
As Arjan Hura, MD, advanced through his training and early years in ophthalmology, he noticed a lot of his mentors and older colleagues discussing the same thing: the importance of starting early in establishing good surgical ergonomics. As he explains to host I. Paul Singh, MD, in this episode of Innovation Journal Club, being proactive about proper health and wellness is an investment in longevity: you don’t have to be old to get injured from repetitive muscular stress.
How He Got Involved in Research
Like many undergraduate students who intend to apply to medical school, Dr. Hura knew his CV would benefit from experience with research. A family friend who was a nephrologist invited Dr. Hura to help with nephrology research in his lab one summer. That exposure gave Dr. Hura insight into how an MD/PhD runs a lab, in addition to gaining experience with immunohistochemistry and histology.
After his first year in medical school, an opportunity to assist with pediatric pulmonology research at the Cincinnati Children’s Hospital exposed Dr. Hura to multi-industry collaboration. His team met weekly with engineers, sleep scientists, pulmonologists, statisticians, and other specialists. He also saw clinical patients.
“I got to see the procedures that were being done in the OR, and then I was back in the lab. I got to see that whole translational aspect of research,” he explained to Dr. Singh.
It wasn’t until his third year of medical school that Dr. Hura decided to pursue ophthalmology, yet he had no contacts in the field whom he could approach about research opportunities. After sending cold e-mails to many individuals, one responded with a timely opportunity—Robert Osher, MD. Then, prior to starting his internship year in Columbus, OH, Dr. Hura reached out to Alice Epitropoulos, MD, whose talk on IOL optics he’d previously attended as a medical student, and she offered him a chance to do research in dry eye disease.
Studying Ergonomics in the OR
Throughout his medical training and now as a practitioner, Dr. Hura said he has heard innumerous talks on the ergonomics of performing surgery. As he told Dr. Singh, “I noticed that it was always people older than me giving these talks, and they also made the same points: You have to start early, and you have to be diligent about the measures you’re taking to protect your body.” Dr. Hura notes that several studies have concluded that 40% to 80% of ophthalmologists will be impacted by cervical or lumbar pain that will interfere with their ability to work.1-7 In 2019, at the annual meeting of the AAO, Dr. Hura attended a Learning Lounge panel discussion that included Chris Riemann, MD, one of his retina attending physicians at the Cincinnati Eye Institute. Dr. Riemann advocated using the 3D heads-up display to perform ocular surgery for ergonomic benefits. Afterward, Dr. Hura and Dr. Riemann were talking. “And I just happened to wonder out loud if anyone has looked at 3D heads-up display with EMG. And you know Chris, he was game.”
Dr. Hura found no papers in the ophthalmic literature in which researchers had quantified median amplitude EMG signals for specific muscle groups while a subject was performing surgery. So, Dr. Hura and Dr. Riemann conducted an investigator-initiated clinical method study in which electrodes were placed on Dr. Riemann’s back over a 4-day period to learn which muscles were being stimulated during surgery. On one day, Dr. Riemann operated using the operating microscope exclusively; on another day, he exclusively used a 3D heads-up display. Plus, there were two crossover days, where Dr. Riemann would use one method in the morning and the other method in the afternoon. All four days were spaced about 1 week apart. When Dr. Riemann used the 3D heads-up display, most muscle groups measured showed a reduction in amplitude compared to when he operated with the traditional microscope (Figure 1). Anecdotally, he also reported experiencing less fatigue.
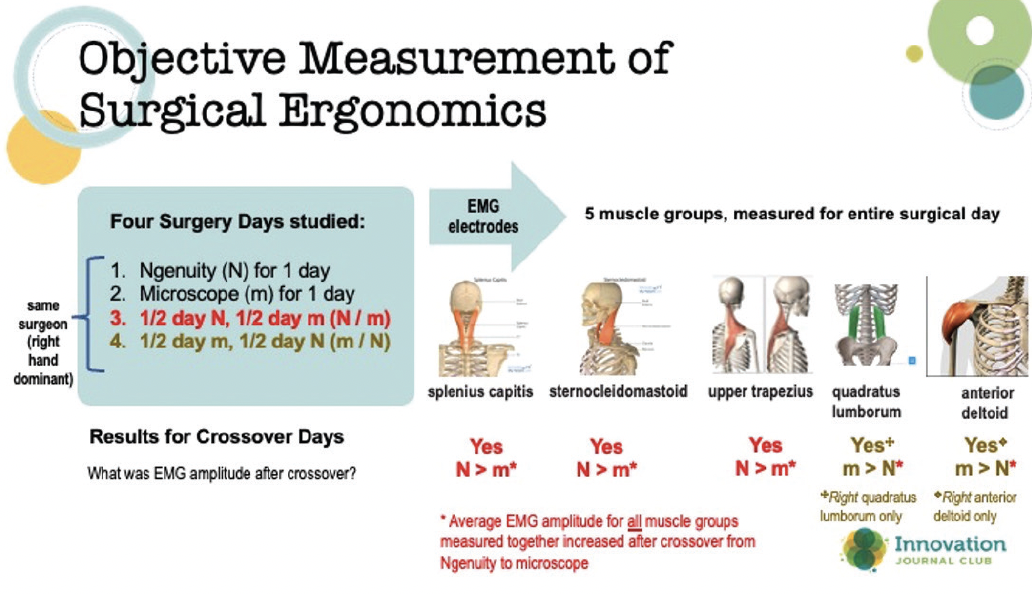
Figure 1. Overview of a clinical method study in which EMG amplitude was measured on a single surgeon using either a microscope or heads-up view, as well as on crossover days from one viewing method to the other.
Although Dr. Hura has submitted this study’s data for publication, he plans to continue the research. “Eventually, I’d like to compile the footage of him [performing surgery] from posterior to anterior and laterally that was recorded in 4K on tripods in the operating room … into a four-split-screen view. I’d like to be able to demonstrate how he’s moving in space, what his hands are doing, and what muscles are firing with each motion.”
1. Chatterjee A, Ryan W, Rosen E. Back pain in ophthalmologists. Eye. 1994;8:473-474.
2. Al-Marwani, Al-Juhani M, Khandekar R, et al. Neck and upper back pain among eye care professionals. OccupMed (Lond). 2015;65(9):753-757.
3. Dhimitri KC, McGwin G Jr, McNeal SF, et al. Symptoms of musculoskeletal disorders in ophthalmologists. Am J Ophthalmol. 2005;139(1):179-181.
4. Hyer JN, Lee RM, Chowdhury HR, et al. National survey of back & neck pain amongst consultant ophthalmologists in the United Kingdom. Int Ophthalmol. 2015;35(6):769-775.
5. Chams H, Mohammadi SF, Moayyeri A. Frequency and assortment of self-report occupational complaints among Iranian ophthalmologists: a preliminary survey. Med Gen Med. 2004;6(4):1.
6. Kaup S, Shivalli S, Kulkarni U, Arunachalam C. Ergonomic practices and musculoskeletal disorders among ophthalmologists in India: An online appraisal. Eur J Ophthalmol. 2020;30(1):196-200.
7. Kitzmann AS, Fethke NB, Baratz KH, et al. A survey study of musculoskeletal disorders among eye care physicians compared with family medicine physicians. Ophthalmology. 2012;119(2):213-220.
