Femtosecond lasers for cataract surgery have been in use for more than 5 years. Many surgeons swear by the technology, whereas others are less convinced of the benefits. I have found the laser especially helpful for many complex cataract cases, yet for certain types of cataracts, I avoid its use.
CORNEAL OPACITY
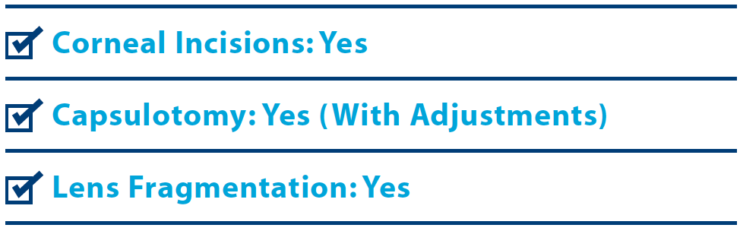
Corneal scarring or opacities can attenuate or block the optical coherence tomography (OCT) imaging necessary for the lens-based cuts. This may lead to skips in the capsulotomy and an incomplete cut. Typically, the OCT shadows are visible during the imaging portion of the laser procedure. Two modifications of the settings can help in this scenario. First, the capsulotomy can be shrunk, enlarged, or moved slightly to avoid a focal opacity. Second, the surgeon can increase the energy setting for the capsulotomy. During phacoemulsification, care must be taken to ensure a complete capsulotomy, and if not achieved, then a manual capsulorhexis can be performed.
I have successfully used the laser in postkeratoplasty eyes and those with Fuchs dystrophy, subepithelial infiltrates, and small pterygium. Eyes with Fuchs dystrophy or other endothelial dysfunction in particular could benefit from the reduction of phaco energy through laser fragmentation.
POSTERIOR POLAR/COMPROMISED POSTERIOR CAPSULE
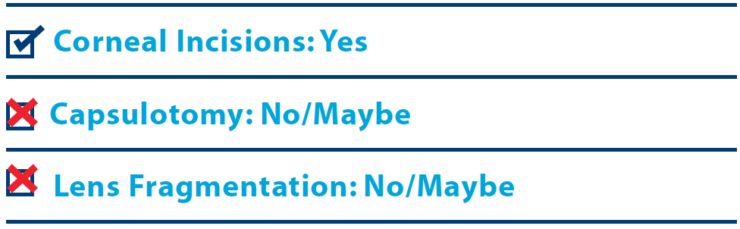
Whatever the surgeon’s technique, the cardinal rule for dealing with posterior polar cataracts is to avoid hydrodissection. The fluid wave may find the potential or actual defect and enter the posterior segment, enlarging the hole. This also applies to rapid-onset cataracts after intravitreal injections. Laser capsulotomy and especially lens fragmentation create plasma bubbles, which can find their way to the capsular defect. In addition, I/A is slightly more “sticky” with laser capsulotomy/fragmentation and may create more difficulties during cortical removal.1 I have heard of other surgeons’ getting into trouble with laser fragmentation for posterior polar cataracts. Even though there are a few case reports of successful limited laser segmentation for posterior polar cataracts,2,3 I prefer a manual approach. I proceed with a manual 5-mm capsulorhexis (to allow a possible optic capture), gentle hydrodelineation, supracapsular emulsification of the endonucleus, and an outside-in approach with I/A of the epinucleus/cortex that leaves the posterior polar area for last (Figure 1).
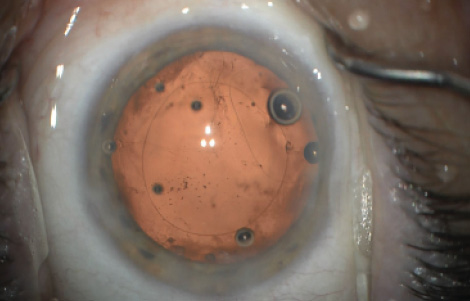
Figure 1. In this postintravitreal injection surgery, Dr. Raviv performed a manual rather than a laser capsulotomy to avoid laser-generated gas bubble enlargement of the preexisting posterior capsular defect seen here.
FORME FRUSTE KERATOCONUS
During the past 2 decades, corneal refractive surgeons have been carefully screening patients for forme fruste keratoconus (FFKC) or frank keratoconus (KC) before LASIK and PRK. Cataract surgeons must apply the same reasoning for laser corneal incisions and avoid them in FFKC and KC. Thisseems obvious, but there are cataract surgeons who do not routinely use topography for their refractive cataract surgery. I have seen one case of ectasia following arcuate incisions.
For patients with KC or FFKC, I have had good results using toric IOLs (when astigmatism is regular and reproducible centrally), so I avoid corneal laser arcuate incisions in these cases.
