CRST spoke to Sondra Black, OD, and Jeffery J. Machat, MD, FRCSC, DABO, about their personal experiences as recipients of the Kamra corneal inlay from AcuFocus. Drs. Black and Machat practice at CrystalClear Vision in Toronto, where the inlay has been available since 2012.
CRST: Describe your current visual function and your experience having the Kamra inlay implanted in your eye.
Sondra Black, OD: Jeff performed my monovision LASIK in 1998, when I was 40. At that time, there was no other option for me, and I was determined not to have to wear reading glasses, because that is the first sign of aging. My vision was excellent—for a while. As I got older, I “grew” out of my monovision LASIK as my presbyopia inevitably progressed. I was able to function, but I felt a little off balance at all distances. I was getting headaches and was wearing reading glasses for extended reading and computer work and also needed glasses for night driving. I told Jeff that we had to find a solution for presbyopia!
We investigated scleral implants, multifocal ablations, and other methods. When we started hearing about the inlay, we became very interested. Jeff had the procedure done in Tokyo, and I was in the surgery room. When he was reading the very next day, I said, “Now, you have to do my eyes, because I am older than you, and this is not fair.”
Once we obtained the proper pocket software to be able to go below my LASIK flap, Jeff did my inlay in front of 60 optometrists, who were watching from our waiting room (Figures 1 and 2). I returned to work the following day. My vision was hazy, and I had to increase the font size on my laptop and phone, as I was determined not to wear my readers. Over the first week, however, I started noticing what I called “moments of clarity,” when I could see clearly through the haze, but then it would disappear. By the end of the first week, I was able to decrease my font size and struggle through. During the next few weeks, my vision continued to become sharper and sharper, and I was able to function without glasses.

Figure 1. Dr. Black undergoing Kamra implantation.
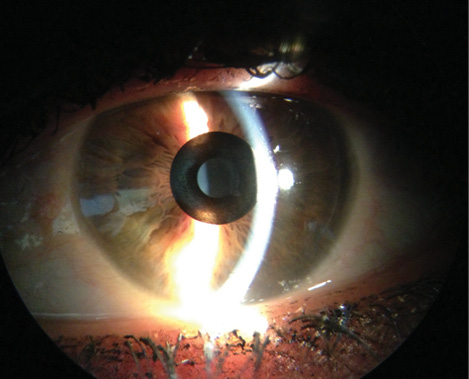
Figure 2. Dr. Black’s eye implanted with the inlay.
I also noticed that, with monovision, my intermediate vision was never clear. Now, that my distance vision is clear, I do not wear my night-driving glasses as I am more binocular and my distance [vision] is better. It will be 2 years at the end of June since I had the procedure, and I have not had to put on reading glasses. My eyes were quite dry at the beginning, so I started myself on Restasis (cyclosporine; Allergan). The drops improved the clarity of my vision, and even over the past year, it has continued to improve. A year ago, in a dim restaurant, I had occasional trouble reading the menu. Now, I can see better under those circumstances as well, so my visual quality has been continually improving.
CRST: Did you have symptoms of dry eye disease before the procedure? Were you pretreated?
Dr. Black: I did not pretreat; I had punctal plugs put in. I was post-LASIK, and with my fully menopausal system, everything was drying up, including my tear film. I was not symptomatic, as I would have expected, but my dry eyes did affect my vision.
CRST: Is the inlay visible in your eye?
Dr. Black: No, you cannot see it at all when you look at me. Patients do not notice it, and neither do my friends. Outside in the sun, if I am not wearing sunglasses, the pupil that has the inlay in it looks larger, because it maintains that 3.8-mm size, whereas the other one is constricted, but the inlay itself is not visible. In a person with light-colored eyes, from an angle, it may be visible. We have never had a patient want the inlay removed for cosmetic reasons.
Jeffery J. Machat, MD, FRCS, DABO: I got to watch Sondra basically suffer with her presbyopia and found great joy and amusement in it … until I hit 50, and presbyopia’s effects hit me quite dramatically. I was surprised at the impact it had on my quality of my life; I just never expected it. When my 16-year-old daughter started to torment me with regard to the size of the font I had on my smartphone, I decided to do something. At that point, it became an emergency! I realized that, of all the procedures that Sondra and I had been experimenting with—researching, testing, and learning about—the one that intrigued me the most was the Kamra.
