Imagine that your familiar car—the one you have driven for years—starts to give you trouble. It is losing reliability or performance and can no longer carry you through life’s routines comfortably. You are in the market for an upgrade. Then, you hear a worldwide decree: the next car you buy must last you the rest of your life. Now, consider your hesitation when the sales representative suggests choosing your forever car without a test drive, even just around the lot.
This is essentially what happens when cataract surgery and refractive lens exchange patients are asked to select a forever IOL without the benefit of a “test drive.” This reality can push both patients and surgeons to make overly conservative choices, make informed consent suboptimal, and, in some instances, lead to regret. It also risks the following dreaded remarks: I never expected it to be like this, and I’m not happy.
During the 2024 ESCRS meeting in Barcelona, Spain, my friend Anaïs Nicolas, a clinical psychologist from Nantes, told an audience, “Any surgical procedure can be psychologically traumatic, even when everything goes smoothly from the surgeon’s perspective.” Cataract and refractive surgeons are entrusted with patients’ most precious sense as they lie beneath the surgical drapes. When they open their eyes and emerge from this cocoon of transformation, they may feel distress if their new view of the world differs from what they expected, and that distress can lead to regret—an outcome no one wants.
Put simply, a mismatch between expectations and outcomes can create a perceived loss of control among patients, which may foster regret. By contrast, effective preoperative simulation can promote a sense of agency, support cognitive ownership, and help patients feel they have shared in the success of the outcome.
ENTER VISION SIMULATION
Vision simulators encompass a range of tools—from simple visual depictions to digital IOL simulators, binocular wearable devices, and real-world trials such as with contact lenses or staged surgery. Each aims to improve patients’ understanding of possible outcomes and strengthen their sense of agency.
I have found that, when patients take an active role in decision-making, they tend to be better informed, more invested in the choice, and less likely to regret it.
DIGITAL IOL SIMULATORS
Every patient I evaluate for IOL implantation receives education with brand-agnostic tools such as the Rendia platform (Rendia), which uses computer-generated images to depict how the world may appear through different IOL designs. These tools can help us explain what the terms halos, glare, and starbursts mean and set expectations in real-world scenarios, most notably night driving. In my view, this type of visualization is essential to effective counseling for advanced-technology IOLs. At a minimum, we should show patients an image that approximates glare from oncoming headlights at night.
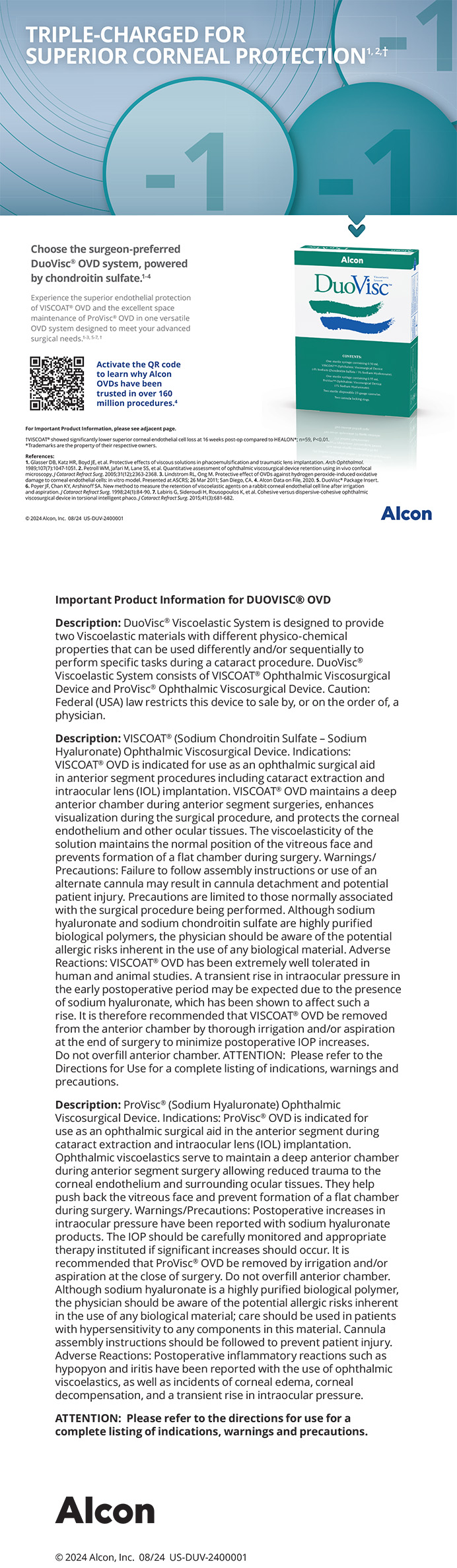
Many IOL manufacturers offer digital or online vision simulators (Figures 1–3).1-3 I have used several of these and find them reliable and efficient for demonstrating how different IOL designs are expected to perform and which optical side effects may accompany a given choice. That said, I find brand-agnostic simulators less distracting during counseling. The latter tools integrate smoothly into the consultation, support a natural discussion of IOL selection, and highlight clear differences among IOL options.

