CASE PRESENTATION
A 23-year-old woman presents for a cataract evaluation. The patient has been diagnosed with a seizure disorder and an intellectual disability/auditory processing disorder. Her current drug regimen consists of carbamazepine for the management of her seizure disorder.
The patient is able to communicate using a computer and smartphone. She reports an overall decrease in her visual acuity and problems with her nighttime vision, including glare, large halos, and blinding photophobia.
Upon presentation, her UCVA is 20/150 OD and 20/150 OS. Her BCVA is 20/100 OD and 20/100 OS. Glare testing reduces her visual acuity to less than 20/800 OU.
An examination finds a 4+ posterior subcapsular cataract in each eye and no nystagmus (Figure). Findings are otherwise normal.
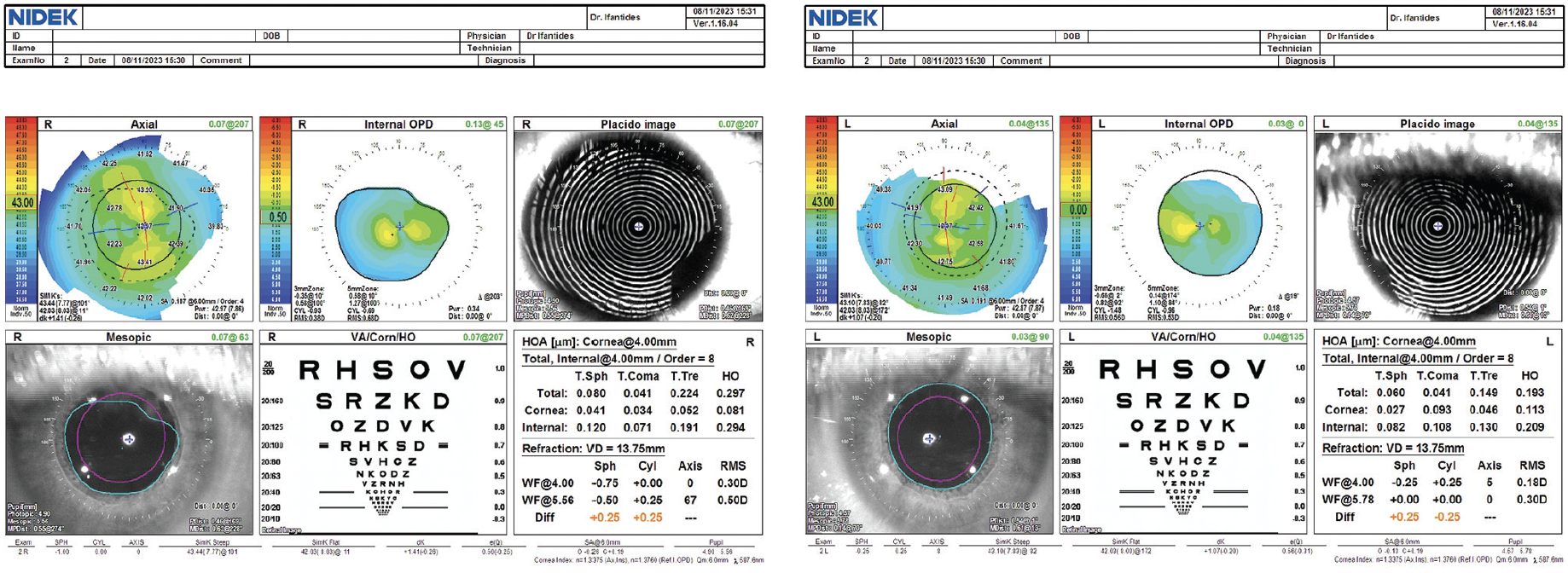
Figure. Preoperative topography.
How would you proceed? Which lens options would you consider given the patient’s age, seizure disorder, and medical history?
— Case prepared by Cristos Ifantides, MD, MBA


