In a recent webinar, Cynthia Matossian, MD, FACS, and Jai G. Parekh, MD, MBA, FAAO, discussed the importance of improving the integrity of the ocular surface as the first step toward achieving good outcomes for ophthalmic surgical patients. Here, they describe the challenges of accurately diagnosing and treating dry eye disease (DED) and share illustrative case studies.
Intervention Can Break the Cycle of DED
DED is more than just a nuisance; it is known to negatively impact patients’ daily activities. “We used to think DED was a minor issue,” Dr. Matossian said. “Many of our colleagues wanted to refer these patients out, because we did not have the tools for proper diagnosis or effective treatments. Now, we understand that suffering from DED impacts the quality of one’s life, and we have data associating the disease with depression and anxiety.1 DED truly has a huge ripple effect,” she added.
The symptoms of DED can range from fluctuations in vision to minor ocular pain and irritation that lead to varying degrees of visual impairment.1 Without treatment, the excessive tear evaporation and ocular surface instability caused by DED can create a cycle of desiccation stress and inflammation that may lead to permanent tissue damage.2 With early diagnosis and intervention, it is possible to break the cycle.
Fortunately, clinicians can easily check for DED by performing ocular surface staining and a slit-lamp examination. They can also use objective tests, such as tear osmolarity testing, MMP-9 testing, and meibography, to diagnose and monitor DED. Objective tests are helpful in motivating patients to comply with their treatment plans by providing visual confirmation that the treatment is making a difference.
Dr. Parekh: Case Study #1
Dr. Parekh described the case of a 72-year-old male who presented for cataract surgery evaluation (editor’s note: this was not Dr. Parekh’s patient). He had a history of impaired vision in both eyes, which had gradually decreased over the last 4 years. His chief complaint was significant visual impairment that could not be corrected. He had no other notable health history other than wearing spectacles. He was no longer able to drive at night and had a very high sensitivity to glare. This patient was beginning to have difficulty reading, and he noted that his vision “seems hazy.” His visual acuity was 20/80 in the right eye and 20/40 in the left eye (Figure 1).
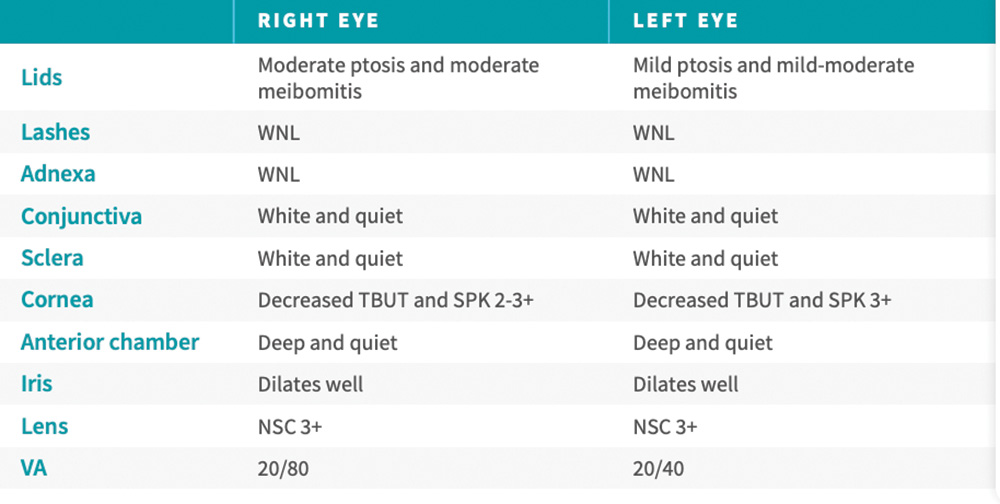
Figure 1. The examination results of a 72-year-old male who presented for cataract surgery evaluation.
Dr. Parekh stressed that, for ophthalmologists to achieve the best surgical outcomes possible, they first must determine the root cause of visual impairments and fluctuating vision. The patient in this case had an OSDI score of 24, which is abnormal, but not extreme. Next, the patient received fluorescein staining and a slit-lamp examination. “In this case, we see a pattern of staining indicating corneal epithelial damage which is causing vision fluctuation” (Figure 2). “If I take that cataract out,” Dr. Parekh explained, “he will still have fluctuating vision. It is incumbent upon me to delay surgery and restore the ocular surface to mitigate the existing damage on the cornea.”
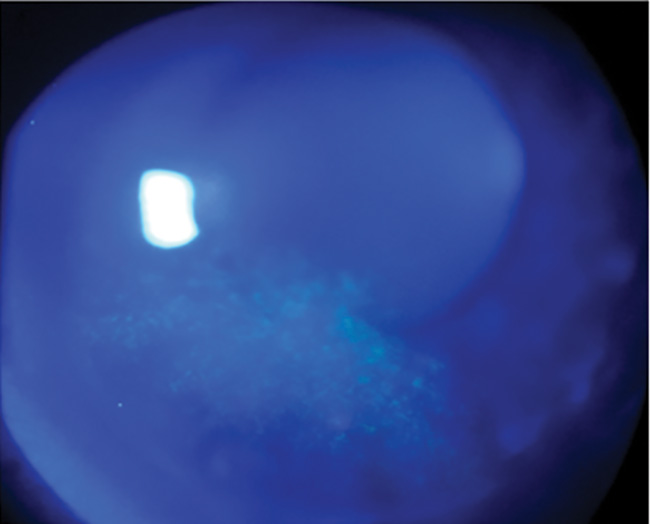
Figure 2. Inferior corneal fluorescein staining indicative of DED.
