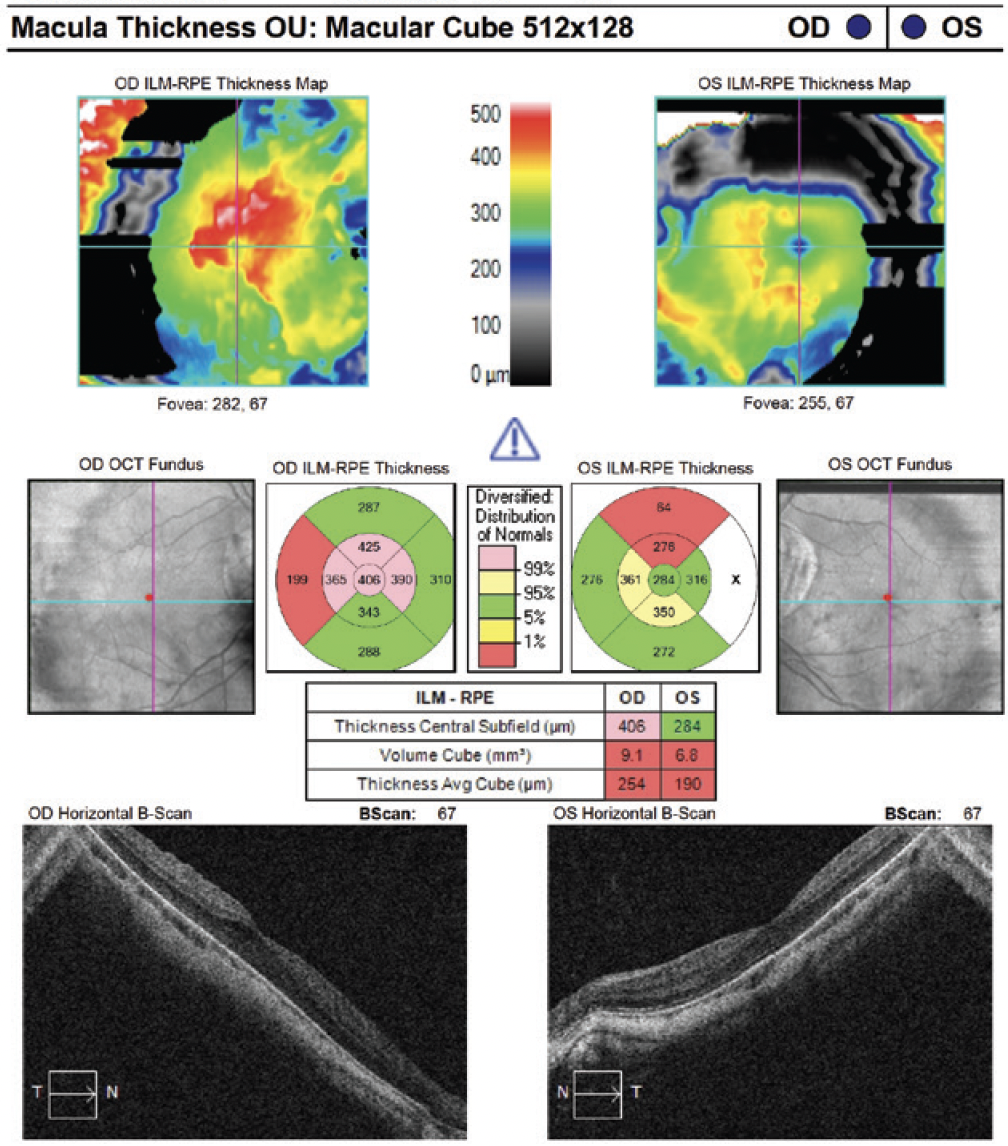
Figure 3. Macular OCT.
He returns approximately 2.5 years later ready to book surgery. His hobbies include jujitsu and riding a motorcycle. Changes to the macula in the right eye, including macular schisis (Figure 4), are detected, but the patient’s BCVA has remained stable.

Figure 4. Macular OCT of the right eye 2.5 years after the scan shown in Figure 3.
How would you proceed?
—Case prepared by Abi Tenen, MBBS(Hons), FRANZCO

JOHN F. DOANE, MD, FACS
This patient has extreme axial myopia with stigmata of pathologic myopia. He has significant visual impairment without contact lenses or glasses.
Before proceeding with refractive correction, I routinely refer patients like this one for evaluation by a retina specialist. In this situation, I would inform the retina specialist that a bioptics procedure is planned—phakic IOL implantation combined with corneal laser vision correction (LVC).
OCT of the optic nerve seems consistent with the myopic status of the left eye. The epiretinal membrane in the right eye does not appear to be affecting the patient’s BCVA, so it probably would not cause a problem with the placement of a phakic IOL. An EVO ICL (STAAR Surgical) would be implanted to correct most of the patient’s refractive error, and corneal LVC would be performed to treat the remainder. By my calculations, the placement of an ICL with the highest spherical power available (-18.00 D) and +1.50 D of toric power would leave him with a refractive error of -1.25 +0.23 x 080º OD and -2.36 +0.19 x 125º OS.
Because he participates in contact sports, I would offer either PRK or laser-assisted lenticule extraction (LALEX) rather than LASIK to correct his residual refractive error.

