On February 28th, during the 2020 American Glaucoma Society Meeting, Novartis Pharmaceuticals hosted a panel discussion titled, “Innovation in Patient Access to Branded Therapy.” Panelists Gregory J. Katz, MD; James Katz, MD; and Robert J. Noecker, MD, MBA, shared their thoughts and experiences with a new program from Novartis.
What are some struggles that you’ve faced over the last few years with respect to getting a branded prescription?
Dr. James Katz: In our practice, it’s been about call-backs. We receive so many call-backs for medications when we prescribe branded products. Patients try to get the medications, and they’re not covered by insurance or they’re too expensive, so they come back to us for second choices and sometimes third choices. So, we don’t get the same medications we expect our patients to use.
“Call-backs have really slowed down the process in our office.”
— DR. JAMES KATZ
Dr. Gregory J. Katz: Call-backs are a tremendous problem. Filling out prior authorizations, which you often have to do for medications that aren’t covered, is just a very time-consuming process. Often, we’ll fill out a prior authorization and sometimes it won’t get accepted. Then we’ll fill out another prior authorization and finally it gets accepted, but then the cost is just unacceptably high for the patient. There’s so much uncertainty. My patient will often ask me, ‘So, how much is this going to cost?’ And typically, I’ll just tell them, ‘I have no idea, because every plan is so different.’ And these are the frustrations that we’re going through.
Dr. Robert J. Noecker: I don’t want to spend my time with a patient talking about how much they paid the last time for their medication. I want to talk about their disease and see how they’re doing. But I find that, more and more, I’m hearing, ‘I paid this when I went to the pharmacy.’ I like to always think that I’m recommending the best drug when I prescribe something. Then I can say, ‘Okay, now I’ll give you the second-best drug, and I hope you don’t have a problem with it.’
Dr. James Katz: That’s right. We try to use the products that we think are best, and there is some loss of confidence when we switch over to another category for the patient.
Any other issues you face in prescribing branded medication? Any solutions you’ve tried to get around these issues?
Dr. Gregory J. Katz: We found co-pay cards useful. But they’re hard or almost impossible to use on Medicare or Medicaid patients. And even on the commercial patients, depending on what pharmacy they go to, if the pharmacist isn’t very familiar with the card or doesn’t want to deal with it, we get a lot of call-backs on that.
“There’s a lot of frustration with all of this stuff for us.”
— DR. GREGORY J. KATZ
Dr. Robert J. Noecker: I really like the co-pay card programs, but for us, because of the way our state government is, a lot of our patients are Medicare patients, so they can’t use it.

