Introduction
Keratometry readings are important parameters needed to determine the exact IOL power. Different SS-OCT biometers employ different approaches to measure the corneal curvature, which leads to slightly different readings.
The question is, how do these different approaches in measuring the corneal power affect IOL power calculations in standard cataract in normal eyes? This article summarizes literature that compared keratometry readings between the available SS-OCT biometers and discusses the impact on monofocal and toric IOL power calculations.
Comparison of keratometry measurements
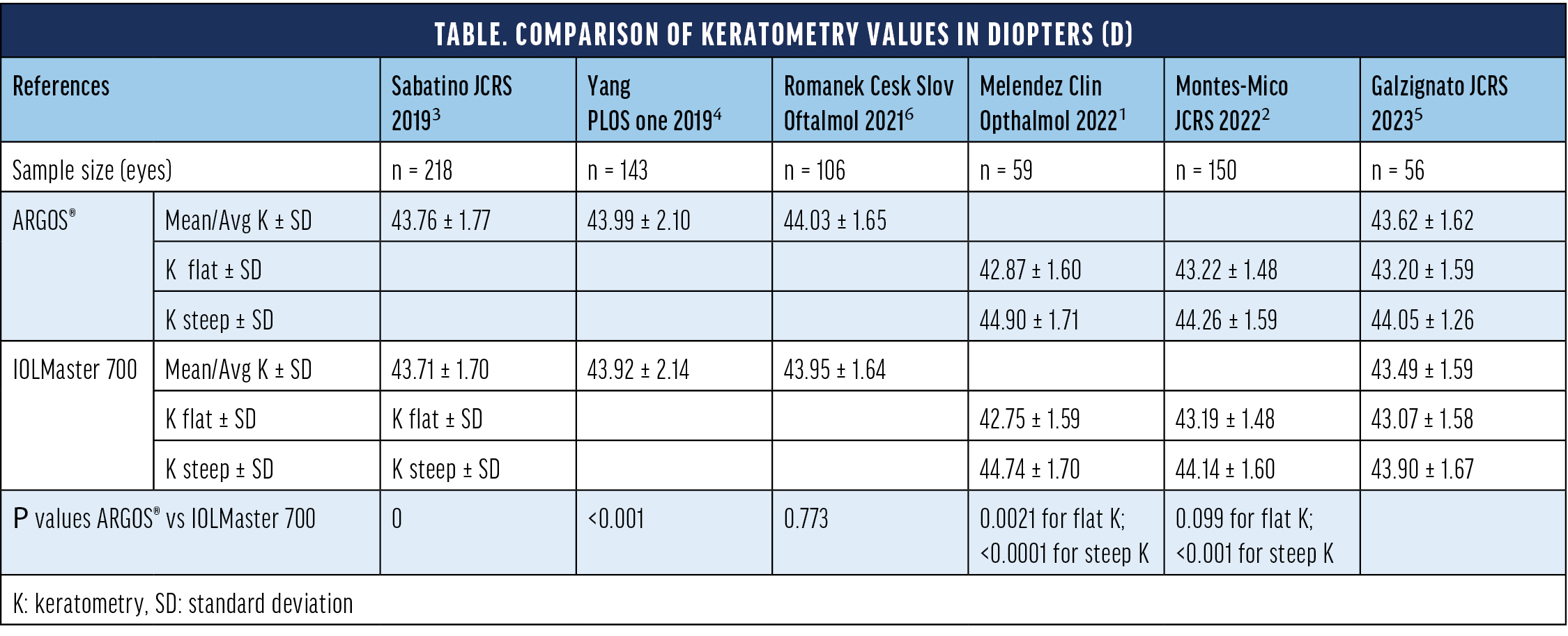
There are a number of studies that compared the ARGOS® (Alcon) and IOLMaster 700 (ZEISS) (Table). Overall, differences in keratometry readings were generally small and did not exceed 0.16 D. In many cases, however, comparisons reached statistical significance.1-5 A significant trend toward flatter K-readings for the IOLMaster 7001-4 in comparison to ARGOS® can be noted. These differences are likely caused by the different measurement approaches.
