CASE PRESENTATION
A 63-year-old man presents for a second opinion. The patient underwent cataract surgery on his nondominant left eye elsewhere by a skilled surgeon 5 months ago. A monofocal posterior chamber IOL was placed in the bag, and a good anatomic result was achieved. His postoperative UCVA is 20/200 and J1+ OS. His BCVA is 20/20- with a manifest refraction of -2.50 -0.25 x 125º OS. The fellow eye has a cataract that is not visually significant, and his UCVA is 20/20- and J16 OD.
The patient underwent myopic LASIK many years ago. A discussion with him suggests that surgery likely took place in the early 2000s. He is unsure what the amount of correction was in each eye. He states that the cataract surgeon did not mention that a history of LASIK can render IOL calculations less predictable. The patient also says that a refractive plan and target and IOL options were not discussed with him before cataract surgery. He does not want to return to his original surgeon.
The patient does not recall if he had monovision before cataract surgery. He reports no symptoms of anisometropia. He says that “everything is blurry” and that he is extremely bothered by a lack of intermediate vision (Figures 1 and 2). He is unhappy with his vision overall and does not want to wear glasses. He has traveled a fair distance for the consultation and is willing to make a return flight for surgery, but he is self-employed and does not want to miss a lot of work.
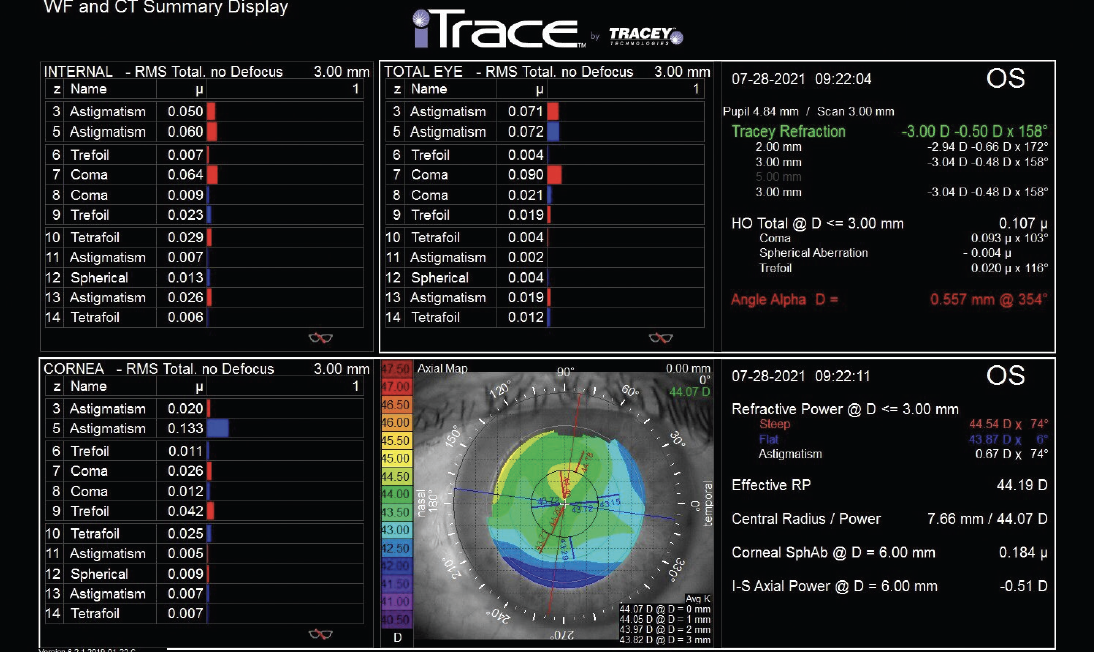
Figure 1. Aberrometry of the left eye using the iTrace (Tracey Technologies).
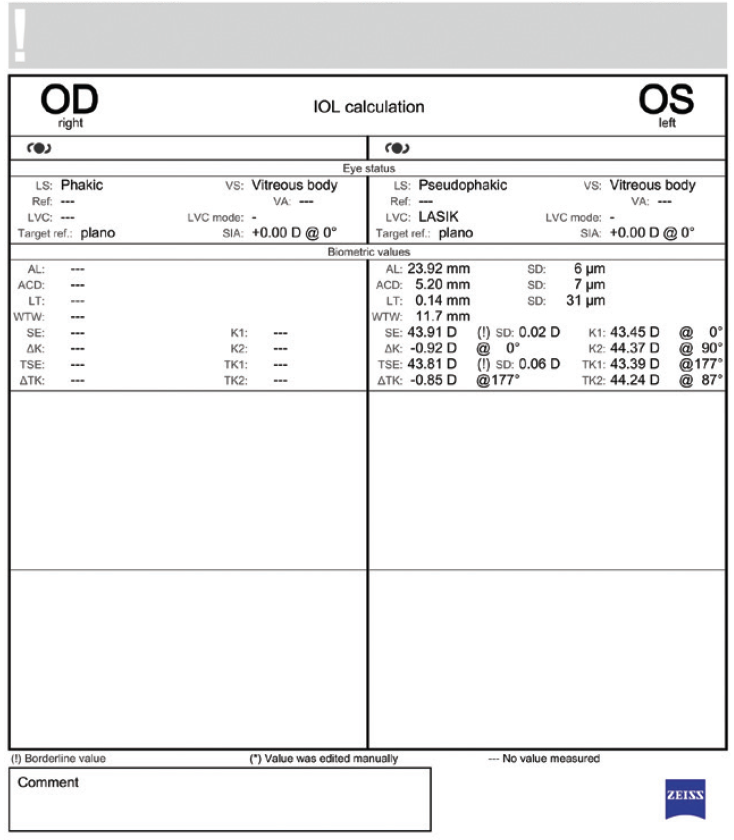
Figure 2. Biometry of the left eye using the IOLMaster 700 (Carl Zeiss Meditec).
What are the patient's options? If you recommend laser vision correction (LVC), would you lift the flap or perform PRK? If you recommend an IOL exchange, how would you choose the IOL power? Would you use the same IOL or a different one? How would you counsel the patient about the risks of an IOL exchange and another refractive miss?
—Case prepared by Neda Nikpoor, MD

