Dry Eye University (dryeyeuniversity.com) was established with the aim of elevating the business of dry eye disease (DED) in modern eye care practices. With the support of industry partners, program 26 sold out in February 2024 and was attended by ophthalmologists, optometrists, private equity teams, and practice CEOs with their staff. DED is big business.
An estimated 36 million individuals have DED in the United States, although the reported prevalence ranges greatly. As the CEO of a practice that specializes in DED care, I have found that at least eight out of 10 patients who walk through our doors have some signs and/or symptoms of DED. In contrast, my work with practices all over the country through Dry Eye University and industry partner relationships suggests that only 3% to 5% of US practices embrace DED patients.
The goals of care are to halt the progression of this lifelong disease and increase patient comfort. In a business sense, however, patients with chronic conditions such as DED and glaucoma are akin to annuities on a practice’s productivity sheet year after year. This article shares tips on how to optimize a DED business.
FINANCIAL CONSIDERATIONS
Advertising. Thankfully, little cash outlay is necessary to create a profitable dry eye center. Patients with DED walk through the practice’s doors every day. Having patients answer the Standard Patient Evaluation of Eye Dryness (SPEED) questionnaire can quickly identify which of them have DED symptoms. (Diagnosing asymptomatic DED requires a slit-lamp examination.)
The only advertising expenditure I recommend when starting a dry eye clinic is to update the practice’s website to include DED as a service area.
Cash pay versus insurance coverage. Many DED services are cash pay, but examinations, amniotic membrane treatment, diagnostics, and allergy testing are covered by insurance. Due diligence by the practice is required. Staff must verify coverage and utilization in advance because patient deductibles can be high and should be collected up front. I also recommend offering patient financing for DED services.
Bundled treatment packages can reduce patient confusion, shorten discussions, and increase capture rates. Perhaps the recommendation for a given patient is eyelid debridement, topical medication for meibomian gland dysfunction, and intraductal meibomian gland probing. Instead of presenting individual options, a patient counselor can offer these three strategies as a package and discuss a monthly payment figure as opposed to a large total.
In my experience, dry eye revenue can eventually constitute 20% or more of a practice’s revenue.
Acquisitions. Tools are necessary for DED diagnosis, patient education, and treatment (Figure 1). I encourage practices to research available resources, seek references from colleagues, and negotiate the best possible pricing and warranties.
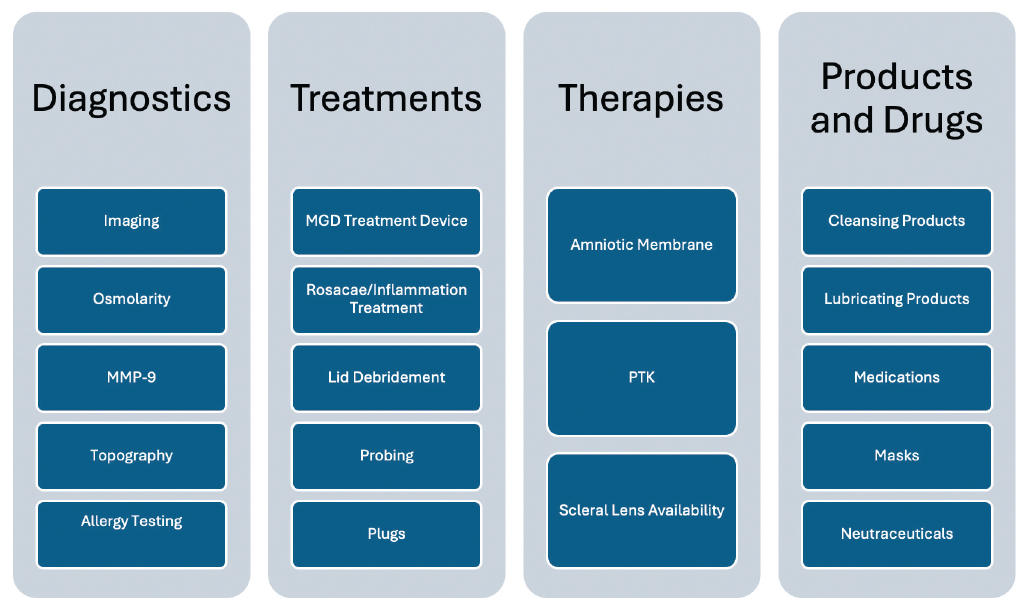
Figure 1. A successful dry eye clinic requires four categories of tools. Abbreviations: CCH, conjunctivochalasis; MGD, meibomian gland dysfunction; MMP-9, matrix metalloproteinase-9; PTK, phototherapeutic keratectomy.