MARFAN SYNDROME/ECTOPIA LENTIS
Cataracts with significant sectoral zonular loss present significant challenges. They typically require a capsular tension ring at the least and usually one or two sutured Ahmed CTSs (Morcher, US distributor FCI Ophthalmics). I have found that the laser can really help with the capsulotomy, which is challenging using a manual approach (Figure 2). The laser capsulotomy can be centered on the dislocated lens and kept on the smaller size. This allows me to skip placing multiple capsular hooks, which are typically necessary during a manual capsulotomy, and to proceed right to a CTS secured with Gore-Tex sutures (W.L. Gore Associates; off-label usage), even before nuclear emulsification.
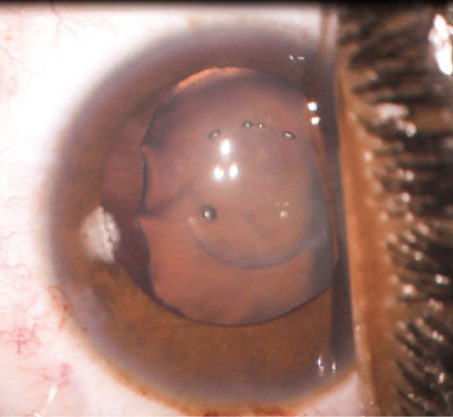
Figure 2. The laser helps Dr. Raviv complete a challenging part of cataract surgery on a patient with Marfan syndrome.
There have been reports of increased capsular tear-outs with early laser platforms4 but with the newest software and latest energy parameters, I believe laser capsulotomy is as secure as a manual capsulorhexis and may decrease complications.5,6
WHITE CATARACTS
White cataracts would seem the perfect scenario for using a laser capsulotomy, and usually they are. However, with intumescent cataracts (dark intralenticular clefts can be seen on the OCT scan), the risk of an incomplete laser capsulotomy remains.7,8 The laser capsulotomy may penetrate the lens capsule in one area first and cause a decompression that moves the lens away from the remaining capsulotomy shots. My approach is to adjust the laser settings to allow for the most rapid capsulotomy, close to 0.5 seconds. This can be done by making the capsulotomy smaller6 and by increasing the vertical spot spacing. Still, a surgeon must be prepared to complete the capsulotomy manually.
PATIENT FACTORS, OTHER SITUATIONS
Without the benefit of anesthesia, it may be difficult to dock the laser on the eyes of certain patients or to keep them from moving if the femtosecond laser is located outside the OR. I typically avoid using the laser in patients with dementia, kyphoscoliosis, or a large filtering bleb. I find the technology helful in cases of nystagmus. In eyes with a dense cataract, a shallow chamber, or zonular weakness, the use of the laser is a no-brainer; in my hands the technology offers a tremendous advantage over standard phacoemulsification.9,10
CONCLUSION
In my experience, the femtosecond laser can be a great asset in complex cataract surgery. At times, however, I find it necessary to modify my usual parameters or to avoid certain laser incisions.
1. Alder BD, Donaldson KE. Comparison of two techniques for managing posterior polar cataracts: Traditional phacoemulsification versus femtosecond laser-assisted cataract surgery. J Cataract Refract Surg. 2014;40(12):2148-2151.
2. Vasavada AR, Vasavada V, Vasavada S, et al. Femtodelineation to enhance safety in posterior polar cataracts. J Cataract Refract Surg. 2015;41(4):702-707.
3. Titiyal JS, Kaur M, Sharma N. Femtosecond laser-assisted cataract surgery technique to enhance safety in posterior polar cataract. J Refract Surg. 2015;31(12):826-828.
4. Abell RG, Davies PE, Phelan D, et al. Anterior capsulotomy integrity after femtosecond laser-assisted cataract surgery. Ophthalmology. 2014;121(1):17-24.
5. Scott WJ, Tauber S, Gessler JA. Comparison of vitreous loss rates between manual phacoemulsification and femtosecond laser-assisted cataract surgery. J Cataract Refract Surg. 2016;42(7):1003-1008.
6. Thompson VM, Berdahl JP, Solano JM, Chang DF. Comparison of manual, femtosecond laser, and precision pulse capsulotomy edge tear strength in paired human cadaver eyes. Ophthalmology. 2016;123(2):265-274
7. Taravella MJ, Meghpara B, Frank G, et al. Femtosecond laser-assisted cataract surgery in complex cases. J Cataract Refract Surg. 2016;42(6):813-816.
8. Conrad-Hengerer I, Hengerer FH, Joachim SC, et al. Femtosecond laser-assisted cataract surgery in intumescent white cataracts.J Cataract Refract Surg. 2014;40(1):44-50.
9. Schultz T, Dick HB Laser-assisted mini-capsulotomy: a new technique for intumescent white cataracts. J Refract Surg. 2014;30(11):742-745.
10. Martin AI, Hodge C, Lawless M, et al. Femtosecond laser cataract surgery: challenging cases. Curr Opin Ophthalmol. 2014;25(1):71-80.