CASE PRESENTATION
A 47-year-old man presents for a refractive surgery consultation. Over the past 2 years, the patient’s hyperopia has progressively increased, necessitating multiple updates to his contact lens prescription. He reports asymmetric visual function, longstanding subjective blurring in the right eye, and a growing intolerance of both contact lenses and spectacles. His ocular and medical history is otherwise unremarkable.
The patient discontinued wearing contact lenses 1 week before presentation. Upon assessment, his UCVA is 20/350 OD and 20/200 OS. His BCVA is 20/50 with a manifest refraction of +12.00 -0.75 x 035º OD and 20/20 with a manifest refraction of +11.50 -1.50 x 040º OS. Pupillary response time is sluggish in the right eye and rapid in the left eye. A slit-lamp examination reveals a mild papillary conjunctival response and peripheral corneal neovascularization in both eyes, consistent with long-term contact lens wear. The central corneas are clear, and mild nuclear sclerosis is evident bilaterally. A dilated fundus examination of each eye is normal.
The patient, a former semiprofessional soccer player and current marathon coach, has a highly active lifestyle. He expresses a strong desire for independence from spectacles and contact lenses during physical activity. How would you proceed?
— Case prepared by Jonathan Solomon, MD, FACS

DAVID A. GOLDMAN, MD
First, I would seek to confirm that amblyopia accounts for the visual acuity and pupillary reaction in the patient’s right eye through a thorough history and/or ancillary testing. If questions remain, a neuro-ophthalmologist would be consulted. Assuming the right eye is somewhat amblyopic and no other pathology is detected, the only option for vision correction would be refractive lens exchange (RLE). The amount of hyperopia is too great to manage with LASIK, PRK, keratorefractive lenticule extraction, or phakic IOL implantation. Additionally, the mild nuclear sclerosis would shorten the effect of any option other than RLE.
Given the conjunctival papillary response and corneal neovascularization, treatment with topical cyclosporine would be initiated to optimize the ocular surface before surgery. Corneal topography and pachymetry would be performed, both to ensure the measurements are in a normal range and to determine whether laser refractive surgery would be an option should RLE result in a refractive surprise.
The only options for minimizing the patient’s postoperative dependence on spectacles and contact lenses would be an extended depth of focus or multifocal IOL. Several studies have demonstrated success with multifocal lenses in patients with amblyopia.1,2 Because he does not have visually significant cataracts at this time, a contact lens trial with a low-add multifocal and a small-offset monovision trial, with the amblyopic eye set for near vision, would be conducted. His level of satisfaction with each trial would help guide IOL selection.
The choice of lens, however, might also be influenced by the power required. If it is too high for a currently available multifocal IOL to correct and space in the patient’s eyes allows, I would consider implanting both a multifocal IOL and a piggyback lens. In this scenario, if pupillary dilation is adequate, I would also consider the option of implanting a multifocal lens in the bag and a Light Adjustable Lens (LAL; RxSight) in the sulcus because optical biometry can be less accurate in short eyes. The LAL features a silicone-based optic, so the risk of intralenticular opacification would be minimal.

SUMITRA S. KHANDELWAL, MD
Before addressing the patient’s refractive goals, I would seek to understand why his vision is changing and why it is so poor. Although he is old enough to begin losing accommodation, the right eye’s 20/50 BCVA and sluggish pupillary response raise concern over potential optic nerve pathology.
Topography would be obtained because long-term contact lens wear can cause corneal warpage and irregular astigmatism. Additionally, gonioscopy would be performed to examine the angle anatomy. The patient may have narrow angles or peripheral anterior synechiae in the angle due to intermittent angle closure. This would indicate a medical reason to consider a procedure such as cataract surgery, although a laser peripheral iridotomy would be a conservative start. OCT of the retinal nerve fiber layer would be obtained to determine the status of the optic nerve.
