When I approach a patient on topical medication for mild to moderate glaucoma about having cataract surgery, I virtually always recommend a mixed procedure with microinvasive glaucoma surgery (MIGS) to treat both diseases. There are many reasons I make that choice.
Compliance is an issue we face in managing glaucoma patients because of either the difficulties with instillation, the continued increase in medication cost, or the subjective intolerance. In addition, we all know topical glaucoma medications can cause ocular surface disease, especially when multiple medications are used. But I’m more concerned with the pathologic alterations to the tissues in or around the eye from a medication’s active ingredient and/or its preservative.
Benzalkonium chloride is generally accepted to cause surface issues, but more importantly, it has been shown to induce apoptosis of the endothelial cells lining the trabecular columns.1,2 Furthermore, glaucoma medications have been shown to cause meibomian gland dysfunction3 and ultrastructural changes to conjunctival goblet cells,4 which may ultimately affect the health of the tear film. Prostaglandins have also been shown to increased cytotoxins in Tenon’s tissue,5 which may reduce the efficacy of future filtration surgeries.6
Pairing MIGS With Cataract Surgery
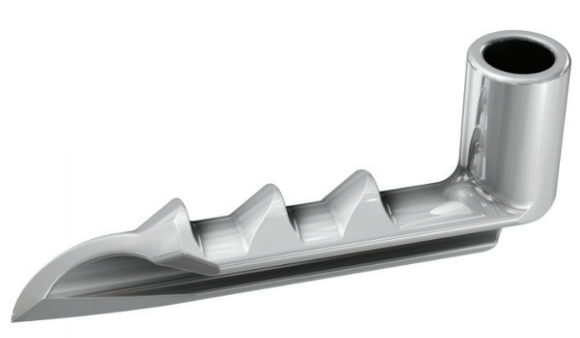
I choose MIGS devices based on the appearance of the drainage angle, the stage of glaucoma, health of the optic nerve, measured IOP and distance from the target as well as number of medications. For patients with controlled mild to moderate open-angle glaucoma (OAG) with a healthy-looking angle, I often opt to bypass the trabecular meshwork (TM) with an iStent Trabecular Micro-ByPass Stent (Glaukos).
If, on the other hand, a patient has uncontrolled OAG on multiple medications, or if the angle appears unhealthy with multiple areas of goniosynechiae or a variegated pattern of pigmentation on the TM, I’ll often couple multiple procedures (such as iStent with endoscopic cyclophotocoagulation). If the angle is unhealthy and the patient is further advanced, my risk tolerance increases and justifies accessing a different drainage pathway altogether such as the suprachoroidal or subconjunctival space.
I’ve generally found all MIGS procedures to be effective and ultimately provide patients with IOPs in the low to mid-teens.7-9 In my experience, the suprachoroidal space can successfully reduce IOP, but it’s not without risk. This pathway is more unpredictable and, as such, we have seen patients develop chronic hypotony after supraciliary stent implantation. We also have been surprised with other adverse events, such as myopic shifts, chronic iritis, and pressure spikes following cleft closure. Nevertheless, utilizing the suprachoroidal space remains an important and viable option for managing select patients.
Trabecular ablative procedures occur further along in my algorithm for three reasons. First, the inner wall of Schlemm's canal is an important blood aqueous barrier, and its removal can allow blood to regurgitate into the anterior chamber with any action that increases the episcleral venous pressure (weightlifting, head-down positions, Valsalva maneuvers, etc), blurring a patient’s vision.10 Second, the TM is an aqueous pump that assists in expulsion of aqueous into and through the distal collector system.11
Lastly, we have many new exciting devices that soon will be available to MIGS surgeons like the iStent inject (Glaukos) and the iDose (Glaukos). These devices would be difficult to use if the nasal TM is removed early in our treatment algorithm. The nasal angle has become our new conjunctiva, so minimizing manipulation initially will allow further manipulation of the system in the future. With that said, in patients with an excessively pigmented TM associated with pigmentary glaucoma or pseudoexfoliative glaucoma and very high pressures on multiple medications, I find a focal ablative procedure to the TM to be effective when stenting is not an option.
All of these options help us lower pressure and reduce or eliminate the need for topical medications. In many cases, MIGS helps bring glaucoma under control and reduces dependency on drops. But for the large number of patients who have mild to moderate glaucoma, iStent offers an opportunity to treat the disease much earlier than we did in the past.
A Safe, Effective Early Option
The proven efficacy of iStent comes along with an excellent safety profile that has been widely studied and reported, with over 300,000 devices implanted to date. The procedure is elegant, and I’ve been able to maximize the excellent results I see with targeted implantation. When determining stent placement location, I aim for areas within the canal that have a significant amount of blood regurgitation, because I know that area of the canal is patent and connected to a functional distal collector system. We can further maximize stent efficacy by implanting the stent adjacent to collector channels. These areas are highlighted by an increased amount of blood regurgitation or blotching within the canal.