Impact on monofocal IOL power calculations
The largest sources of error that influence monofocal IOL power calculations and refractive outcomes include: predicted postoperative anterior chamber depth (35%), predicted postoperative refraction (27%), axial length (17%), and pupil size (8%) measurements.7 The influence of keratometry is small. Anterior corneal keratometry measurements contribute approximately 2%, and the ratio of anterior/posterior corneal keratometry readings contributes approximately 4% to the error sources.7
The outcomes of monofocal IOL power calculations therefore do not seem to show differences between the ARGOS® and IOLMaster 700 biometers. Omoto et al8 identified significant differences in the mean anterior corneal radius curvature between these biometers, but the percentage of eyes within ± 0.5 D prediction error was similar for various IOL power calculation formulas. A similar conclusion was drawn by Yang et al4 assessing the effect of IOL power calculations using the Haigis formula. Authors did find significant differences in the average keratometry readings (Table), but these changes are not considered to be clinically significant to influence the final refraction.
Impact on toric IOL power calculations
The contribution of individual error sources shifts significantly when we investigate toric IOL power calculations. The largest error source is derived from the corneal measurement contributing 0.59 D (27% of the total error sum).9 Within the corneal measurement error source, 0.26 D are the result of differences between devices (including posterior corneal surface), 0.14 D corneal radii, 0.10 D diurnal changes, and 0.09 D central corneal thickness.9
As such, a comparison of predicted clinical outcomes utilizing SS-OCT biometers to calculate the toric IOL power may reveal some differences. A study conducted by Melendez et al1 compared clinical outcomes using ARGOS®, the Barrett Universal II formula and the Barrett toric calculator to the predicted clinical outcomes from the IOLMaster 700 with Total Keratometry (TK) measurements and the Barrett TK Toric calculator (Figure). The cylinder prediction error of 0.5 D or less was 83.1% for ARGOS® and 76.3% for the IOLMaster 700.1 This difference however was not statistically significant. A similar, but significant, trend was noted for the refractive spherical equivalent. Using the ARGOS® resulted in a refractive prediction error of 79.7%, while that of the IOLMaster 700 was 61% (P = 0.016).1
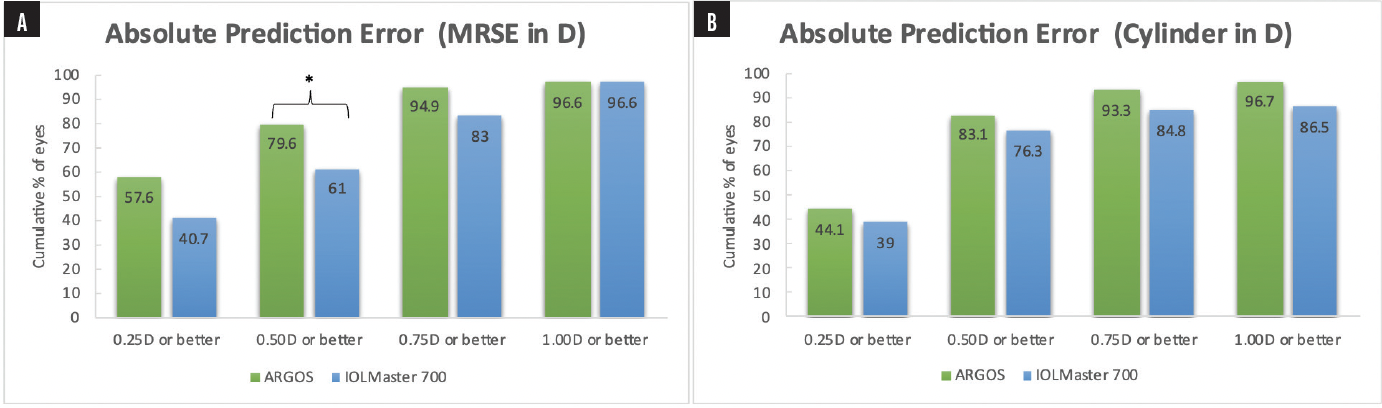
Figure. Absolute prediction error for (A) manifest refractive spherical equivalent (MRSE) in diopters and (B) cylinder in diopters.1
*Percent of eyes with MRSE of 0.5 D or better was statistically higher with ARGOS® as compared to IOLMaster 700 (P = 0.016)
Of note, the IOLMaster 700 does not directly measure the posterior corneal curvature; instead it uses the anterior corneal curvature and corneal thickness to model the posterior cornea. In this study, the extrapolated posterior corneal surface of the IOLMaster 700 did not show an improvement in refractive outcomes over using the predicted posterior cornea in the Barrett formulas.1
Conclusions
Norrby et al7 and Hirnschall et al9 examined common error sources that influence refractive outcomes in monofocal and toric IOL power calculations. While keratometry readings have a small impact on refractive outcomes in monofocal IOL power calculations,4,7,8 it constitutes the largest source for inaccuracies in toric IOL power calculations.1,9
1. Melendez RF, Smits G, Nguyen T, Ruffaner-Hanson CD, Ortiz D, Hall B. Comparison of astigmatism prediction accuracy for toric lens implantation from two swept-source optical coherence tomography devices. Clin Ophthalmol. 2022;16:3795-3802.
