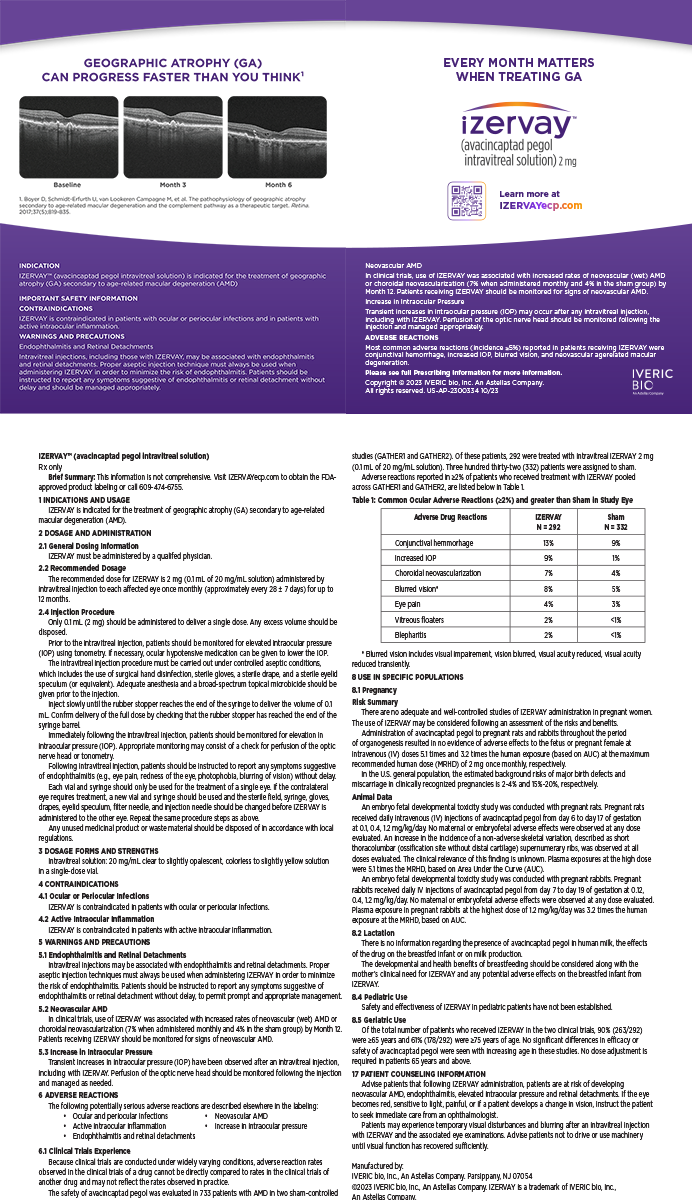
In the past, one of the main issues regarding PRK was that some patients developed visually significant haze weeks to months following the surgery (Figure 1). During the last 2 to 3 years, refractive surgeons' improved understanding of the risk factors for the condition and new prophylactic treatments have dramatically reduced the risk for haze following surface-ablation procedures. The decreased risk of vision loss coupled with a desire to avoid various LASIK complications has prompted many ophthalmologists to readopt surface ablation as their primary refractive surgery procedure.
CAUSESUV Exposure
I became very interested in postoperative haze during my cornea fellowship in 1996 and 1997. Approximately 3 months after a seemingly successful PRK, one of my patients left for a 4-day deep-sea fishing trip off the coast of Mexico. When he returned, he had severe haze. He also revealed that he had been exposed to a great deal of sunlight because he had not worn sunglasses during his trip.
Aleksander Stojanovic, MD, of Tromso, Norway, noticed the same association between UV exposure and haze, and his practice was perfectly located to study this observation. Near the Arctic Circle, it is dark 24 hours per day during the wintertime and light 24 hours per day during the summer months. Dr. Stojanovic's cases of haze following PRK occurred only in the summer and correlated closely to the environmental levels of UV radiation.1
Laser Energy
The second main risk factor for developing postoperative haze relates to the amount of laser energy applied to the cornea. Patients with higher degrees of myopia (&Mac179; 6.00 D) seem to run the greatest risk of haze because they require deeper ablations. Similarly, larger optical zones entail deeper ablation and therefore a greater risk of postoperative haze. At the 2002 annual ASCRS meeting in Philadelphia, Ning Lin, MD, of Columbia, South Carolina, reported2 that his patients' risk of haze following LASEK increased when the total depth of ablation exceeded 100 µm.