Image courtesy of Christopher E. Starr, MD.
This patient received treatment with meibomian gland probing, warm compresses, and OTC drops.3-5 Following repeated biometry, he proceeded to cataract surgery.
Dr. Matossian: Case Study #2
Dr. Matossian described the case of a 42-year-old female who presented for a routine eye exam (editor’s note: this was not Dr. Matossian’s patient). She was a parent and worked as a buyer for a large retailer. Her chief complaints included increasing difficulty with near vision and symptoms of eye fatigue, especially late in the day. She had no significant ocular history other than spectacle wear. Visual symptoms and eye fatigue affected her ability to perform at work and enjoy her hobbies. Figure 3 shows this patient’s examination results. Inferior fluorescein corneal staining (Figure 4) indicated DED.
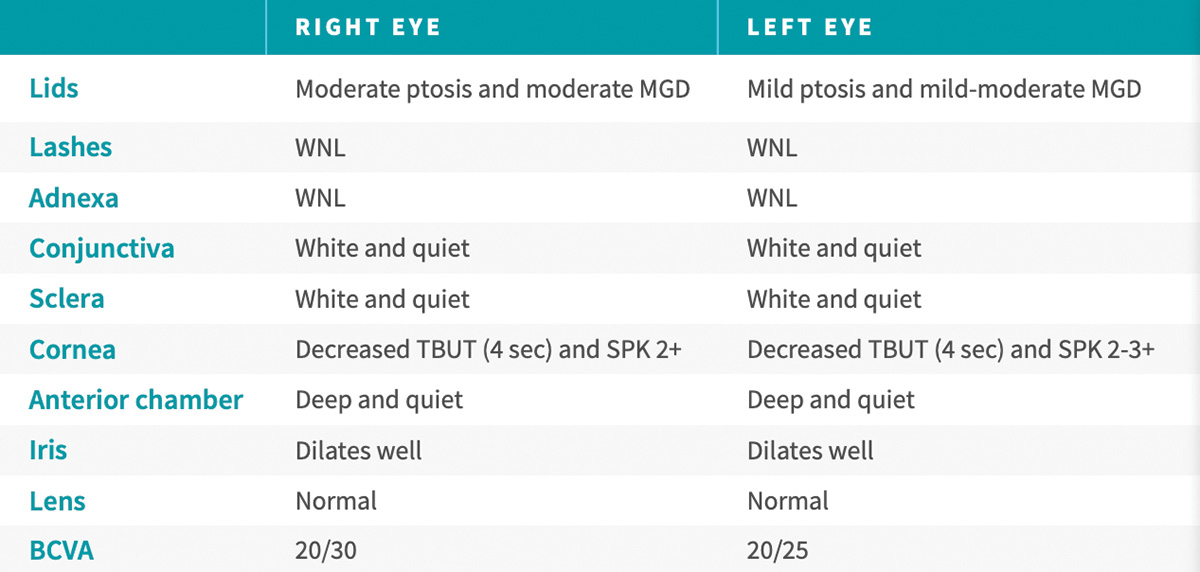
Figure 3. Examination results of a 42-year-old female who presented for a routine check-up.
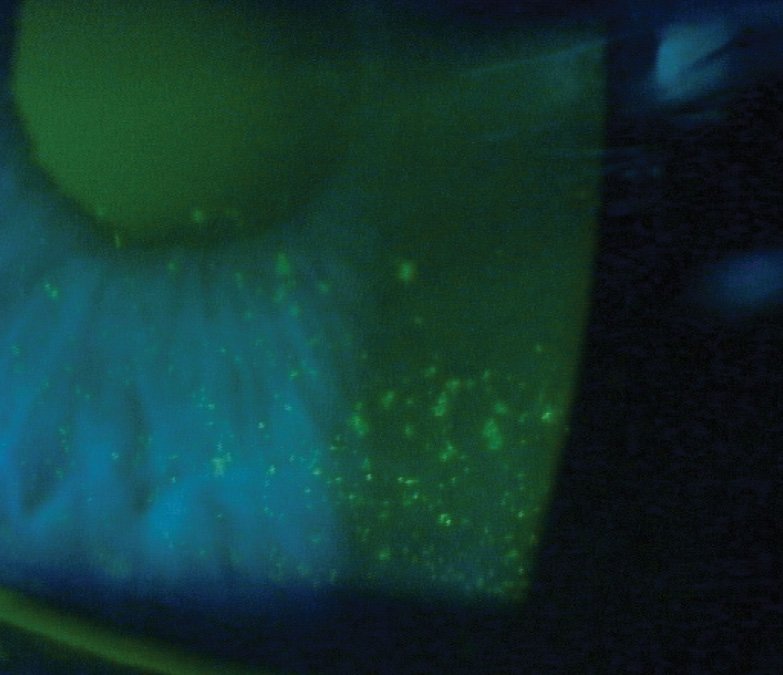
Figure 4. Inferior corneal fluorescein staining indicated DED.