RLE would be an option in this situation, but lens surgery on short eyes is associated with an increased risk of choroidal detachment and posterior pressure. Biometry would reveal whether the patient’s hyperopia is axial. If the axial length is less than 21 mm, rather than RLE, I would recommend scleral contact lens wear, which could improve his visual acuity with less limbal toxicity than his current soft contact lenses. If the axial length is not short enough to raise concern about ophthalmic complications such as a choroidal hemorrhage and the patient understands the risks, then lens-based surgery could be considered, especially if the angles are narrow. IOL selection would be challenging because of the high correction required. To achieve the patient’s goals, it would be necessary to implant a piggyback IOL. A combination of an acrylic one-piece IOL in the bag with a silicone lens such as the LAL would be an excellent choice. Postoperatively, it would be important to monitor him for uveitis-glaucoma-hyphema syndrome because the anterior chamber is likely shallow and the LAL is a thick lens.

KJELL U. SANDVIG, MD, PHD
The patient’s right eye likely has some degree of amblyopia (amblyopic pupillary reflex). No information on axial length, anterior chamber depth, or lens thickness is provided, so microphthalmos and nanophthalmos cannot be excluded.
Because laser treatment and phakic IOL implantation are generally unsuitable for eyes with high hyperopia, RLE is the remaining alternative for this patient, who desires independence from glasses and contact lenses during physical activities, but this procedure is associated with increased peri- and postoperative risks in very short eyes. On the other hand, RLE would eliminate the risk of angle-closure glaucoma.
The patient’s progressive hyperopia might not be a true increase but instead due to increasing decompensation. Ideally, this would be confirmed by a cycloplegic refraction over a certain period. If his binocular vision is good or nonexistent, he might benefit from a slightly myopic target (eg, -1.50 D) in the right eye. If he has binocular vision but it is weak, emmetropia would be targeted in both eyes.
My preference would be a one-piece hydrophobic acrylic IOL, possibly a toric model if more than 0.75 D of corneal astigmatism is present. IOL calculations would be performed with either the Haigis or Kane formula. I would advise against presbyopia-correcting IOLs in this unique, high-risk situation.
I would perform delayed sequential RLE, starting with the right eye, to gain experience with perioperative conditions and postoperative refractive accuracy. I would instill a dispersive OVD to protect the cornea during phacoemulsification and would attempt to limit perioperative pressure variations as much as possible to prevent choroidal effusion.

STEFANIE SCHMICKLER, MD
Because both eyes have mild nuclear sclerosis and the pupillary reaction in the right eye is sluggish, amblyopia cannot be the reason for the poor visual acuity in the patient’s right eye. Before planning any surgical intervention, further evaluation of the right eye is required. OCT of the optic disc and visual evoked potential testing would be performed to determine whether there is a problem with the optic nerve or visual pathway. Provided that no problems are identified, I would offer the patient RLE but would emphasize that his visual acuity in the right eye may not improve. I would counsel him to expect to gain independence from spectacles and contact lenses only for distance.
No information on angle kappa or higher-order aberrations is provided, so I would not recommend a trifocal or extended depth of focus IOL. Furthermore, I would assume that no premium lens is currently available that could fully correct the patient’s high hyperopia. Instead, I would select an aspheric IOL such as a CT Asphina (Carl Zeiss Meditec), C-flex or Superflex (Rayner), or Akreos AO (Bausch + Lomb). A monovision strategy might improve his range of focus if RLE improves the visual acuity in his right eye.

WHAT I DID: JONATHAN SOLOMON, MD, FACS
The longstanding blur, sluggish pupillary response, manifest refraction, and lack of 20/20 visual potential in the patient’s right eye prompted further questioning. He stated that the right eye had always been weaker. Mild amblyopia was therefore suspected.