BHARAT GURNANI, MBBS, DNB, FCRS, FICO, FAICO CORNEA, FAICO REFRACTIVE SURGERY, MRCS(ED), MNAMS, FACS, FIACLE, AND KIRANDEEP KAUR, MBBS, DNB, FPOS, FICO, FAICO PEDIATRIC OPHTHALMOLOGY, MRCS(ED), MNAMS, FACS
The posterior subcapsular cataracts are profoundly reducing the patient’s functional vision, particularly under glare conditions. Given her age, seizure disorder, and cognitive challenges, surgical planning would seek to balance refractive predictability, safety, and long-term durability. Her carbamazepine therapy and seizure history warrant prioritizing ocular and perioperative stability.
The risk of ocular trauma and forceful eyelid squeezing increases during a seizure, so a monofocal IOL would be the most reliable and safest option. A multifocal or extended depth of focus (EDOF) IOL might exacerbate dysphotopsias such as halos and glare—symptoms the patient is already experiencing—and could compromise her contrast sensitivity. Additionally, neurocognitive processing difficulties would make her neural adaptation to premium optics less predictable.1
In our experience, a bilateral refractive target of low myopia (-0.50 to 0.75 D) is often well tolerated by patients her age and provides them with good uncorrected distance visual acuity while maintaining their near visual function. Provided that she demonstrates good fixation and cooperation, her astigmatism is regular, and topography is repeatable, a toric IOL could be considered, but its rotational stability could be compromised during a seizure.
Surgical intervention is warranted in this situation because posterior subcapsular cataracts often progress rapidly in young patients. Careful coordination with an anesthesiologist would be essential to minimize triggers and ensure adequate seizure control perioperatively. Phacoemulsification with a hydrophobic monofocal IOL, strong caregiver involvement, and clear postoperative instructions would offer the safest, most predictable visual rehabilitation.2


MAHSAW MANSOOR, MD, AND SAMUEL MASKET, MD
The visually significant bilateral posterior subcapsular cataracts are causing profound glare disability and functional vision loss. Given the patient’s age and neurologic comorbidities, careful preoperative planning would be essential. First, reliable measurements of her visual acuity, best refraction, and visual potential would be confirmed. No ocular comorbidities are listed in the case presentation, so for the purposes of this article, we will assume there are none. Fortunately, corneal topography confirms a regular pattern and low amount of internal higher-order aberrations; higher-than-usual posterior against-the-rule cylinder balances the anterior corneal with-the-rule astigmatism.
Because of the patient’s age, IOL selection would address the induction of instant presbyopia. If preoperative testing or counseling suggests that a trifocal IOL is contraindicated owing to concerns about neural adaptation, visual processing limitations, the use of carbamazepine with atropine-like effects on the pupil, or her likely intolerance of dysphotopsias, an enhanced monofocal lens with a monovision strategy or an EDOF IOL such as the Clareon Vivity (Alcon) would be chosen instead.
Given the patient’s seizure disorder and auditory processing disorder, immediately sequential bilateral cataract surgery performed under general anesthesia would be our preference to minimize perioperative stress, reduce repeated anesthetic exposure, and improve compliance. Considering her age and potential for late zonulopathy, a capsular tension ring would be placed prophylactically. If her ability to cooperate with future Nd:YAG laser capsulotomies in a clinical setting is a concern, we would consider performing a primary posterior capsulotomy (with posterior optic capture).
Overall, the surgical approach should balance long-term stability, the patient’s visual rehabilitation, and her neurologic and cognitive considerations while prioritizing her safety and quality of life.

THOMAS A. OETTING, MS, MD
The current situation requires the surgeon to slow down and think about why the patient has cataracts, what alterations to standard surgery might be required, and how her recovery can be optimized.
Consideration No. 1: Why Does the Patient Have Cataracts?
The patient’s lack of nystagmus to some extent suggests that her dense cataracts are more likely acquired and not congenital. Carbamazepine therapy is associated with acquired bilateral cataract formation, including posterior subcapsular cataract. Eye rubbing and other trauma are considerations in a young patient, but in that scenario, more asymmetry in the cataracts might be expected. The patient’s cataracts, seizure disorder, and intellectual disability could also be part of a metabolic disorder such as hypoparathyroidism, and that possibility would be addressed before general anesthesia.3
Most likely, however, the cataracts are related to carbamazepine treatment.
Consideration No. 2: How Should Surgery Be Performed?
I am assuming that the patient would not be able to undergo surgery with topical anesthesia and that the examination was difficult. I would therefore combine an examination under general anesthesia (EUA) with her surgery. The EUA would include keratometry (if not performed in the clinic) and A- and B-scan ultrasonography. Data from the EUA would immediately be entered into an online formula such as the Kane formula to estimate her IOL power (www.iolformula.com).
The patient’s informed consent would be obtained for immediately sequential bilateral cataract surgery but would leave open the option of unilateral surgery if unexpected pathology is noted in one eye during the EUA. If she has a history of eye rubbing, I might consider delayed sequential bilateral cataract surgery, but I would prefer to operate on both eyes with one general anesthesia.
I would be prepared for weak zonules and have the following available: a capsular tension ring, a three-piece IOL for traditional or bicapsular optic capture, a capsular tension segment, and trypan blue dye. The need for postoperative drops would be avoided through the use of intracameral moxifloxacin and subconjunctival dilute triamcinolone.4
I would assume that the patient could not sit for an Nd:YAG laser capsulotomy and therefore perform a primary posterior capsulotomy with bicapsular capture of the three-piece IOL in both eyes to prevent posterior capsular opacification.5 The wound would be secured with a 10-0 polyglactin suture, which would later dissolve, obviating the need for postoperative removal.
Consideration No. 3: Which IOL Would Be Optimal?
I would choose a monofocal IOL and a refractive target of -1.00 D in each eye to optimize the patient’s intermediate visual function while still allowing her decent distance visual acuity. She would likely find self-care and feeding herself easier with a focal point at 1 m rather than at distance. Multifocal IOLs would be avoided because she may have retinal issues and because potential eye rubbing could compromise the cornea in the long term.
Although this is a challenging case and will require a lot of time in the OR and clinic, I am confident that the patient could benefit from cataract surgery. Caring for patients like her gives me the greatest satisfaction.