BRETT MUELLER, DO, PHD
The patient is not happy with his overall UCVA and wants a solution. First, I would try to determine what about his vision upsets him. I would point out that the distance vision in his right eye and the near vision in his left eye are very good. If he acknowledges that he is happy with both, then I can focus on how to enhance his overall UCVA by slightly improving his uncorrected intermediate visual acuity.
I would discuss with the patient the possibility of performing an IOL exchange and potentially placing a trifocal IOL in his left eye. I am comfortable implanting this type of IOL in patients who have a history of myopic LVC, especially if the magnitude of higher-order aberrations is less than 0.4. I have also had a lot of success placing a trifocal IOL in one eye and leaving the other eye phakic. Patients usually experience neural adaptation and appreciate a seamless continuous range of vision.
If the patient is concerned about experiencing glare and halos postoperatively, then I would offer him the option of receiving either a Clareon Vivity IOL (Alcon) or Light Adjustable Lens (RxSight) in the left eye with a refractive target of -0.75 to -1.00 D. Based on my experience, this approach should give him good intermediate and near vision in the left eye while the right eye provides good distance vision.


ARTHUR VAN DEN BERG, MD, AND GEORGE O. WARING IV, MD, FACS
The first step is a lengthy discussion of the patient’s goals and different ways of achieving them. He has several options, one of which is an LVC enhancement. PRK with the application of mitomycin C for 24 seconds could be considered. We would not recommend lifting the LASIK flap for the enhancement because of the increased risk of epithelial ingrowth. A contact lens trial simulating a target refraction of -1.50 D would be conducted to see if the patient enjoys the intermediate and near visual acuity achieved with blended vision and reduced anisometropia. If he does not, a contact lens trial simulating full distance correction would be performed.
An IOL exchange is seemingly a better alternative. We generally favor an extended depth of focus IOL such as the Tecnis Symfony OptiBlue (Johnson & Johnson Vision) for eyes with a history of myopic LASIK. The refractive target would be planned for -0.35 D in the nondominant eye. Cataract surgery would then be performed on the fellow eye. The same IOL would be implanted with the intended refractive target of plano. The ORA system (Alcon) would be used with the Barrett True K formula. A back calculation for the pseudophakic eye would also be performed to estimate IOL power with the intended target of -0.35 D. Prior to surgery, we would advise the patient that he may require a refractive enhancement and discuss the risks and benefits of both an IOL exchange and extended depth of focus IOLs.

WHAT I DID: NEDA NIKPOOR, MD
As the contributing authors stated beautifully, the first step in a situation like this one is to identify the patient’s goals and set realistic expectations.
A thorough discussion and a trial of different refractive targets revealed that the patient was satisfied with monovision but bothered by the degree of anisometropia. He was happy with -1.25 to -1.50 D of myopia. We discussed the challenges of hitting the refractive target in eyes that have a history of LASIK as well as the pros and cons of various options to correct his vision. I advised against lifting the LASIK flap because of the risk of ingrowth and against PRK because of the unpredictable outcome and leaving him with a monofocal lens. I recommended an IOL exchange for a Light Adjustable Lens (my first choice) or a Vivity IOL (my second choice).
Because the patient wished to avoid multiple flights to see me, he decided to undergo an IOL exchange for a Vivity IOL with a target of -1.25 D. Preoperatively, we again discussed the risks of surgery, including the possibility of an inaccurate IOL calculation and capsular rupture. The patient’s refractive error and biometry were used to back calculate the appropriate IOL power, and the plan was confirmed with intraoperative aberrometry (ORA System).
One day after surgery, the patient was extremely satisfied with his uncorrected vision. One month after surgery, his uncorrected distance visual acuity in the operated eye was 20/50, uncorrected near visual acuity was J1+, and his refraction was -1.50 -0.25 x 010° OS. He felt no need to wear glasses to see at any distance and was very pleased with his outcome.