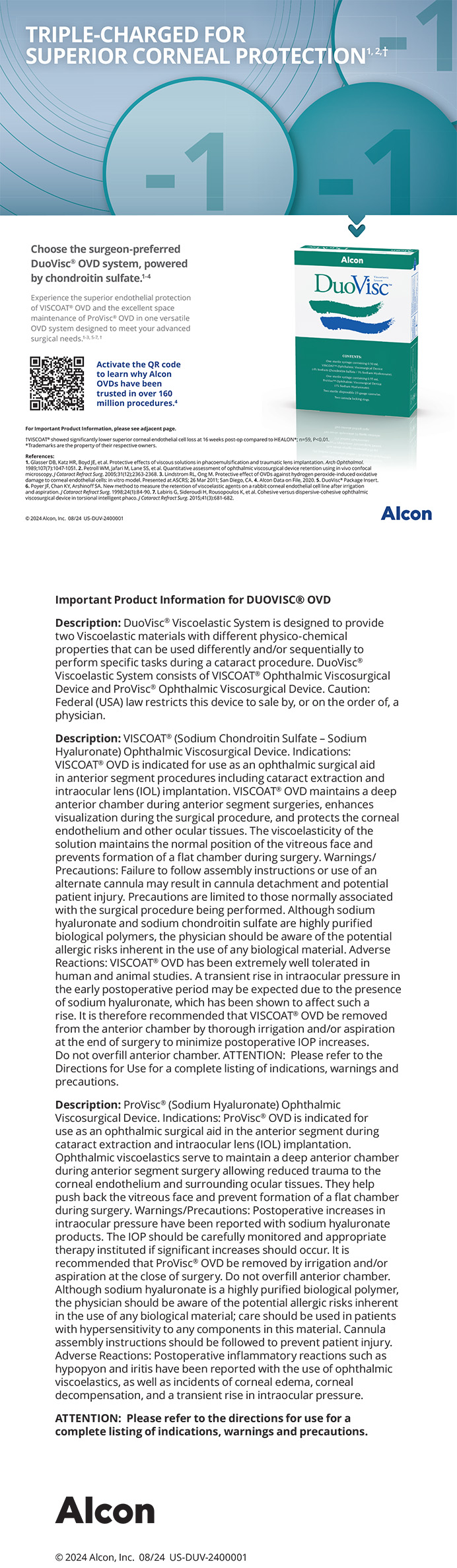
Given the patient’s strong desire for visual independence during physical activity and his increasing intolerance of contact lenses, after a discussion of his options, he decided to proceed with bilateral RLE followed by staged, secondary IOL implantation to address the expected residual hyperopia due to biometry limitations. Preoperative A-scans revealed an axial length of approximately 19.5 mm in both eyes, necessitating the maximum dioptric power (+34.00 D) for the primary lens in each eye (Figure 1).
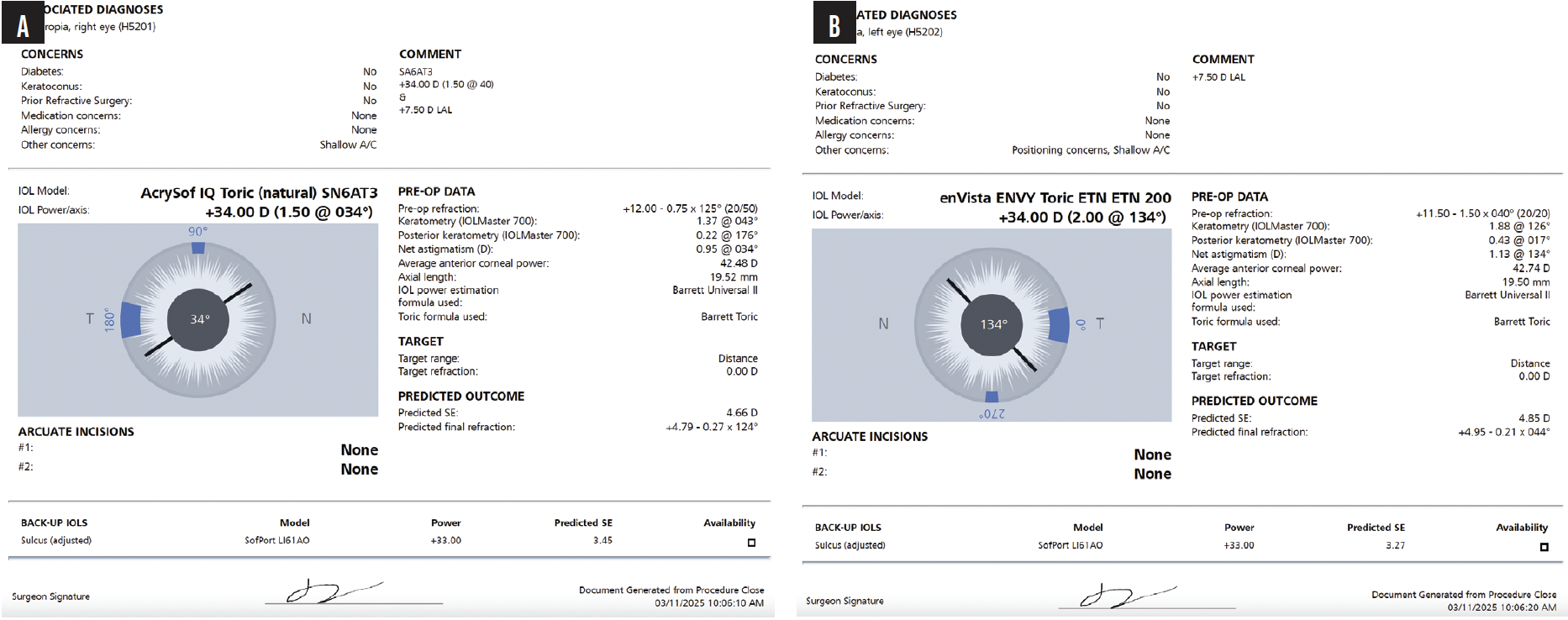
Figure 1. IOL calculations using the Veracity Surgery Planner (Carl Zeiss Meditec) for the primary lens implants in the right (A) and left (B) eyes.
