When we see patients before cataract or refractive surgery, we optimize the ocular surface beforehand, so we can take accurate preoperative measurements. We follow a systematic approach to managing the ocular surface disease, but one problem we see again and again is Demodex blepharitis, and it has been the 800-pound gorilla in the room. We have not had robust treatment options for these mites, so we have instead focused on controlling their effects on the lids and ocular surface before proceeding with surgery.
The absence of proven, effective therapies has been a particular concern because a significant number of patients have Demodex infestation, including about 45% of patients with blepharitis,1 84% of patients 60 and older, and 100% of patients who are over 70.2 Patients with rosacea have nine times the average rate of infestation.3
Now, as we’re watching exciting therapeutic developments for Demodex blepharitis move through the pipeline, it’s important to raise our understanding of the prevalence of this condition and learn how we can easily identify it by checking for collarettes on the upper lid margin. Practitioners should also be aware of a recent prevalence study, which they are encouraged to try in their own practices.
Key to Demodex Blepharitis: Collarettes
Collarettes are a pathognomonic sign of Demodex blepharitis. In a study of eyelashes with and without collarettes, 100% of the lashes with collarettes had Demodex mites, while only 7% of the lashes without collarettes had Demodex mites.4
We see collarettes all the time: clear to whitish waxy cuffs at the base of the eyelashes, particularly on the upper lid. Also called cylindrical dandruff, collarettes are the accumulated waste products of D. folliculorum, a common parasitic mite that lives in the eyelash follicles. While the presence of Demodex is normal, the appearance of collarettes indicates an abnormally high population.
Collarettes are formed through the mite’s natural life cycle. Demodex mites burrowed in the eyelash follicles release proteases and lipases for external digestion of the eyelid’s healthy epithelial cells and sebum. Collarettes form at the base of the eyelashes through the accumulation of waste products from this process, including digestive proteases and lipases, undigested cellular material, lipids, keratin, follicular dandruff, Demodex eggs, and dead Demodex mites. The mite’s 14-18-day life cycle5 repeats as new eggs hatch, and the population continues to proliferate.
This infestation causes Demodex blepharitis, which is characterized by inflammation of the eyelid margin, itching, redness, blurring of vision, ocular irritation, and lash abnormalities. Patients are often treated for ocular surface inflammation and given traditional treatments for blepharitis without addressing the Demodex infestation, so the problem and its symptoms continue.