After successful implantation, I want to see some level of blood regurgitation either through the snorkel of the stent or around the stent itself, which tells me that the stent is well seated. Additionally, upon evacuation of viscoelastic from the anterior chamber, I look for blanching of the episcleral venous system, which further confirms precise stent positioning. If I do not see regurgitation of blood around the stent or blanching, I often reposition the stent by sliding it over a bit. This works very well and makes iStent a forgiving procedure.
The excellent results, proven safety profile, and minimal disruption to my practice are among the reasons iStent is my go-to procedure for patients with mild to moderate OAG.
1. Baudouin C, Denoyer A, Desbenoit N, et al. In vitro and in vivo experimental studies on trabecular meshwork degeneration induced by benzalkonium chloride (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2012;110:40-63.
2. Rasmussen CA, Kaufman PL, Kiland JA. Benzalkonium chloride and glaucoma. J Ocul Pharmacol Ther. 2014;30(2-3):163-169.
3. Arita R, Itoh K, Maeda S. Comparison of the long-term effects of various topical antiglaucoma medications on meibomian glands. Cornea. 2012;31(11):1229-1234.
4. Zhu W, Kong X, Xu J, Sun X. Effects of long-term antiglaucoma eye drops on conjunctival structures: an in vivo confocal microscopy study. J Ophthalmol. 2015;2015:165475.
5. Koh SW, Coll TJ, Rose L, et al. Antiglaucoma eye drop pulses—increased interleukin-6 secretion by Tenon’s capsule fibroblast cultures. J Glaucoma. 2004;13(3):200-209.
6. Broadway DC, Grierson I, O’Brien C, Hitchings RA. Adverse effects of topical antiglaucoma medication. II. The outcome of filtration surgery. Arch Ophthalmol. 1994;112(11):1446-1454.
7. Pahlitzsch M, Davids AM, Zorn M, et al. Three-year results of ab interno trabeculectomy (Trabectome): Berlin study group. Graefes Arch Clin Exp Ophthalmol. 2018;256(3):611-619.
8. Fea AM, Rekas M, Au L. Evaluation of a Schlemm canal scaffold microstent combined with phacoemulsification in routine clinical practice: Two-year multicenter study. J Cataract Refract Surg. 2017;43(7):886-891.
9. Vold S, Ahmed II, Craven ER, et al. Two-year COMPASS Trial results: supraciliary microstenting with phacoemulsification in patients with open-angle glaucoma and cataracts. Ophthalmology. 2016;123(10):2103-2112.
10. Ahuja Y, Malihi M, Sit AJ. Delayed-onset symptomatic hyphema after ab interno trabeculotomy surgery. Am J Ophthalmol. 2012;154(3):476-480.
11. Carreon T, van der Merwe E, Fellman RL, et al. Aqueous outflow—a continuum from trabecular meshwork to episcleral veins. Prog Retin Eye Res. 2017;57:108-133.
INDICATION FOR USE. The iStent® Trabecular Micro-Bypass Stent (Models GTS100R and GTS100L) is indicated for use in conjunction with cataract surgery for the reduction of intraocular pressure (IOP) in adult patients with mild to moderate open-angle glaucoma currently treated with ocular hypotensive medication. CONTRAINDICATIONS. The iStent® is contraindicated in eyes with primary or secondary angle closure glaucoma, including neovascular glaucoma, as well as in patients with retrobulbar tumor, thyroid eye disease, Sturge-Weber Syndrome or any other type of condition that may cause elevated episcleral venous pressure. WARNINGS. Gonioscopy should be performed prior to surgery to exclude PAS, rubeosis, and other angle abnormalities or conditions that would prohibit adequate visualization of the angle that could lead to improper placement of the stent and pose a hazard. The iStent® is MR-Conditional meaning that the device is safe for use in a specified MR environment under specified conditions, please see label for details. PRECAUTIONS. The surgeon should monitor the patient postoperatively for proper maintenance of intraocular pressure. The safety and effectiveness of the iStent® has not been established as an alternative to the primary treatment of glaucoma with medications, in children, in eyes with significant prior trauma, chronic inflammation, or an abnormal anterior segment, in pseudophakic patients with glaucoma, in patients with pseudoexfoliative glaucoma, pigmentary, and uveitic glaucoma, in patients with unmedicated IOP less than 22 mmHg or greater than 36 mmHg after “washout” of medications, or in patients with prior glaucoma surgery of any type including argon laser trabeculoplasty, for implantation of more than a single stent, after complications during cataract surgery, and when implantation has been without concomitant cataract surgery with IOL implantation for visually significant cataract. ADVERSE EVENTS. The most common post-operative adverse events reported in the randomized pivotal trial included early post-operative corneal edema (8%), BCVA loss of ≥ 1 line at or after the 3 month visit (7%), posterior capsular opacification (6%), stent obstruction (4%) early post-operative anterior chamber cells (3%), and early post-operative corneal abrasion (3%). Please refer to Directions for Use for additional adverse event information. CAUTION: Federal law restricts this device to sale by, or on the order of, a physician. Please reference the Directions for Use labeling for a complete list of contraindications, warnings, precautions, and adverse events.
iStent and Glaukos are registered trademarks of Glaukos Corporation. PM-GL-0016