Image courtesy of Paul Karpecki, OD.
Dr. Matossian noted that, because there is often a disconnect between patients’ symptomology and what clinicians see on the slit lamp examination, listening to their complaints is very important. In addition to staining, she said, ophthalmologists should evaluate eyes for meibomian gland dysfunction. She described her approach: “With a cotton tip applicator or your finger, hold the lid down, lift the lid up, and push on it. Check that the orifices are open and that quality meibum is coming out.” Meibomian gland imaging is another tool that Dr. Matossian uses to obtain objective information. The meiboscore number increases when the meibomian glands show changes in their architecture or even degeneration. From black and white images, she can determine a meiboscore from zero to 3, which enables patients to easily see and understand the level of their disease. This patient had a meiboscore score of 2, depicted in Figure 5.
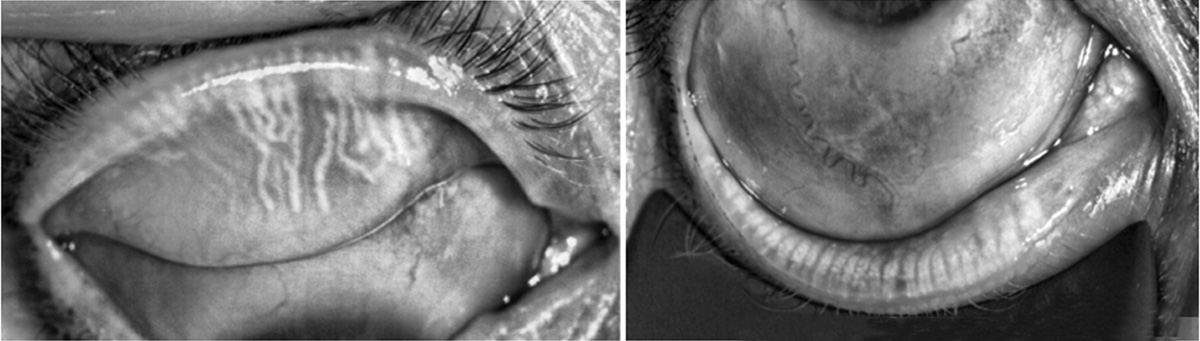
Figure 5. Meibomian gland imaging shows a meiboscore score of 2.
Images courtesy of Sheri Rowen, MD.
This patient was treated with intense pulse light (IPL) therapy, warm compresses, and over-the-counter artificial tears. At a subsequent follow-up visit, the patient’s visual quality had improved, and her ocular staining looked significantly better.
Patients Are Invested in Good
Visual Outcomes
“A healthy ocular surface is important to getting good surgical outcomes,” explained Dr. Parekh. Prior to scheduling ocular surgery, he recommends that practitioners perform a DED consultation, because many patients will have an abnormal corneal surface and concurrent DED.6 “Sometimes, we worry that delaying surgery to tune up the ocular surface and treat the tear film may cause the patient to leave us and find another provider,” he acknowledged. “However, my experience is that patients are very compliant with the regimen I prescribe. They have a vested interest in getting the best outcome for their eyes and their vision.”
1. Dana R, Meunier J, Markowitz JT, Joseph C, Siffel C. Patient-reported burden of dry eye disease in the United States: results of an online cross-sectional survey. Am J Ophthalmol. 2020;216:7-17. doi: 10.1016/j.ajo.2020.03.044.
2 Pflugfelder SC, de Paiva CS. The pathophysiology of dry eye disease: What we know and future directions for research. Ophthalmology. 2017;124(11S):S4-S13. doi: 10.1016/j.ophtha.2017.07.010.
3. Lam PY, Shih KC,Fong PY, et al. A review on evidence-based treatments for meibomian gland dysfunction. Eye Contact Lens. 2020;46:3-16.
4. Pucker AD, Ng SM, Nichols JJ. Over the counter (OTC) artificial tear drops for dry eye syndrome. Cochrane Database Syst Rev. 2016;2(2):CD009729.
5. Fermon S, Zaga IH, Melloni DA. Intraductal meibomian gland probing for the treatment of blepharitis. Arch Soc Esp Oftalmol. 2015;90:76-80.
6. Trattler, WB, Luch J. What cataract surgeons don’t know can hurt premium IOL outcomes. Ophthalmol. Times. November 13, 2013. https://www.ophthalmologytimes.com/view/what-cataract-surgeons-dont-know-can-hurt-premium-iol-outcomes. Accessed April 30, 2023.
©2023 Bausch + Lomb NOV03.0021.USA.23


