Despite major advances in corneal surgery, penetrating keratoplasty (PKP) continues to have a role in disease management. The challenges of full-thickness transplants include a lengthy healing period and variability in the healing process among patients. As corneal surgeons remove the PKP sutures over the course of a year, they make adjustments in an effort to minimize astigmatism. Long-term, high-dose postoperative steroid treatment raises PKP patients’ risk of developing glaucoma, and this therapy combined with the transplantation procedure can also hasten cataract formation.
Successfully managing these cases requires consideration of the whole patient. Some of these patients do well with glasses or contact lenses, and after thorough discussion, they choose to continue with these forms of refractive correction after cataract surgery. Other patients wish to reduce their dependence on glasses or contact lenses. Some questions to ask are
- Is their astigmatism regular or irregular, and what options might be employed to reduce it?
- Are patients on topical medical therapy for glaucoma? If so, they may be candidates for microinvasive glaucoma surgery; a number of these procedures will not induce astigmatism.
CASE EXAMPLE
A 40-year-old man developed an infection in his right eye and underwent a full-thickness corneal transplant. Over the course of a year, the patient’s sutures were removed, leaving him with fairly regular corneal astigmatism (Figure 1). He developed a cataract and glaucoma in his right eye from postoperative steroid treatment. The IOP measured 24 mm Hg OD on a fixed combination of brimonidine tartrate and timolol maleate (Combigan, Allergan) dosed twice daily.
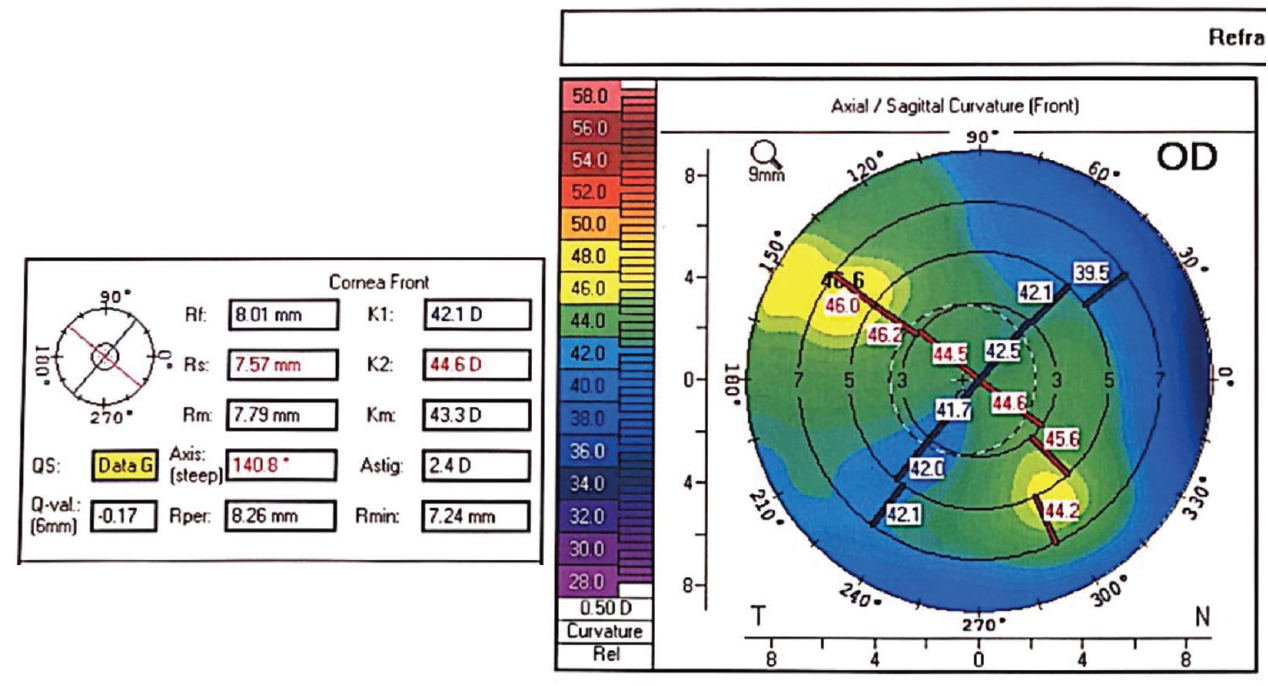
Figure 1. Topography demonstrated regular astigmatism after PKP.
The patient decided to proceed with cataract surgery. Because he desired as much freedom from glasses and contact lenses as possible, I recommended a toric IOL to correct the 2.00 to 3.00 D of regular astigmatism present in his right eye. To address the mild glaucoma safely and effectively with minimal refractive impact, I recommended implantation of the iStent Trabecular Micro-Bypass Stent (Glaukos) in combination with cataract surgery.
When operating on a post-PKP eye, I am careful to protect the corneal graft. I therefore coated the endothelium with a dispersive OVD, made the main cataract incision slightly more posteriorly than usual to avoid the graft-host interface, and minimized phaco time.
I used intraoperative aberrometry to fine-tune the spherical and toric powers of the IOL and to assist with the IOL’s axial alignment. Based on preoperative measurements, the online toric calculator had recommended a 20.00 D model SN6AT5 AcrySof IQ Toric IOL (Alcon; Figure 2), but intraoperative aberrometry recommended a higher toric power, specifically the 20.00 D model SN6AT6 AcrySof IQ Toric IOL. Surgeons should exercise judgment and caution in cases such as this one, because intraoperative aberrometry may not be able to accurately capture corneas that are irregular or that have undergone various procedures such as PKP and radial keratotomy. Next, I implanted the iStent in the standard fashion while being mindful of the corneal graft. To maximize astigmatic correction with the IOL, I carefully removed the OVD from behind the IOL and confirmed the accuracy of its alignment.
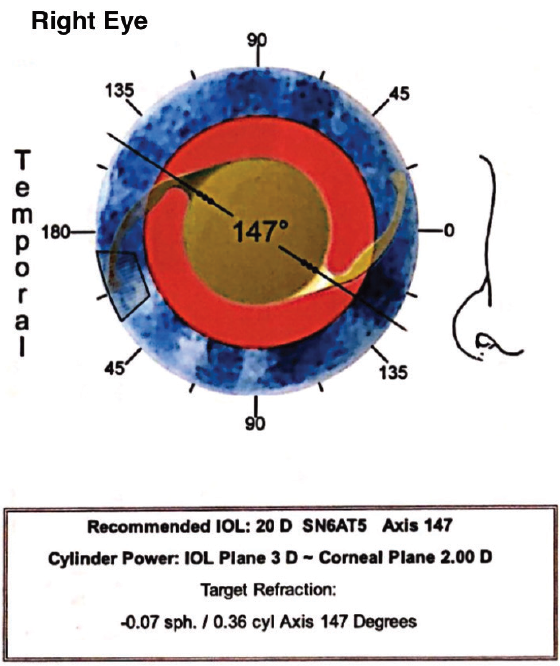
Figure 2. The online toric calculator recommended placing a toric IOL that would correct for 20.00 D of astigmatism at the corneal plane.
The patient did well. Four months postoperatively, he had a distance UCVA of 20/20 and an IOP of 12 mm Hg on no antihypertensive medication. He continued to administer a steroid drop once daily.