In terms of the technology, there were certain very specific factors that I thought were critical for a surgeon with a type A personality. I needed to be binocularly balanced. Sondra is very easygoing, as are most of my successful monovision LASIK patients, but I knew that I was not one of them. I was also concerned about the loss of stereopsis and my ability to perform surgery. The Kamra has allowed me to maintain my stereopsis and feel balanced at distance. Frankly, I was able to return to surgery within days, feeling comfortable and safe. It was exactly what I had hoped for (Figure 3).
I also wanted a procedure that gave me, not just near vision, but intermediate vision. Monovision and many refractive procedures that are based on a prescription have two real problems. One is they only provide clear vision at a given distance. The second is that, as presbyopia advances, the effect is lost. The Kamra procedure addresses both of these issues. It absolutely gives continuous clear vision from very close to very far with no dead spots. It also corrects for advancement of my presbyopia. I had the procedure done in August 2012. I have noticed that my dominant right eye is seeing worse at near, but I have had no changes whatsoever in the past 3 years to my inlay eye and my ability to see close. So, that was another critical decision-making point.
Another factor was that I did not want a multifocal ablation, as I did not want to risk losing my visual quality. The Kamra would not affect the clarity or sharpness of my central vision. The inlay uses small-aperture optics and has a central clear zone, which was extremely important to me. I have not had to sacrifice my distance clarity, and the device is removable and therefore reversible, which increases the safety profile and makes it attractive to patients. This is one of the most critical factors that drew me to the inlay.
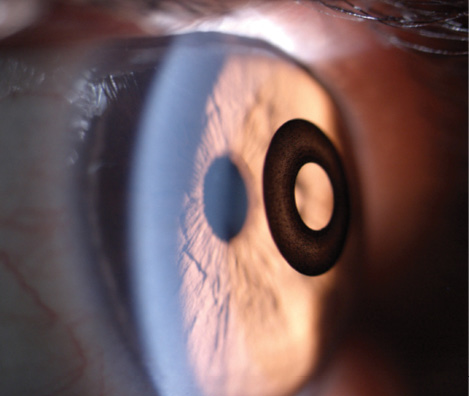
Figure 3. The Kamra inlay in Dr. Machat’s eye.
I think corneal inlays will play a huge role in presbyopic treatment over the course of the next decade or two. The Kamra is the first of a number of corneal inlays that I expect to see approved in the United States. Inlays provide real options for baby boomers such as myself, my friends, and my colleagues, and the devices allow us to continue to feel young, which is probably the most important aspect for me. Each and every time I had to put on reading glasses, I felt old, so to eliminate them is to turn back the clock.
Some of my friends who were myopic and never wanted LASIK are now getting LASIK and [the] Kamra. The sudden need for bifocals has pushed them to make the leap. Our LASIK volume has increased since we started implanting the Kamra, and so have our refractive lens exchange (RLE) cases.
CRST: Expand on the synergies of the inlay and RLE.
Dr. Machat: We use the AcuTarget HD (AcuFocus) in our practice to show patients what is happening with their lens. Our approach is, “You have a vision problem. We have a vision solution.” Presbyopic patients who already present with an elevated optical scatter index, which demonstrates that they have early lens changes that go along with age and the beginning of cataract formation, may be far better off having an RLE procedure. The diagnostic instrument helps us educate them about what we recommend and why.
With the addition of the Kamra inlay, our entire practice has grown, and we think of ourselves as a presbyopia practice. We hired an age-appropriate patient consultant, somebody in her 50s so that she can talk to and relate to our patients who are coming in with these vision problems. She has had the Kamra inlay implanted, so she really does understand. Her husband had an RLE. She has a great background for educating patients and helping them understand that we are going to pick the best procedure for them based upon their corneal and lens findings. n
Sondra Black, OD
• vice president and clinical director at Crystal Clear Vision Canada, Toronto
• (416) 928-0777 or (416) 988-8495; sondra.black@crystalclearvision.com
• financial disclosure: consultant to AcuFocus
Jeffery J. Machat, MD, FRCSC, DABO
• founder and chief medical director of Crystal Clear Vision in Toronto, Canada
• (416) 928-0777; jeff.machat@crystalclearvision.com
• financial disclosure: consultant to AcuFocus