CASE PRESENTATION
A 76-year-old patient presents with diplopia and blurry vision in the right eye. This eye underwent penetrating keratoplasty for advanced keratoconus 20 years ago, cataract surgery with the implantation of a toric IOL 4 years ago, and sutured recentration of the IOL 1 year ago.
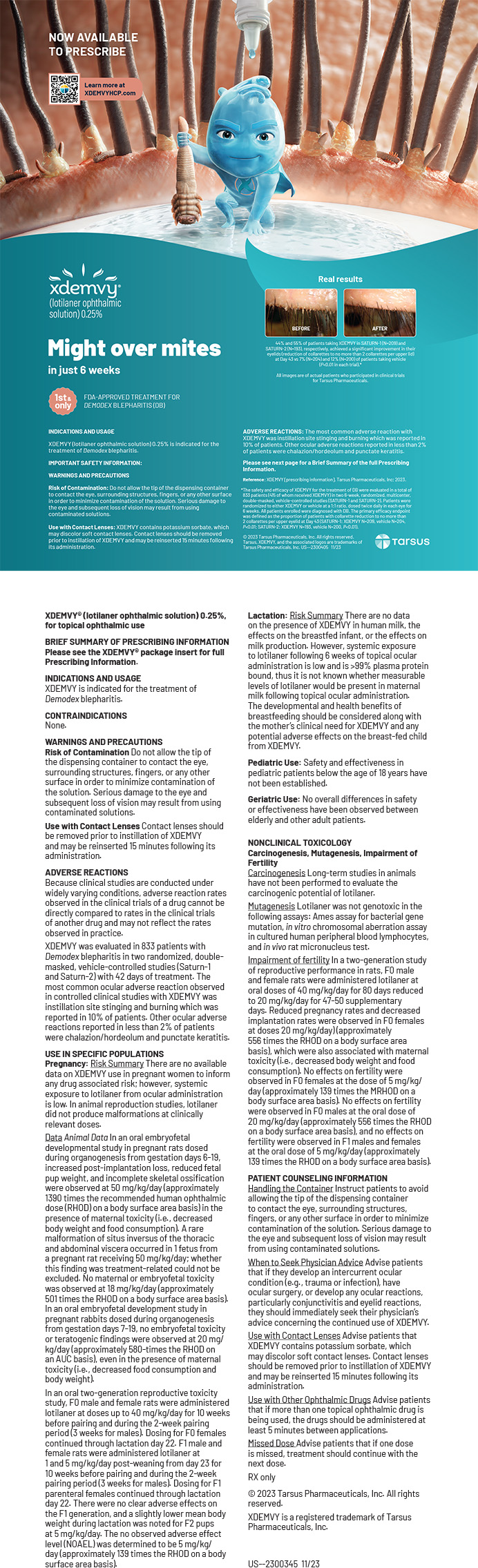
On examination, the patient’s UCVA is 20/200 OD, and their BCVA is -2.50 + 4.00 x 150º = 20/50 OD. The corneal transplant is clear. Superior dislocation of the IOL–capsular bag complex is observed (Figure 1). Residual cortex and anterior tilt of the lens are evident, and iris sutures are present at the 11 and 12 clock positions. Multiple iris transillumination defects are visible. An OCT scan of the macula is normal. Tomography reveals 5.00 D of astigmatism at 140º.