A monofocal toric IOL was selected for the right eye, and a trifocal toric IOL was chosen for the dominant left eye. One day after RLE, the patient’s manifest refraction was +4.79 -0.27 x 124º OD and +4.95 -0.21 x 044º OS. One month after surgery, his UCVA was 20/100-2 OD and 20/50 OS. His BCVA was 20/50 with a manifest refraction of +5.00 -0.75 x 140º OD and 20/25 with a manifest refraction of +4.75 -1.00 x 045º OS.
Two months after RLE, immediately sequential bilateral sulcus fixation of an LAL was performed (Figure 2). IOL calculations used the following formula: manifest refraction spherical equivalent x 1.5 = piggyback IOL power. The result was +7.50 D. Because the LAL is available in 1.00 D increments, a +7.00 D LAL was selected for each eye. The plan was to target mild hyperopia and refine the result with postoperative light adjustments (Figure 3).
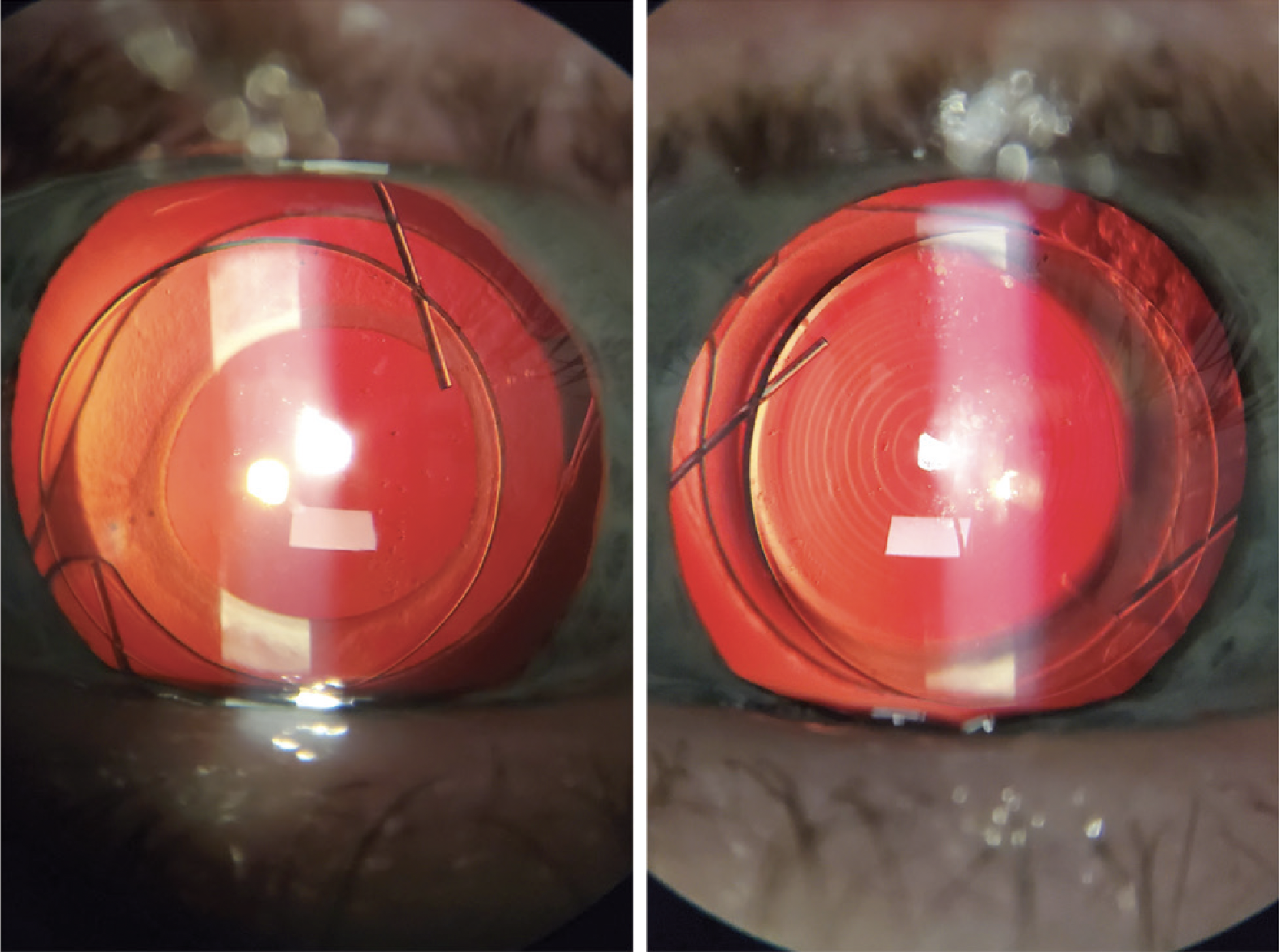