Prior Corneal Surgery
Previous corneal surgery such as RK, LASIK, and even corneal transplantation has been reported as a risk for haze following PRK.3,4
UV Protection
The most basic method of haze prevention is for patients to wear sunglasses with complete UV protection and to avoid exposure to high levels of UV radiation during the first year following PRK or LASEK.
Vitamin C
After identifying the problem of postoperative haze, Dr. Stojanovic began studying the effects of vitamin C in his patients based on the observations of Amund Ringvold, MD, PhD, of Oslo, Norway, that reindeer have high levels of vitamin C in their corneas and that this vitamin has antioxidant properties. In a forthcoming study, Dr. Stojanovic treated patients with 1,000 mg of vitamin C q.d. for 1 week preoperatively and during the first 2 weeks following PRK. He found that the patients' risk of haze decreased from 3.7% to zero with oral vitamin-C supplementation.
Mitomycin C
The prophylactic use of mitomycin C (MMC) is the subject of intense controversy in the field of refractive surgery. An Italian study5 of high myopes undergoing PRK found that none of the patients who received preoperative, prophylactic treatment with MMC developed haze following surgery, whereas some of the patients who did not receive treatment did develop haze postoperatively. The investigators also reported that prophylactic MMC was relatively safe but noted that its use required them to reduce the laser energy treatment by 10%. Nevertheless, we do not currently know the long-term risk posed by the application of MMC on the central cornea. For that reason, many surgeons question the appropriateness of using the agent for all patients with higher levels of myopia.
LASEK Versus PRK
Debate continues regarding whether postoperative haze is less likely to occur after LASEK than PRK. Several surgeons have anecdotally affirmed this statement, but, as yet, there is no definitive study in the literature on the subject.
SIGNIFICANT POSTOPERATIVE HAZE
The first step in treating postoperative haze is to apply topical steroids. If the haze fails to clear in 4 to 6 weeks, the next step is to remove the scar. A few years ago, this would have involved manual debridement with a diamond bur, applying MMC 0.02% to the corneal surface to prevent the further development of haze, and then allowing the cornea to heal. Today, many refractive surgeons elect to perform a superficial PTK on these patients, followed by the application of MMC to prevent the haze from recurring.6 The reason for this change in procedures is that a manual keratectomy is more likely to produce an irregular corneal surface that can render follow-up treatments more challenging.
CONCLUSION
A better understanding of the causes of postoperative haze, combined with the advent of prophylactic techniques including vitamin-C supplementation and the topical application of MMC, enable refractive surgeons to feel more comfortable about the prospect of performing PRK and LASEK on patients with higher degrees of myopia or who have undergone previous corneal surgery. As a result, it appears that surgeons' use of surface-ablation procedures is on the rise.
1. Stojanovic A, Nitter TA. Correlation between ultraviolet radiation level and the incidence of late-onset corneal haze after photorefractive keratectomy. J Cataract Refract Surg.2001;27:404-410.
2. Lin N. Prediction of corneal haze using ablation depth and AD/CT ratio in post-LASEK patients. Paper presented at: the ASCRS/ASOA 2002 Symposium on Cataract, IOL and Refractive Surgery; June 1, 2002; Philadelphia, PA.
3. Gimbel HV, Sun R, Chin PK, van Westenbrugge J. Excimer laser photorefractive keratectomy for residual myopia after radial keratotomy. Can J Ophthalmol. 1997;32:1:25-30.
4. Artola A, Ayala MJ, Perez-Santonja JJ, et al. Haze after laser in situ keratomileusis in eyes with previous photorefractive keratectomy. J Cataract Refract Surg. 2001;27:1880-1883.
5. Carones F, Vigo L, Scandola E, Vacchini L. Evaluation of the prophylactic use of mitomycin-C to inhibit haze formation after photorefractive keratectomy. J Cataract Refract Surg. 2002;28:2088-2095.
6. Porges Y, Ben-Haim O, Hirsh A, Levinger S. Phototherapeutic keratectomy with mitomycin C for corneal haze following photorefractive keratectomy for myopia. J Refract Surg. 2003;19:40-43.