PARAG A. MAJMUDAR, MD
The patient has extreme myopia. In situations like this one, vision correction can be life-changing and pose minimal risk if all preoperative parameters are appropriate.
Only a phakic IOL could safely correct the degree of myopia in this case. Given his stable refractive error, appropriate internal ACD, and healthy corneal parameters, the patient appears to be a good candidate. In the United States, where I practice, only three options are available: an EVO ICL, which has a maximum power of -15.00 D; a Visian ICL (STAAR Surgical); and a Verisyse/Artisan IOL (Johnson & Johnson Vision/Ophtec).
An advantage of the EVO ICL is that it does not require a laser peripheral iridotomy. The lens might also be less likely to induce cataract formation. The patient would have to understand, however, that a secondary procedure such as PRK or LASIK might be required to treat residual ametropia. I am not sure if the EVO ICL is available in higher myopic powers outside the United States.
The Visian ICL may be available in higher powers, but the higher potential for pupillary block and earlier cataract formation might dissuade me from this approach.
I have had success with the Verisyse lens, but it cannot correct astigmatism, because it has a large optic and is not foldable. In my experience, placing the large incision at the steep meridian can reduce preexisting astigmatism, and the lens is available in higher myopic powers than the EVO.
I have seen several patients with extreme myopia who have refracted to less than 20/20 (6/6) but whose BSCVA after the implantation of a phakic IOL was better. Outcomes depend on the status of the macula. I always counsel these patients that 20/20 (6/6) BSCVA may not be achievable because of the degree of their myopia.

BRETT MUELLER II, DO, PHD
The patient presents with a spherical equivalent of -18.50 D OD and -20.25 D OS. The corneal evaluation revealed no contraindications to either LASIK or SMILE, and the ACD measured 3.14 mm OD and 3.16 mm OS.
I would counsel him that, given the degree of myopia, no single procedure could eliminate his refractive error. Following clearance from a retina specialist for lattice degeneration, I would recommend a bioptics approach. First, approximately -16.00 D spherical equivalent would be addressed by implanting a toric EVO ICL. Then, if indicated, LVC would be performed to treat the residual myopia.
Preoperatively, I would inform the patient that he might be satisfied with his vision following refractive lens surgery and therefore might choose to defer additional treatment. Should he wish to pursue full emmetropia, however, I would recommend LALEX or PRK rather than LASIK because of his participation in combat sports to minimize flap-related risks.

DAGNY ZHU, MD
The patient presents with a mild decrease in BCVA, greater in the left than the right eye, secondary to pathologic myopia. Although corneal topography appears normal, his refractive error is too high to be safely addressed with LVC. The endothelial cell count is healthy. Assuming the internal ACD is greater than 3.00 mm OU, he appears to be a suitable candidate for an EVO ICL.
Before proceeding, several factors must be considered. Given his extreme myopia, the patient may have anatomic variations that could make ICL sizing and placement challenging. The white-to-white distance or, ideally, the sulcus-to-sulcus distance would be measured with ultrasound biomicroscopy to determine his candidacy for an ICL. Furthermore, given his participation in jiujitsu and motorcycle riding, the patient would receive extensive counseling on the potential risks of eye injury, ICL dislocation and rotation, and cataract formation. Because the maximum amount of correction with the EVO ICL in the United States, where I practice, is -15.00 D spherical equivalent, the patient may need a laser vision enhancement following phakic IOL implantation.
My preferred approach would therefore be the bilateral implantation of spherical EVO ICLs (to eliminate the risk of toric ICL rotation) followed by flapless laser vision enhancement (PRK or LALEX) at least 3 months after refractive stability has been achieved.
Before surgery, he would be referred to a retina specialist, who would educate the patient about his macular conditions and perform scleral depression to evaluate him for peripheral retinal holes or tears, with treatment performed if warranted.

WHAT I DID: ABI TENEN, MBBS(HONS), FRANZCO
The patient’s refractive errors were beyond the range of LVC, and refractive lens exchange posed a high risk due to his age and myopic changes. I had therefore recommended an EVO ICL during his initial consultation in 2022. I had also advised him that sparring in martial arts could cause a significant injury to his eyes, which would be of even greater concern with a phakic lens in situ.
Calculations showed that implanting the highest-powered ICL available in Australia, where I practice, would result in an approximately 2.50 D undercorrection in each eye. The patient and I decided that a refractive surgery enhancement could be performed as appropriate. I reasoned that PRK might be the best option because no suction would be applied to the eyes.
When the patient returned to my office in April 2025, the progressive macular changes in the right eye led me to postpone surgery for at least 6 months to determine if the retina remains stable. He is also being monitored by a vitreoretinal surgeon, who thinks that imminent ICL surgery is appropriate.




