CASE PRESENTATION
A 75-year-old woman is referred for an evaluation of her right eye. Her surgical history is significant for hexagonal keratotomy that was performed on her right eye in 2004 and resulted in high irregular astigmatism and corneal scars (Figure 1). Other relevant associated pathologies include myopia, Fuchs corneal dystrophy, presbyopia, and cataract.
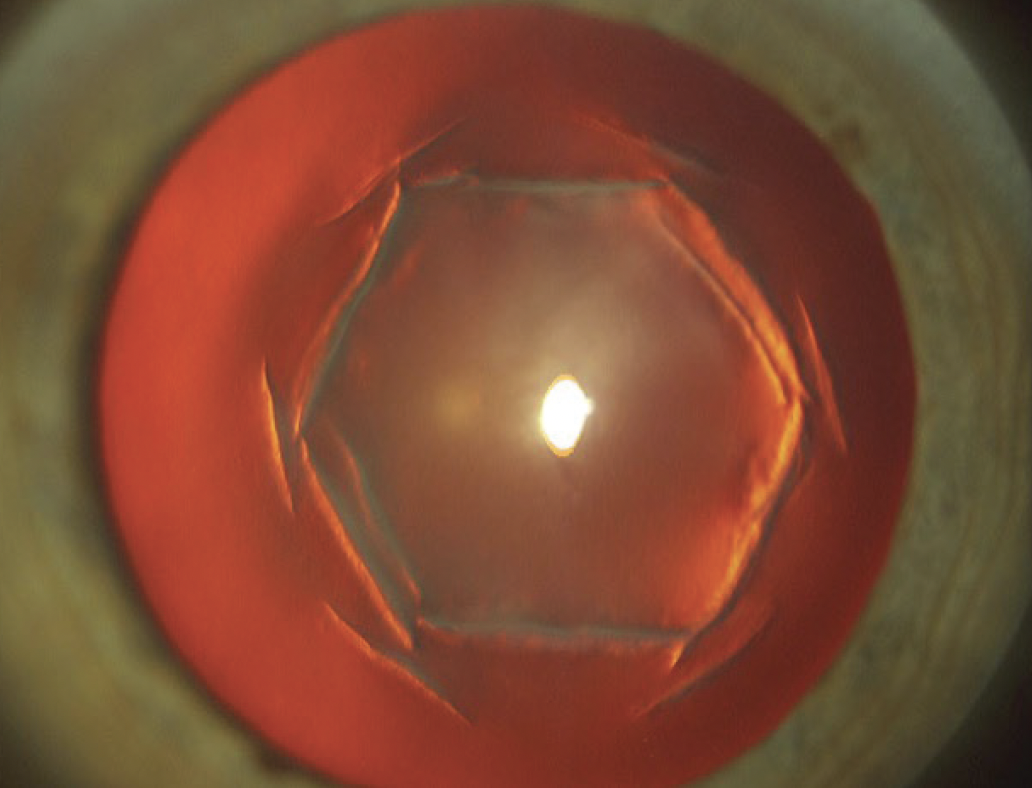
Figure 1. Corneal scars from an earlier hexagonal keratotomy.
On presentation, the patient’s UCVA is count fingers at 3 feet OD, and her BCVA is 20/400 OD. Measurements with the Pentacam AXL (Oculus Optikgeräte) indicate an ectatic cornea with keratometry readings of 88.90 D @ 111.1º and 65.50 D @ 21.1º and an apical pachymetry reading of 475 µm (Figures 2 and 3). Her visual acuity improves to 20/50 OD with pinhole testing and a retinal acuity meter (AMA Optics).

Figure 2. The right eye has high irregular astigmatism and steep keratometry.