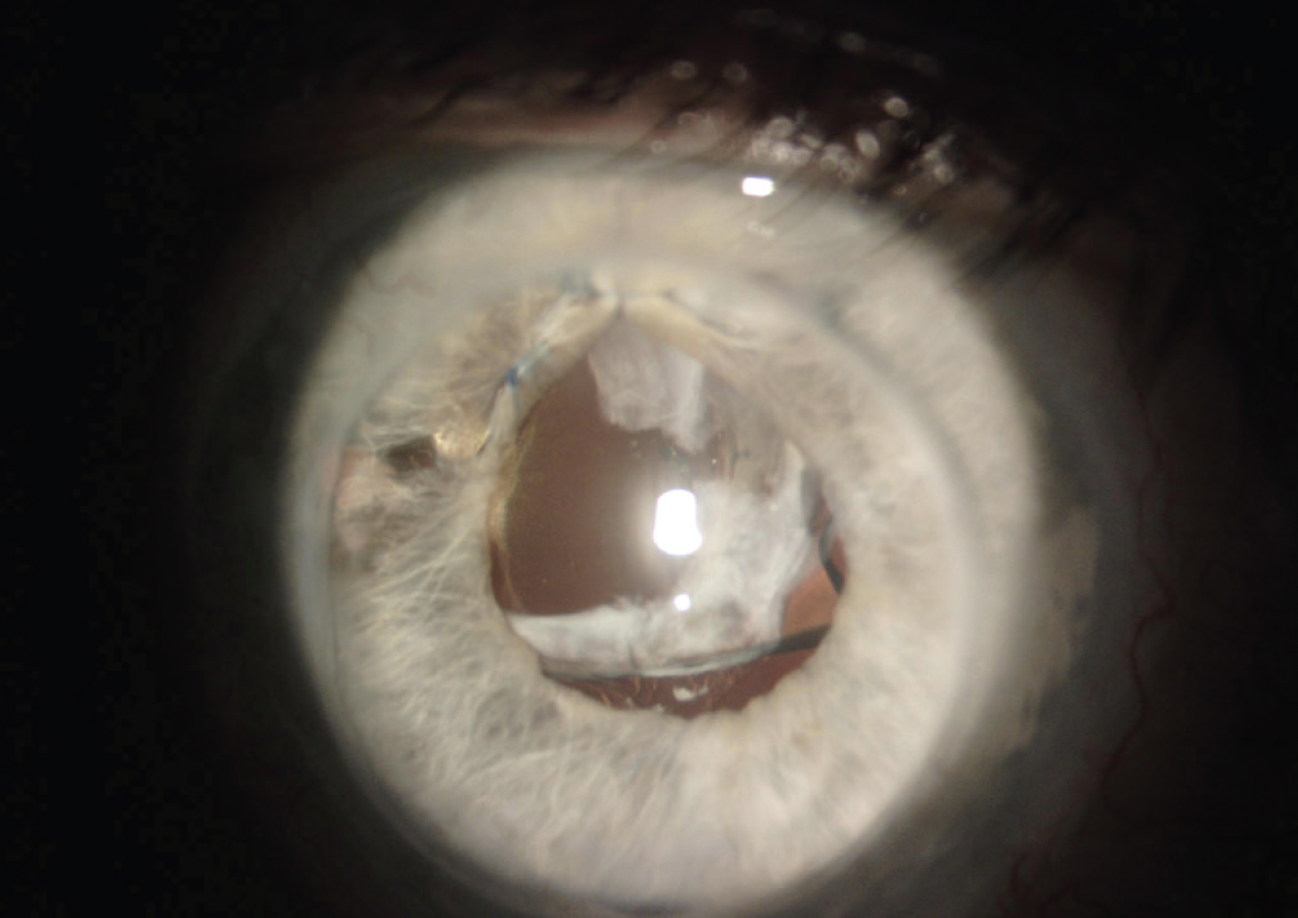
Figure 1. A slit-lamp examination finds a dislocated IOL–capsular bag complex in an eye with a history of penetrating keratoplasty.
The left eye has a significant corneal scar, and the patient’s BCVA is 20/200 OS.
How would you proceed? Would you recenter the IOL–capsular bag complex? Perform an IOL exchange for a scleral-fixated lens? How would the presence of a corneal transplant influence incision placement and surgical planning?
—Case prepared by Audrey R. Talley Rostov, MD

ASHVIN AGARWAL, MS
Scheimpflug tomography with the Pentacam (Oculus Optikgeräte) would be performed to evaluate the corneal astigmatism in the patient’s right eye. Analysis would focus on important indicators such as the root mean square value of higher-order aberrations and the refractive power map, both of which play a crucial role in incision planning. The patient would receive preoperative counseling regarding the management of postsurgical irregular astigmatism, including options such as contact lenses and glasses.