Figure 1. Johnson & Johnson Vision IOL simulator.
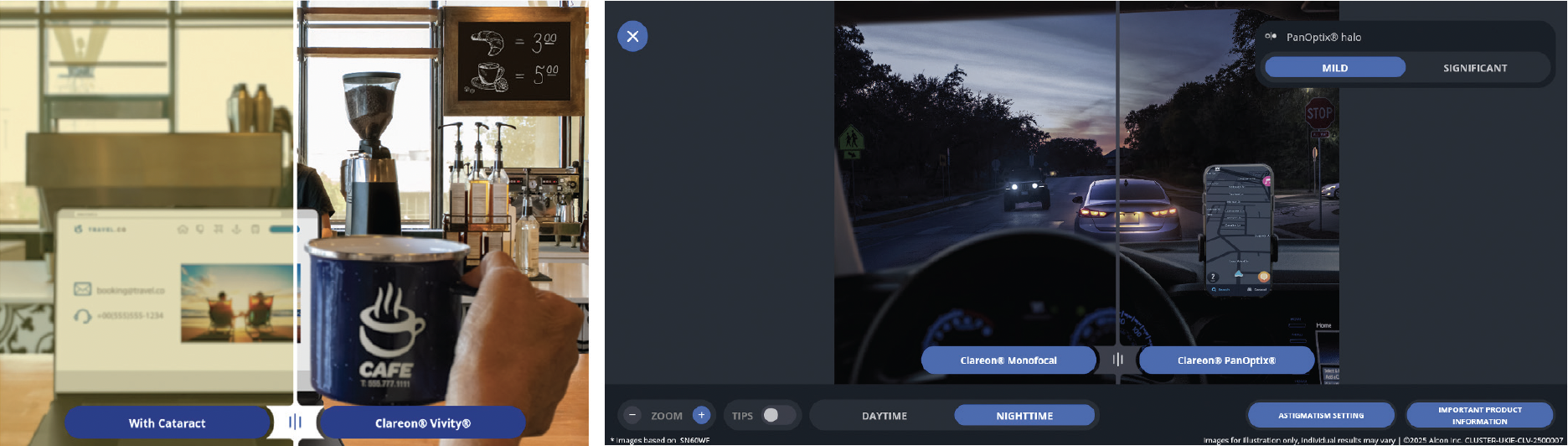
Figure 2. Alcon Vision Educator.
Figure 3. Rayner GalaxyIOL education tool.
BINOCULAR WEARABLE SIMULATION
A picture is worth 1,000 words, but a wearable simulation may be worth far more. The most powerful preoperative surgical simulator I have used thus far is the SimVis Gekko (2EyesVision; Figure 4). This wearable device demonstrates binocular visual performance by replicating the through-focus performance of various IOLs. The simulator allows patients to rate their satisfaction with their near and distance visual acuity and to experience differences in glare, contrast sensitivity, and dysphotopsias with various IOL designs before undergoing surgery.