Figure 1. Program benefits of MyChoiceRx.
Can you talk about the experiences you’re having in your practices with MyChoiceRx?
Dr. Gregory J. Katz: We have had no prior authorizations that we’ve needed to do. I’ve had no patients that have not been able to get the medicine through this program. We’ve had very limited call-backs. And when the patients ask, ‘How much is this going to cost?’ we know exactly how much it’s going to cost.
Dr. James Katz: I know my patients are going to pay no more than $60 for Durezol (Novartis) or Ilevro (Novartis), and those are the products I use. There’s a comfort for us in telling a patient that, and it’s quick. In our practice it’s about workflow, keeping it efficient, and moving on. (Figures 1 and 2).
Dr. Robert J. Noecker: It gives a bit of predictability.
“The whole process for us is very easy because the technician just e-prescribes it through ScriptHero, and we don’t have to deal with it again.”
— DR. GREGORY J. KATZ
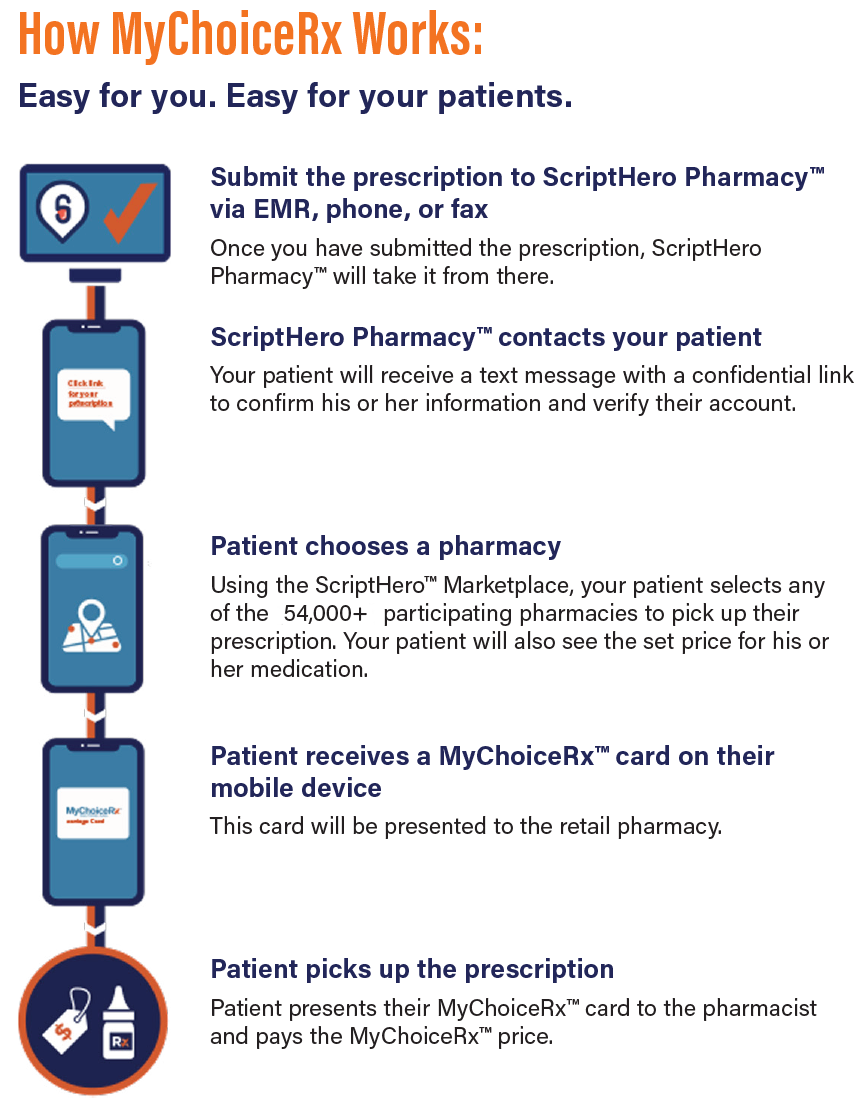
Figure 2. The MyChoiceRx process.
What are some of the results you’ve had with MyChoiceRx?
Dr. Gregory J. Katz: I used ScriptHero 57 times, and I’ve had 12 patients fill the prescription. Most of these patients already had multiple bottles of their medication at home, so they didn’t need the prescription. However, I sent the prescription into ScriptHero Pharmacy so they could get set up with the system, and I think the majority of these patients are going to be using it in the future.
Dr. James Katz: We sent 56 prescriptions to the ScriptHero pharmacy, and almost all of them (51) were filled. And again, these are products that are one-time products, surgical products. So, when I prescribe them, they’re getting them that time. Our call-backs went down to only one out of the 56, and that was at the beginning.
Dr. Robert J. Noecker: We find that patients like it. It has cut down on the number of call-backs and problems. Although, once again, it’s unusual how certain people’s insurance works. But we’ve found that patients actually did better buying at the pharmacy, and that’s what most of the patients chose to do.
Do you have any closing thoughts?
Dr. James Katz: I think patients see this as, we’re advocates for them, so it works out both ways. We are trying to deliver the correct medications, or the ones we believe in, to our patients at the best price we can. We’re doing it in an efficient manner for our patients.
“MyChoiceRx has been a big win-win process for us and our patients, making it easier for our office and helping patients get the medicines that we want them to get at an affordable price.”
— DR. GREGORY J. KATZ

“We want to keep our staff happy and our patients happy, so I think it works out well for everyone.”
— DR. JAMES KATZ
The speakers were paid by Novartis Pharmaceuticals Corporation (NPC) to conduct this presentation.

Novartis Pharmaceuticals Corporation
East Hanover, New Jersey 07936-1080
© 2020 Novartis
9/20
T-AAF-1394215