I would plan an IOL exchange using the glued IOL scaffold technique.1 After the initial steps of a conventional glued IOL technique are complete, a three-piece foldable IOL would be gradually introduced. A handshake technique would be used to externalize the trailing haptic. The IOL haptics would then be carefully tucked into the scleral pockets. A vitrectomy would be performed at the sclerotomy sites to eliminate residual cortex and any protruding vitreous. Next, the original toric IOL would be bisected with IOL cutting scissors and extracted. If necessary, a single-pass four-throw pupilloplasty would be performed to reconstruct the pupil. A generous amount of an OVD would be maintained in the eye during surgery to minimize endothelial damage.
I had a similar case in which a 68-year-old man experienced dislocation of a posterior chamber IOL into the anterior chamber and corneal decompensation. An IOL exchange using the glued IOL scaffold technique was performed in combination with a pre-Descemet endothelial keratoplasty and a single-pass four-throw pupilloplasty. Three weeks after surgery, the patient’s BCVA was logMAR 0.3 (Figure 2).
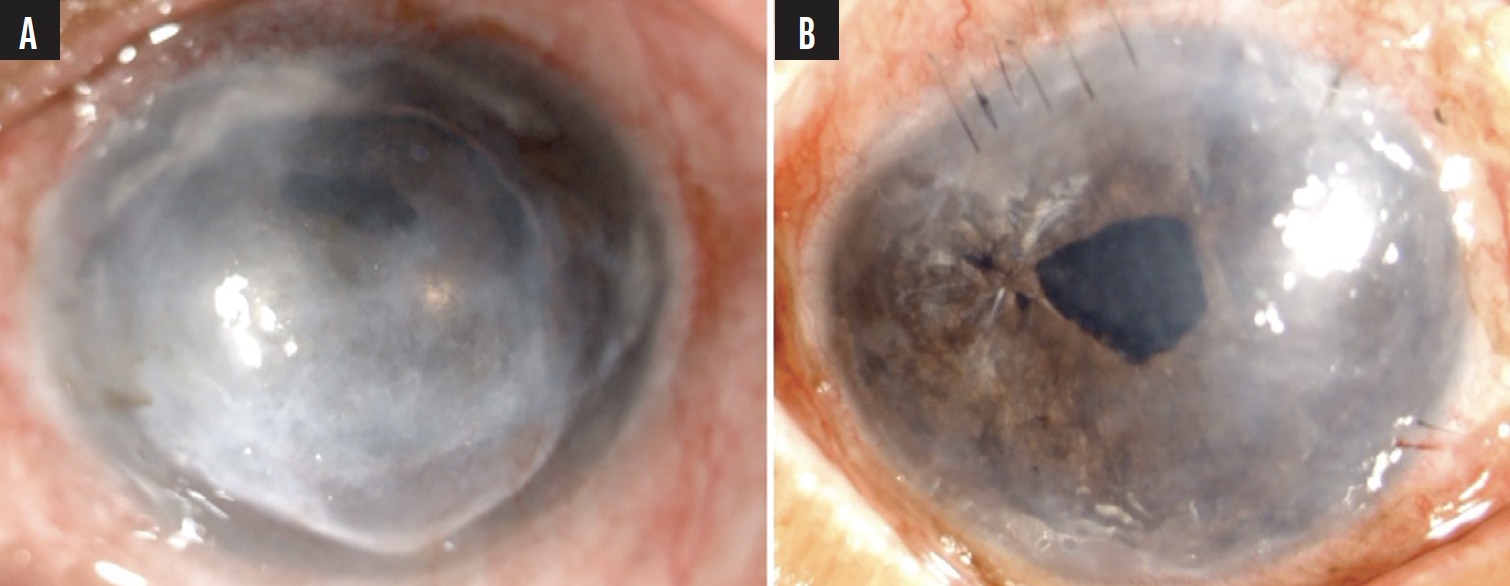
Figure 2. A 68-year-old man presented with posterior chamber IOL dislocation into the anterior chamber and endothelial decompensation (A). The eye is shown 3 weeks after an IOL exchange with the glued scaffold technique in combination with a pre-Descemet endothelial keratoplasty and single-pass four-throw pupilloplasty (B).
(Courtesy of Ashvin Agarwal, MS)

EHUD ASSIA, MD
The cornea of the right eye appears to be clear, so the patient is not currently a candidate for a graft exchange. My usual approach to eyes with malpositioned IOLs is to reposition the lens if it seems to be in good shape and the visual axis is clear. This minimally invasive procedure is performed by passing needles and sutures through tiny scleral holes.
