A physician's perspective

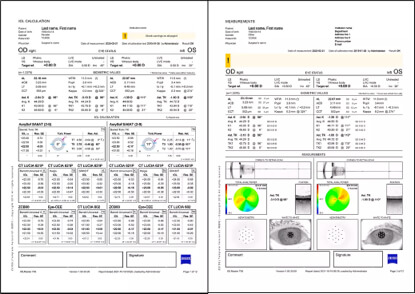
Modern surgeons are lucky enough to live in an age with advanced biometers that allow surgeons to improve the precision of their presurgical IOL calculations. My clinic leverages the power of the ZEISS IOLMaster 700 to reduce the risk of refractive surprises, optimize workflow, and improve refractive outcomes.
Let's explore each of those benefits in detail.
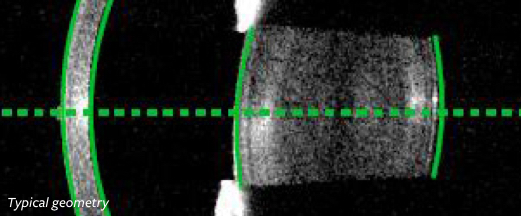
Reduced risk of refractive surprises. Traditional IOL power calculation relies on an exact measurement (ie, that of the anterior corneal surface) and an estimate of total corneal power (ie, a nomogram). The ZEISS IOLMaster 700 features Total Keratometry, a technology that accounts for the posterior corneal surface when making IOL power calculations, thereby replacing the assumption made by a nomogram with a precise anatomic measurement acquired via swept-source OCT. Patients with atypical corneal geometries can now have their unique anatomy accounted for in the presurgical period.
Total Keratometry on the ZEISS IOLMaster 700 has proven to be particularly effective when managing cases of patients with astigmatism. In my estimation, 40% of the patients who visit my clinic have astigmatism. With Total Keratometry, I can rest assured that my total corneal power calculations are as accurate as possible for these patients.
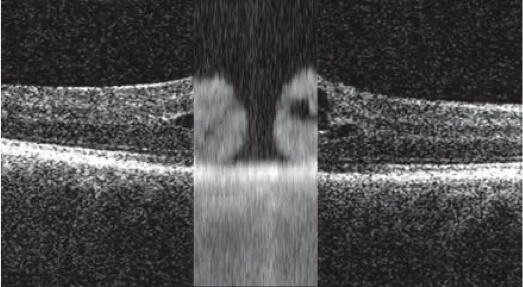
Optimized workflow. Assessment with the ZEISS IOLMaster 700 is part of my clinic's routine cataract evaluation for new patients. Patients with dense cataracts can be assessed using the ZEISS IOLMaster 700, which allows my staff to stick with an efficient, easy-to-use platform rather than move that patient to ultrasound imaging.
In my opinion, surgeons who use the ZEISS VERACITY Surgery Planner platform will maximize their experience with the ZEISS IOLMaster 700. Calculations captured by the ZEISS IOLMaster 700 are at a surgeon’s fingertips in the OR when employing ZEISS VERACITY Surgery Planner.
Improved refractive outcomes. A surgical practice that includes technology such as the ZEISS IOLMaster 700 may experience reduced rates of postsurgical enhancements thanks to the more exact nature of IOL calculations. At my practice, I have noticed a marked decline in the rate of requested enhancements from astigmatic patients, which I credit in part to the precise presurgical measurements I am empowered to obtain via the ZEISS IOLMaster 700. This, in turn, has made my practice more efficient, as I am able to spend more time with new patients in need of cataract surgery.
Surgeons who wish to embrace cutting-edge innovations in their practice should consider adding the ZEISS IOLMaster 700 to their preoperative routine. The easy integration of the platform into a clinic means that workflow and patient throughput will not be disrupted, and more precise total corneal calculations may mean higher rates of patient satisfaction and reduced rates of surgical enhancements—all of which leads to increased clinical efficiency and more satisfied patients.
William Trattler, MD
Dr. Trattler is a consultant for Carl Zeiss Meditec, Inc.
References:
1. Jack T. Holladay, MD, Hidden Figures, Cataract & Refractive Surgery Today Europe, April 2018
2. Depending on experience of operator and eye conditions.
3. R. Varsits, N. Hirnschall, B. Doeller, O. Findl; Increasing the number of successful axial eye length measurements using swept-source optical coherence tomography technology compared to conventional optical biometry; presented at ESCSR 2016.
4. Srivannaboon S, Chirapapaisan C. Comparison of refractive outcomes using conventional keratometry or total keratometry for IOL power calculation in cataract surgery. Graefe's Arch Clin Exp Ophthalmol. 2019;257(12):2677-2682.
5. Yeo TK, Heng WJ, Pek D, Wong J, Fam HB. Accuracy of intraocular lens formulas using Total Keratometry in eyes with previous myopic laser refractive surgery. Eye. 2020.
6. ZEISS IOLMaster 700 Central Topography does not replace a full topography. For any further diagnosis please use a topographer.
The statements of the doctor in this insert reflect only his personal opinions and do not necessarily reflect the opinions of any institution with which he is affiliated. The doctor shown in this insert has a contractual or other financial relationship with Carl Zeiss Meditec, Inc. and has received financial support.
Not all products and services are available in all countries.
CAP-en-US_32_025_0227II

Sponsored by ZEISS