Figure 4. SimVis Gekko 2.0.
Although integrating a binocular, mobile simulator into the clinical practice can be challenging—particularly with respect to clinician time and patient flow—giving patients an opportunity to see what they might experience after surgery can create a meaningful psychological bridge between their pre- and postoperative visual experiences. Reassuringly, Barcala et al reported that the presence of a cataract did not alter IOL preferences demonstrated with the SimVis Gekko.4
In my day-to-day clinical practice, I routinely use Rendia’s brand-agnostic vision demonstrator to help counsel patients on their IOL options. I reserve the SimVis Gekko2 for those who need a more in-depth simulation to aid decision-making for two reasons. First, the evaluation can take an optometrist out of clinic for at least 20 minutes. Second, some patients find the headset distracting.
REAL-WORLD TRIALS
Contact Lenses
I regularly use contact lens trials for elective IOL patients. The opportunity to test different levels of blended vision or to compare blended vision with multifocality in their own environments helps them feel confident in their decisions.
Patients can evaluate how their vision feels during real-world activities such as playing badminton, attending orchestra rehearsals, chairing a meeting, and driving at night. This immersive experience equips them to provide meaningful feedback, supports their agency and ownership of refractive targets, identifies potential difficulties in advance, and, ultimately, enhances their postoperative satisfaction.
Contact lens trials, however, can be challenging for some patients and time-consuming for administrative staff. A clear process and pathway are therefore necessary to maximize the trials’ effectiveness.
Staged Surgery or Custom Match
What if we could offer patients a real-world test drive of multifocality?
If a patient is anatomically suitable for a diffractive multifocal IOL and has the motivation to pursue a high degree of spectacle independence, staged surgery (also known as custom match) can leverage the brain’s preference for one eye over the other as a practical, real-world simulator.
The sensory nondominant eye receives a diffractive trifocal IOL first. The second eye is typically scheduled to undergo surgery about 1 week later. During that interval, the patient is encouraged to take the new lens for a spin. For example, I ask patients to ride as passengers during nighttime drives and rate their dysphotopsias. I also ask them to take note of their distance, intermediate, and near performance and whether their experiences improve over the ensuing days.
When the time comes for lens replacement surgery in the dominant eye, the patient’s lived experience becomes the key data point guiding IOL selection. If they are satisfied, a trifocal IOL is implanted in the dominant eye. If dysphotopsias are too bothersome, a nondiffractive increased range of focus IOL is selected for the dominant eye. Because many patients naturally partially suppress the nondominant eye, this strategy may reduce binocular optical side effects while still providing near vision from the first trifocal IOL.
FINAL THOUGHTS
Expectation management is a clinical intervention. The goal of vision simulators is to help patients avoid unwanted surprises and regret by setting realistic expectations preoperatively. Although available simulators share this objective, the devices vary in how accurately they replicate IOLs’ real-world visual performance.
For many patients, a digital comparison is sufficient to communicate the key trade-offs among IOL designs. Other patients benefit from a more immersive simulation that provides them with greater clarity and confidence in selecting the option that best aligns with their priorities. Ultimately, patients should understand what they are choosing and feel actively involved in the decision-making process. This shared understanding protects everyone involved and, in my experience, tends to yield greater satisfaction among patients and clinicians, even though additional time and effort are required.
1. Alcon. Vision Educator. Accessed January 26, 2026. smarteducator.myalcon.com
2. Johnson & Johnson Vision. IOL Simulator. Accessed January 26, 2026. jnjvisionpro.eu/simulator
3. Rayner. GalaxyIOL Vision Simulator. Accessed January 26, 2026. galaxyiol.com/vision-simulator
4. Barcala X, Zaytouny A, Rego-Lorca D, et al. Visual simulations of presbyopic corrections through cataract opacification. J Cataract Refract Surg. 2023;49(1):34-43.