The current case, however, presents additional considerations. The patient’s BCVA is suboptimal in the right eye, yet it is the better-seeing eye. It has undergone surgery at least three times already, and the cornea may not tolerate more than one additional operation. There is evidence of iris damage, a significant amount of residual lens material, and high corneal astigmatism. Furthermore, the IOL is a toric model, so it must be positioned in a precise location.
Although IOL repositioning would be doable, the surgical results may be disappointing, and additional surgery may be required. For these reasons, I would release the IOL (if it is sutured to the iris) and remove both it and the lens capsule. A new toric IOL, preferably one with four closed loops, would then be sutured to the sclera to maintain a precise axis, optimize lens stability, and minimize tilt. The toric power would be calculated with the corneal parameters only (anterior and posterior curvatures plus incision location and size). The current refraction, which is affected by the IOL toricity and tilt, would be ignored. My preferred fixation technique is the adjustable flange technique using 6-0 polypropylene sutures, but other techniques could be used instead.

SAMUEL MASKET, MD
My approach is based on the following four assumptions:
- No. 1: The patient cannot wear a contact lens;
- No. 2: Corneal topography reveals reasonably regular corneal astigmatism;
- No. 3: The existing corneal graft is unlikely to require replacement; and
- No. 4: The iris is incapable of holding an Artisan IOL (Ophtec).
The nasal haptic of the malpositioned IOL is located outside a fibrotic capsular bag remnant, and the capsule has been cut superiorly. Given these conditions, neither the IOL nor the capsule can be salvaged. An IOL exchange is therefore necessary. A toric IOL is the most likely to provide the patient with good vision, but scleral fixation would be required. Fortunately, the enVista hydrophobic acrylic IOL (model MX60, Bausch + Lomb) has positioning holes at the haptic-optic junction, allowing suture fixation, and it is available in a toric model that can provide up to 5.75 D of astigmatic correction at the IOL plane and approximately 4.00 D at the corneal plane. That would be useful here.
A pars plana assisted anterior vitrectomy would be performed. Next, the IOL and capsular bag would be removed through a 3.5-mm temporal limbal incision. The appropriately powered toric IOL would then be sutured on the axis. A cow-hitch technique with PTFE sutures would be used to secure the IOL to the sclera 2.5 to 3.0 mm posterior to the limbus via sclerotomies placed 5.0 mm apart (Figure 3). The sutures would be tied to one side in slipknots, equally tensioned, and cut short, allowing careful burying of the knots in the sclerotomies. Afterward, as tolerated by the iris tissue, pupilloplasty can be attempted in order to reduce pupil size.
Figure 3. With a cow-hitch technique, PTFE sutures are passed through the positioning holes at the haptic-optic junction of an MX60 IOL just before lens implantation.
(Courtesy of Samuel Masket, MD)

WHAT I DID: AUDREY R. TALLEY ROSTOV, MD
Given the violation of the capsular bag, dislocated IOL, and previous attempt to reposition it, I decided to perform an IOL exchange and vitrectomy. A generous amount of a dispersive OVD was injected to protect the corneal endothelium. Scissors and forceps (both from MicroSurgical Technology) were used to section the IOL and remove it through a 3-mm temporal corneal incision located outside the graft-host junction. After a pars plana vitrectomy was performed, a three-piece CT Lucia IOL (Carl Zeiss Meditec) was implanted and secured with intrascleral haptic fixation. The target refraction was -2.00 D. I planned for slight myopia in case the patient requires an endothelial keratoplasty in the future.
Eight weeks after the IOL exchange, corneal relaxing incisions were made in the graft with a femtosecond laser to reduce residual astigmatism. The patient’s final refraction was -2.00 +1.50 x 145º = 20/30+2. They were pleased with the result, and the cornea remained clear.
1. Agarwal A, Kumar DA, Jacob S, et al. Fibrin glue-assisted sutureless posterior chamber intraocular lens implantation in eyes with deficient posterior capsules. J Cataract Refract Surg. 2008;34(9):1433-1438.