Practices that stock and sell products can make a reasonable profit if they use volume pricing when shopping, set prices based on their overhead, and implement a fail-safe inventory protection process. Another option is to partner online with companies such as Dry Eye Rescue so that patients can make purchases and the practice can make a profit without having to maintain inventory.
FLOW AND PROCESS
Education. All patient-facing staff members should receive training so that they can offer appropriate information and education. Surgical counselors are particularly well positioned to help educate and capture DED patients.
Flow. Figure 2 shows my recommendation for clinic flow. The technician starts the workup and completes the SPEED questionnaire with the patient. Diagnostic imaging, tear osmolarity testing, and matrix metalloproteinase-9 measurements are obtained. Depending on the SPEED score and other results, the technician may hand off the patient to a counselor with a simple statement like the following: “Based on your signs and symptoms of DED, I am going to have the counselor review a few things about this disease process before you meet with the doctor.” The counselor readies the patient for the provider, who then reviews the diagnostics, makes recommendations, and hands the patient back to the counselor for scheduling.
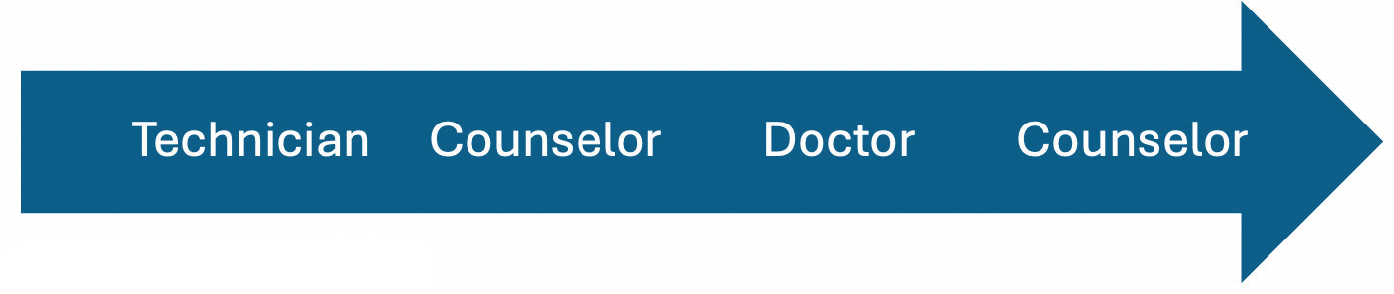
Figure 2. Suggested flow of a dry eye clinic.
Scheduling. Many practices I have encountered want to use block scheduling for DED patients. The volume of patients with DED, however, is generally too high for them to be seen just 1 day per week or by a single provider. DED treatment scheduling should be strategic. Care consists largely of cash-pay procedures that boost the practice’s bottom line, so appointments should not be viewed as disruptions. Many treatments take several minutes to perform, making the addition of same-day procedures easy.
Follow-up visits are required for the evaluation of treatment efficacy. SPEED and osmolarity scores can be instrumental in the assessment of patient comfort and treatment success.
IMPLEMENTATION
I highly recommend appointing a champion to take charge of integrating DED care into the practice. Consistency and staff education drive success. Treating the practice’s providers and staff members with DED creates a pool of passionate team members who can provide impressive testimonies about the services offered. Team collaboration to develop a dry eye standard of care for the practice can help ensure consistency. This standard can be adjusted when new offerings are added.
Industry partners are excellent resources for education and implementation assistance. Their first responsibility is to their own products, so it is important to partner with the manufacturers of all the technologies the practice offers.
CONCLUSION
Patients with DED are special in many ways. Some have been ignored for so long that their disease is negatively affecting their quality of life. Others are asymptomatic. A dry eye clinic can benefit a large segment of the practice’s existing patient base and boost its profitability.