Figure 3. Scheimpflug overview showing a cataract and high irregular corneal astigmatism in the right eye.
The patient is dissatisfied with her current vision and the adverse impact it has on her life. How would you proceed?
—Case prepared by Arun Gulani, MD, MS, DNB, FAAO, FRSH, FWCRS

JORGE L. ALIÓ, MD, PHD, FEBOPHTH, FWCRS
Practiced in the late 1980s and 1990s, hexagonal keratotomy was an aggressive and unpredictable form of corneal refractive incisional surgery that caused significant complications, particularly irregular astigmatism.1
If the patient is satisfied with her 20/50 pinhole vision OD, I would recommend a refractive lens exchange with a small-aperture IOL (IC-8 Apthera, Bausch + Lomb). An IOL calculation formula designed for eyes with a history of radial keratotomy (RK) would be used. Although hexagonal keratotomy differs from RK, the procedures adhere to the same principles of corneal deformation. Hexagonal keratotomy, however, steepens the cornea, whereas RK flattens it.
Although the implantation of an Apthera IOL is a straightforward procedure, the outcome for this patient cannot be guaranteed because centration of the lens might not correspond well to that of the corneal ectasia. Furthermore, no case series of refractive lens exchange after hexagonal keratotomy has been published that could guide IOL power selection.
Another option for the patient might be penetrating keratoplasty (PKP) followed by refractive cataract surgery approximately 9 months later—after the sutures have been removed. The IOL calculation would target correction of the residual astigmatism from the corneal graft surgery.2,3

NEDA SHAMIE, MD
Given the patient’s history of hexagonal keratotomy, very high irregular astigmatism, and Fuchs corneal dystrophy, a thorough evaluation of every comorbidity is required to decide if one or more must be addressed. An overrefraction with a rigid gas permeable contact lens could help determine if the irregular cornea is the cause of her deteriorating vision. If so, treatment of the cornea would be pursued first. The patient could consider wearing scleral lenses until surgery becomes necessary. If, however, the overrefraction does not improve her vision, the patient would be evaluated for cataracts, corneal opacification from Fuchs dystrophy or scarring, and maculopathy.
For this discussion, I will assume that the sources of the patient’s problem are her highly aberrated cornea and corneal endothelial insufficiency due to Fuchs corneal dystrophy that is severe enough to warrant treatment. In this situation, PKP is the most appropriate surgical intervention because it would address both issues. Deep anterior lamellar keratoplasty is inadvisable because it would not address the underlying endothelial pathology. I would consider performing a femtosecond laser–enabled PKP using a zigzag pattern if the hexagonal incisions are within the margins of that pattern. I favor this approach because I find it improves wound apposition, speeds healing, and smooths the contour of the graft-host junction.
During the PKP, a 24-bite running continuous suture would be used to manage postoperative astigmatism. The suture could be adjusted within the first 3 months to fine-tune the patient’s astigmatism as needed. Full suture removal would be considered 12 to 18 months after the PKP once wound healing has stabilized. Cataract surgery would be planned after the corneal measurements have stabilized. A toric IOL would be implanted if the eye has 4.00 D of regular astigmatism or less. If the eye has greater than 4.00 D of regular corneal astigmatism, astigmatic keratotomies would be performed to lower the amount of cylinder to within the range of a toric IOL, and surgery would proceed after the eye stabilizes. If the eye has irregular astigmatism, either an IC-8 Apthera or a monofocal IOL would be implanted, and the patient would be fitted with a scleral or rigid gas permeable contact lens postoperatively.
This stepwise approach to management is key to achieving optimal results for this patient. Cases this complex are among the most rewarding because a successful outcome has the potential to transform the patient’s quality of life.

BLAKE WILLIAMSON, MD, MPH, MS
First, a scleral contact lens fitting would be attempted. If the patient can tolerate this form of correction, I believe cataract surgery with a monofocal IOL followed by scleral contact lens wear would provide her with the best possible quality and quantity of vision.
If the patient is highly motivated to reduce her dependence on spectacles and contact lenses, a small-aperture IOL could be considered. I would proceed cautiously, however, and emphasize preoperatively that the large swing in astigmatism across the central cornea might necessitate an IOL exchange.