2. Montes-Mico R. Evaluation of 6 biometers based on different optical technologies. J Cataract Refract Surg. 2022;48(1):16-25.
3. Sabatino F, Matarazzo F, Findl O, Maurino V. Comparative analysis of 2 swept-source optical coherence tomography biometers. J Cataract Refract Surg. 2019;45(8):1124-1129.
4. Yang CM, Lim DH, Kim HJ, Chung TY. Comparison of two swept-source optical coherence tomography biometers and a partial coherence interferometer. PLoS One. 2019;14(10):e0223114.
5. Galzignato A, Lupardi E, Hoffer KJ, Barboni P, Schiano-Lomoriello D, Savini G. Repeatability of new optical biometer and agreement with 2 validated optical biometers, all based on SS-OCT. J Cataract Refract Surg. 2023;49(1):5-10.
6. Romanek J, Slukova K. Comparison of optical biometers Argos and IOLMaster 700. Cesk Slov Oftalmol. 2021;77:295-299.
7. Norrby S. Sources of error in intraocular lens power calculation. J Cataract Refract Surg. 2008;34(3):368-376.
8. Omoto MK, Torii H, Masui S, Ayaki M, Tsubota K, Negishi K. Ocular biometry and refractive outcomes using two swept-source optical coherence tomography-based biometers with segmental or equivalent refractive indices. Sci Rep. 2019;9(1):6557.
9. Hirnschall N, Findl O, Bayer N, Leisser C, et al. Sources of error in toric intraocular lens power calculation. J Refract Surg. 2020;36(10): 646-652.
IMPORTANT PRODUCT INFORMATION ARGOS® OPTICAL BIOMETER
Caution: Federal (USA) law restricts this device to the sale by or on the order of a physician.
Indication: ARGOS® is a non-invasive, noncontact biometer based on swept-source optical coherence tomography (SS-OCT). The device is intended to acquire ocular measurements as well as perform calculations to determine the appropriate intraocular lens (IOL) power and type for implantation during intraocular lens placement.
Intended Use: The Reference Image functionality is intended for use as a preoperative and postoperative image capture tool. It is intended for use by ophthalmologists, physicians, and other eye-care professionals and may only be used under the supervision of a physician.
Warnings / Precautions:
• Only properly trained personnel with experience may operate the device and control software and interpret the results.
• Factors that influence the measurement of patient’s eyes are listed in the User Manual (Table 1): pseudophakic eye, wearing contact lenses, fixation problem, cornea opacity, non-intact cornea, refractive surgery, blood in the vitreous humor, retinal detachment, keratoconus, asteroid hyalosis, ambient light in the room, and deformation of the corneal shape. Please consider the guidance provided in Table 1 when you encounter these factors.
• Optical Radiation - This device is equipped with a Class 1 laser light source.
Attention: Refer to the ARGOS® User Manual for a complete description of proper use and maintenance, optical and technical specifications, as well as a complete list of warnings and precautions.
© 2023 Alcon Inc. 06/23 US-ARB-2300049