ZEBA A. SYED, MD
Despite the patient’s young age, her reduced BCVA and dramatic reduction in visual acuity with glare testing indicate that cataract surgery would likely result in meaningful functional improvement, particularly at night. Preoperative counseling would involve both the patient and her caregivers, and the language used would be tailored to the patient’s intellectual disability.
Close coordination with her neurologist and the anesthesia team would be essential to ensure optimal perioperative seizure control. Sedative choices should be considered carefully because some agents might lower the patient’s seizure threshold or interact with her antiepileptic drug. Although topical anesthesia with minimal sedation is often preferred for cataract surgery, her ability to cooperate must be realistically assessed. If cooperation is limited, general anesthesia might be required, although the heightened anesthetic risk must be taken into account.
Intraoperatively, additional precautions might be warranted given the risk of a postoperative wound leak in the presence of limited cooperation or eye rubbing. These steps would include careful wound construction and possible closure of the main incision with a dissolvable suture, which would enhance wound stability and not require removal at the slit lamp postoperatively.
Given the patient’s intellectual disability, multifocal and EDOF IOLs would be avoided. Corneal topography demonstrates greater than 1.00 D of astigmatism in both eyes, making a toric monofocal IOL an option to improve her UCVA while preserving her contrast sensitivity.
Overall, the surgical approach should prioritize visual quality and long-term neurologic tolerance rather than spectacle independence.

WHAT I DID: CRISTOS IFANTIDES, MD, MBA
Because the patient was able to communicate, we spent time discussing her favorite activities, which included a mix of outdoor activities and using a computer and smartphone. Given her young age and the absolute presbyopia that cataract surgery would induce, I discussed a multifocal lens with the patient and her guardian. The conversation thoroughly addressed the technology’s pros and cons, including the potential for residual nighttime halos; neural adaptation; and the possibility that she would be unable to tolerate the IOL. Because the patient was young and active and because she could communicate in basic terminology whether she liked something, her guardian and I decided to proceed with implanting a full range of focus lens to maximize the patient’s spectacle independence with the understanding that a lens exchange might become necessary in the future.
Delayed sequential bilateral cataract surgery with a Clareon PanOptix lens (Alcon) was performed. Rather than general anesthesia, a combination of midazolam and ketamine was administered before the patient was exposed to bright lights and possible overstimulation. She remained calm during surgery with the Ally Adaptive Cataract Treatment System (Lensar) to help align astigmatism correction with the IOL. Microscope illumination was decreased to below 50% to prevent triggering a light-induced seizure. I also verbally walked the patient through each step of surgery to avoid startling her.
Postoperatively, she experienced rapid neural adaptation, and she was happy to be able to see at near, intermediate, and distance. When mild posterior capsular opacification developed in each eye 1.5 years postoperatively, it was treated successfully with an Nd:YAG laser capsulotomy.
1. de Silva SR, Evans JR, Kirthi V, Ziaei M, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2016;12(12):CD003169.
2. Wang D, Ma Y, Hu T, Wang Y, Cai K. Evaluation of visual and optical quality following phacoemulsification cataract surgery with diffractive multifocal intraocular lens implantation: an observational study. Medicine (Baltimore). 2024;103(29):e38905.
3. Marcucci G, Cianferotti L, Brandi ML. Clinical presentation and management of hypoparathyroidism. Best Pract Res Clin Endocrinol Metab. 2018;32(6):927-939.
4. Shorstein NH, McCabe SE, Alavi M, Kwan ML, Chandra NS. Triamcinolone acetonide subconjunctival injection as stand-alone inflammation prophylaxis after phacoemulsification cataract surgery. Ophthalmology. 2024;131(10):1145-1156.
5. Oetting TA. Hyaloid-sparing double capture. Cataract & Refractive Surgery Today. January 2019. Accessed January 7, 2026. https://crstoday.com/articles/2019-jan/hyaloid-sparing-double-capture