Figure 2. Slit-lamp photographs of the piggyback IOL in each eye.
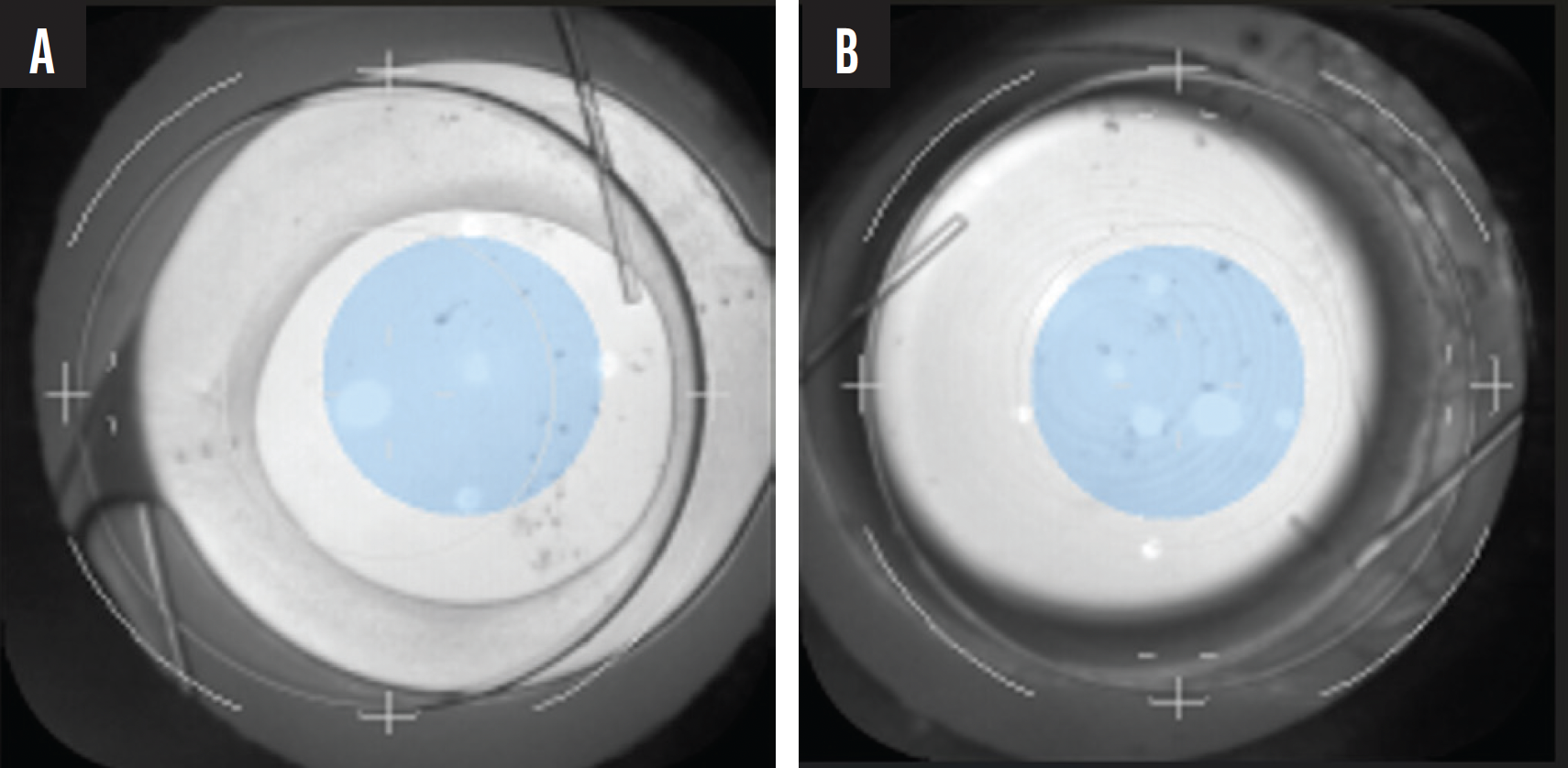
Figure 3. The right (A) and left (B) eyes during light adjustment.
One week after the first light adjustment (4 weeks after LAL implantation), the patient’s uncorrected distance visual acuity (UDVA) was 20/60 OD and 20/30 OS. His uncorrected near visual acuity (UNVA) was J5 OD and J2 OS. His BCVA was +1.00 -1.00 x 145º = 20/50 OD and +0.75 -0.75 x 030º = 20/25 OS. At the lock-in visit (8 weeks after LAL implantation), the patient’s UDVA was 20/60 OD and 20/25+2 OS. His UNVA was J5 OD and J2 OS. His BCVA was +0.50 -0.50 x 165º = 20/50-1 OD and +0.25 -0.25 x 035º = 20/20-2 OS.
The final outcome balanced the patient’s optical limitations with his functional demands and highlights collaboration between the patient and surgeon. Although the initial refractive correction was constrained by available IOL power, postoperative fine-tuning ultimately achieved functional spectacle-free UDVA and UNVA for the patient. He is satisfied with his vision during athletic activities and daily tasks, and he is being monitored for posterior capsular opacification and potential intralenticular opacities.
1. de Wit DW, Diaz JM, Moore TC, Moore JE. Refractive lens exchange for a multifocal intraocular lens with a surface-embedded near section in mild to moderate anisometropic amblyopic patients. J Cataract Refract Surg. 2012;38(10):1796-1801.
2. Petermeier K, Gekeler F, Spitzer MS, Szurman P. Implantation of the multifocal ReSTOR apodised diffractive intraocular lens in adult anisometropic patients with mild to moderate amblyopia. Br J Ophthalmol. 2009;93(10):1296-1301.