WHAT I DID: ARUN GULANI, MD, MS, DNB, FAAO, FRSH, FWCRS
This case typifies referrals my practice receives daily from around the world. The management strategy reflects my dedication to overcoming optical, anatomic, and physiologic complexities with the fewest interventional techniques possible to maximize the patients’ UCVA.4-6
My first surgical objective was to facilitate accurate measurements in this eye with an unstable cornea (see how the case was managed below). Paired 0.45-mm intrastromal corneal ring segments (Intacs, CorneaGen) were placed outside the hexagonal keratotomy incisions to hug the unstable corneal island (Figure 4). This intervention stabilized the cornea, reduced the amount of astigmatism from 23.50 to 1.40 D, and improved the keratometry reading from 88.90 to 62.70 D. CXL was then performed to reinforce the cornea and secure the achieved contour.7-9

Figure 4. Intrastromal corneal ring segments are placed to help stabilize the cornea before cataract surgery.
(Figures 4–6 courtesy of Arun Gulani, MD, MS, DNB, FAAO, FRSH, FWCRS)
After the eye demonstrated refractive stability for 4 months, cataract surgery was performed. A small capsulorhexis was created to maintain the clear central optical zone and stable lens capsule diaphragm and prevent postoperative rotation of the IOL.10 A toric lens was implanted to correct the patient’s ametropia and astigmatism (Figure 5). The cataract incision was secured without sutures to minimize surgically induced astigmatism and reinforced with ReSure Sealant (Ocular Therapeutix; product not currently being produced).