Simple, Routine Screening
Because collarettes are the product of Demodex infestation, diagnosing Demodex blepharitis is as simple as identifying the presence of collarettes. They are easily seen with a standard eye examination of the upper lid margin with the patient’s eyes closed. It’s important to have the patient look down or close their eyes because you may miss the collarettes when looking straight at the patient’s open eye. There is no need to epilate a lash and examine it under the microscope to confirm the diagnosis–a standard eye exam is just as effective, takes less time, and doesn’t hurt the patient (Figure 1).7,8
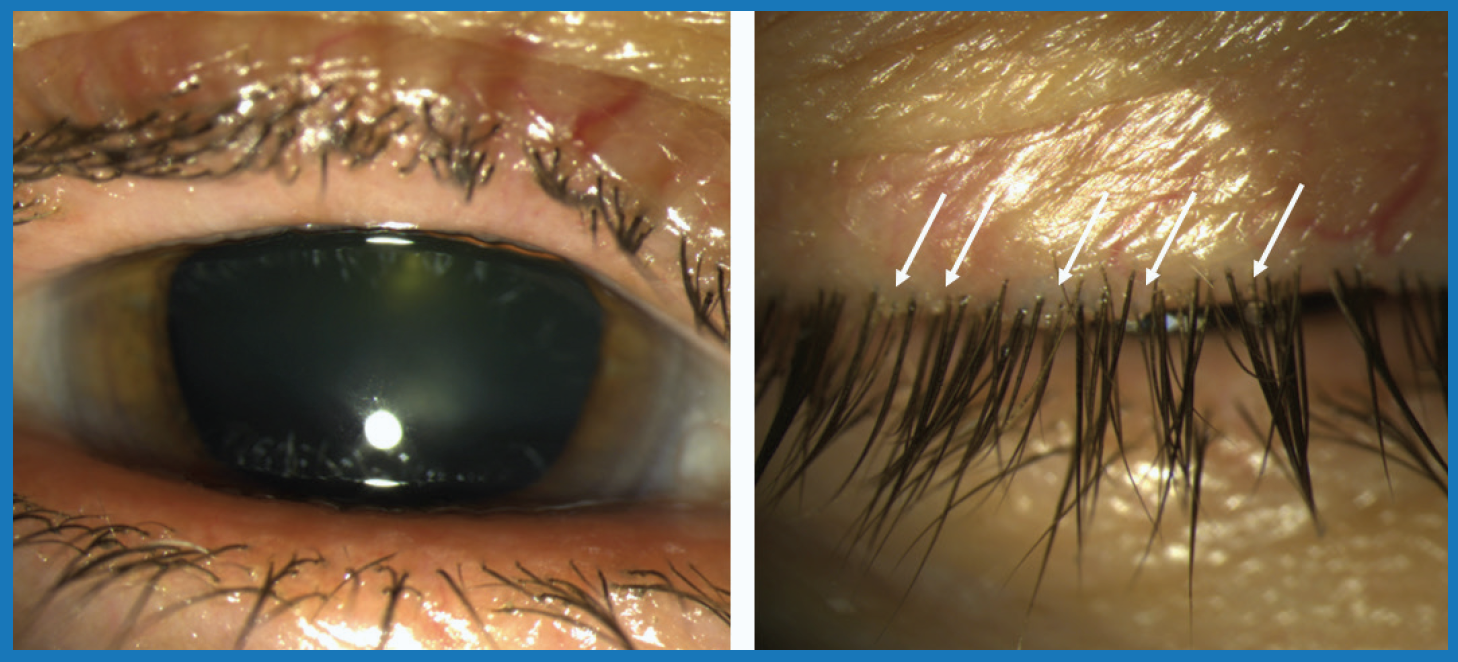
Figure 1. Collarettes are difficult to see on the open eye (left) but are clearly visible on the closed eye (right).
Photo: Elizabeth Yeu, MD
Screening for collarettes should be a simple part of every routine eye exam. Some patients might not be complaining of symptoms yet, or they might have symptoms that we misinterpret solely as dry eye disease, so we need to understand what’s really happening. Also keep in mind that although Demodex blepharitis disproportionately affects older patients, it exists in many groups, including younger patients. In addition to collarettes, patients with Demodex blepharitis commonly exhibit lash distension or loss, eyelid thickening, corneal scarring, and eyelid redness. And they often present with ocular surface discomfort, contact lens intolerance, and recurrent styes or chalazia.
Study: High Prevalence, Dry Eye Implications
In a multi-center observational trial in June and July 2020 that included both ophthalmologists and optometrists, practitioners quantified how many patients had collarettes, which is indicative of Demodex blepharitis. Each doctor completed a short questionnaire and standard eye exam for sequential patients presenting for any purpose, for a total of 1,121 patients in eight practices.
On average, about 58% of patients had collarettes (Figure 2).9 This translates to about 25 million patients that may have Demodex blepharitis in the United States. Many practitioners were surprised at how widespread Demodex blepharitis is in their patient population. The study supports routine screening of all patients, especially as treatment options emerge that can help us treat the underlying cause of disease. Another noteworthy finding among the same sequential study sample was that 20% of patients were using Restasis (Allergan) or Xiidra (Novartis), and 13% used one of these medications and had collarettes.
