A change in coding and reimbursement for MIGS procedures implemented in January 2022, which resulted in a 90% reduction in reimbursement for all trabecular meshwork bypass stenting procedures, appears to have driven an increase in canal-based procedures and a decrease in angle-based procedures after the cuts were implemented.1
An analysis of national claims data from a 5% sample of all Medicare beneficiaries compared glaucoma procedure counts between the first quarter of 2021 and the first quarter of 2022.1 According to the investigators, the utilization of angle-based stenting procedures, including the Hydrus Microstent (Alcon) and iStent (Glaukos), decreased by about 20,960 procedures between 2021 and 2022.1 As well, there were increases in goniotomy procedures by an estimated 11,680 cases and canaloplasty procedures by about 6,640 cases between the 2 years (Figure 1).1 Taken together, these data suggested a shift in procedural selection among ophthalmic surgeons, which was most likely driven by coding and reimbursement changes implemented in January 2022.1
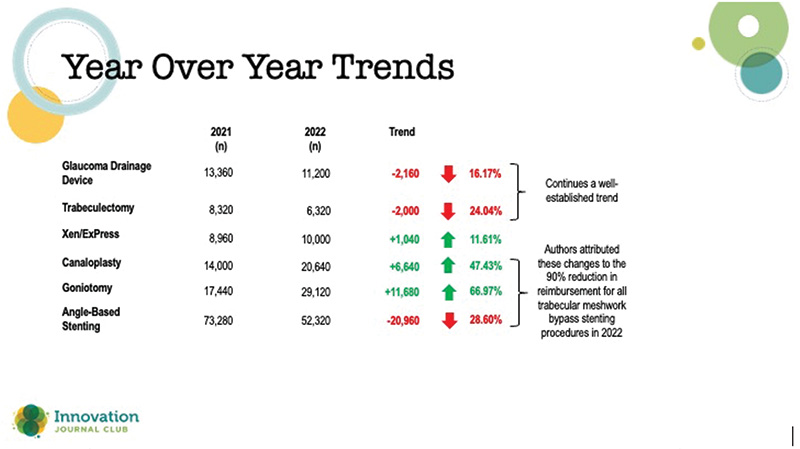
Figure 1. Comparisons in procedural counts in 2021 and 2022 in an analysis of national claims data from a 5% sample of all Medicare beneficiaries.
While it is unclear what impact the shift in procedural choice had on patients’ outcomes, the analysis nevertheless points to the effects of the evolving reimbursement landscape on physician behavior.
“[As human beings], we are driven by different factors. One is innovation, one is what the patient needs, and one is reimbursement because this is our job,” said Dr. Bedrood, commenting on the results. “When that changes, it changes our behavior; that's what the study showed.”
There may be additional insurance issues providers will need to be mindful of. For example, a new local coverage determination that became effective in November 2024 restricts reimbursable procedures to cataract plus one stent device per eye, effectively ending reimbursement for combination MIGS procedures. Fundamentally, these kinds of changes challenge physicians to continue making decisions that are in the best interest of patient care in the context of various financial rules non-physicians implement.
“The onus is really on us as physicians to act responsibly, to not overuse certain codes. I think there's also an onus on both industry and doctors to give data,” Dr. Bedrood concluded. “Without that, we are not going to be able to reverse any of these things. There is a responsibility on our behalf to help ourselves and help our patients.”
1. Williams PJ, Hussain Z, Paauw M, et al. Glaucoma surgery shifts among Medicare beneficiaries after 2022 reimbursement changes in the United States. J Glaucoma. 2024;33(1):59-64.