Figure 5. The eye after cataract surgery.
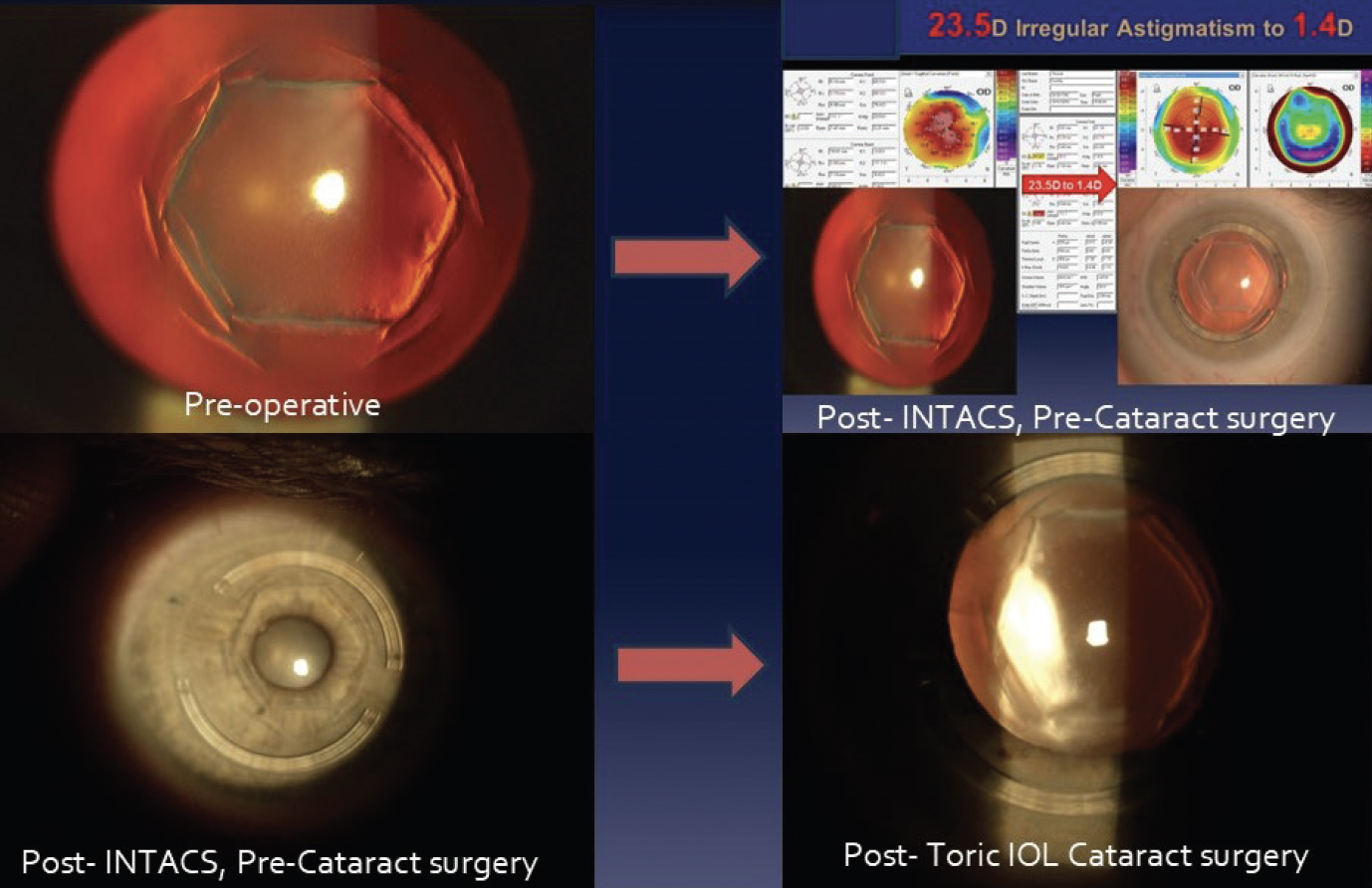
Figure 6. Staged approach to unaided vision summarized.
Postoperatively, the patient’s UCVA was 20/25- OD. This outcome underscores the effectiveness of approaching seemingly insurmountable challenges with an unshakable focus on unaided vision, using the smallest number of interventional techniques, and even employing staged techniques (Figure 6) when addressing complex corneal and refractive conditions in accordance with the principles of Corneoplastique11 to restore the patient’s lifestyle.12
1. Basuk WL, Zisman M, Waring GO 3rd, et al. Complications of hexagonal keratotomy. Am J Ophthalmol. 1994;117(1):37-49.
2. Xie K, Wang L, Koch DD. Cataract surgery in previous refractive corneal surgery cases. In: Alió JL, Dick HB, Osher RH, eds. Cataract Surgery: Advanced Techniques for Complex and Complicated Cases. Springer; 2022:157-164.
3. Lovisolo CF, Renna A, Alió JL. Complications of refractive keratotomy. In: Alió JL, Azar DT, eds. Management of Complications in Refractive Surgery. 2nd ed. Springer; 2018:347-382.
4. CLEAR a new concept in refractive surgery. Ocular Surgery News. April 2018. Accessed November 11, 2024. https://www.healio.com/news/ophthalmology/20180426/video-clear-a-new-concept-in-refractive-surgery
5. Gulani AC. Vision à la carte: designing vision. Ophthalmology Times. September 15, 2013; 38(18):31-33. Accessed November 11, 2024. https://www.ophthalmologytimes.com/view/vision-la-carte-designing-vision
6. Gulani A. Introducing the Gulani Planning System. EyeWorld. August 2017. Accessed November 11, 2024. https://digital.eyeworld.org/i/853444-aug-2017/30?
7. Gulani AC. Keratoconus: thinking outside the cone. Ophthalmology Times. October 1, 2016. Accessed November 11, 2024. https://www.ophthalmologytimes.com/view/keratoconus-thinking-outside-cone
8. Gulani AC. Shaping the future and reshaping the past: the art of vision surgery. In: Copeland and Afshari’s Principles and Practice of Cornea. 1st ed. Jaypee Brothers Medical Publishers; 2013:1252-1273.
9. Gulani AC. Think outside the cone: raising keratoconus surgery to an art. Advanced Ocular Care. November/December 2010:35-37.
10. Gulani AC. Refractive surgery presentation spotlight: making a lens work (premium lens implant success). EyeWorld. 2018;23(1):68.
11. Gulani AC. Corneoplastique: art of vision surgery. Indian J Ophthalmol. 2014;62(1):3-11.
12. Gulani AC. Show me the patients: patient satisfaction, not surgical landmarks or chart indices, mark of success. Ophthalmology Times. April 20, 2020. Accessed November 11, 2024. https://www.ophthalmologytimes.com/view/show-me-patients-patient-satisfaction-not-surgical-landmarks-or-chart-indices-mark-success