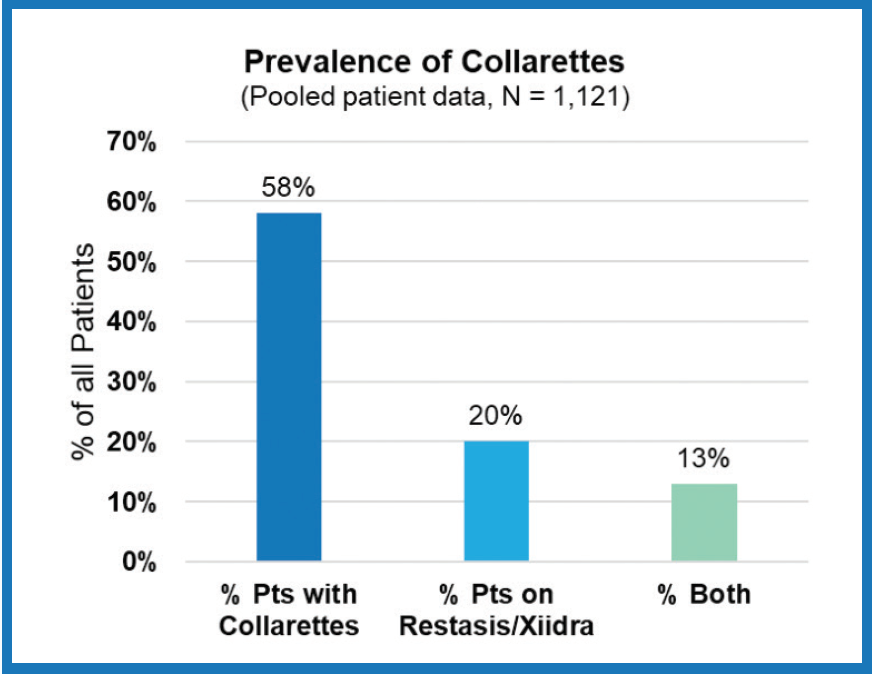
Figure 2. Prevalence of collarettes among all patients coming to ECP offices.
In cases like these, where doctors diagnose and treat ocular surface disease but do not diagnose and treat Demodex blepharitis, we often see that patients don’t meet their goals for dry eye therapy because the Demodex problem is unresolved. Considering that more than half of patients taking a prescription dry eye therapy in these practices had collarettes, it’s likely that the patients and doctors have been growing frustrated that these medications have not been more effective.
Take the Collarette Challenge
How many patients in your practice have Demodex blepharitis? To find out, simply screen every sequential patient for collarettes over the course of 1 week and record the results. It’s an eye-opening first step in a new era where effective treatment for Demodex blepharitis is on the horizon.
1. Zhao YE, Wu LP, Hu L, et al. Association of blepharitis with Demodex: a meta-analysis. Ophthalmic Epidemiol. 2012;19(2):95-102.
2. Post CF, Juhlin E. Demodex Folliculorum and Blepharitis. Arch Dermatol. 1963;88:298-302.
3. Chang YS, Huang YC. Role of Demodex mite infestation in rosacea: A systematic review and meta-analysis. J Am Acad Dermatol. 2017;77(3):441-447.e6.
4. Gao YY, Di Pascuale MA, Li W, et al. High prevalence of Demodex in eyelashes with cylindrical dandruff. Invest Ophthalmol Vis Sci. 2005;46(9):3089-3094.
5. Liu J, Sheha H, Tsenga SCG. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol. 2010;10(5):505-510.
6. McBain AJ, O’Neill CA, Oates A. (2016). Skin Microbiology. Elsevier.
7. Fromstein SR, Harthan JS, Patel J, et al. Demodex blepharitis: clinical perspectives. Clin Optom (Auckl). 2018;10: 57-63.
8. Peles IM, Zahavi A, Chemodanova D, et al. Novel In-Office Technique for Visual Confirmation of Demodex Infestation in Blepharitic Patients. Cornea. 2020;39(7):858-861.
9. Tarsus Collarette Prevalence Study, 2020.


