
In today’s MIGS landscape, there are many device options with good safety and efficacy profiles for patients undergoing combined cataract and MIGS surgery. However, those same devices are not approved for use outside the combined cataract surgery setting, and many insurance programs, including Medicare, do not cover standalone procedures. That is until the OMNI Surgical System (Sight Sciences) entered the marketplace. Having a device available for both phakic and pseudophakic patients that has excellent safety and efficacy has changed the way we approach glaucoma surgical interventions.
Using the OMNI for standalone patients to lower IOP and reduce the dependency on prescription eye drop medications is extremely valuable. For MIGS-trained surgeons, OMNI is a single intelligently designed MIGS device that combines two implant-free titratable procedures—canaloplasty and trabeculotomy (Figure)—and effectively targets all three points of resistance in the conventional outflow pathway, with or without cataract surgery.

Figure. Canaloplasty and trabeculotomy with the OMNI Surgical System.
Outflow Pathway Resistance
There are several surgical options available that specifically address one area of resistance. We know that the trabecular meshwork (TM) is the most commonly targeted area of resistance in the outflow pathway, which is why stent procedures can be effective. However, the TM is not the only place of possible resistance. Up to 50% of resistance is located in Schlemm canal and the distal collector channels.1-3 As a result, if you haven’t addressed further down the pathway, including the collector channels, then you will not achieve maximum efficacy. Having the ability to address all three areas of resistance within the outflow pathway with one procedure substantially increases the likelihood you will find the most critical area of resistance for that particular patient and achieve the desired efficacy.
OMNI in Standalone Cases—What Surgeons Should Know
The first and most crucial area surgeons should examine is the angle. Make sure it is wide open and that there are no peripheral anterior synechiae that would make access to Schlemm canal difficult. The other area of focus is to ensure there is no neovascularization in the angle or other angular abnormality that would hinder the successful deployment of the device and dilation of the collector system.
With any surgical procedure, patient education is paramount and should be regarded as the first line of treatment. The advantages versus the current treatment regimen, including the goals and expectations of surgical intervention, should be clearly explained and defined. In many cases, we are trying to achieve two things: better control of IOP and a reduced or eliminated dependency on medicated drops, which patients find most appealing and is a prime reason they choose to have the procedure.
Expectations & Outcomes
The goal is to set the patient’s expectations appropriately, and we dispel the idea that the surgery will cure their disease. We explain that the surgical process will not eliminate the need for regular pressure checks or even future medical or surgical intervention—as glaucoma cannot be cured, at least not today—but it will provide us a safe and effective way to manage the pressure to reduce the risk of long-term, progressive damage to the optic nerve. We emphasize that OMNI is a minimally invasive intervention with long-term effects, but that the natural process of the disease may require further intervention. We want patients to understand that the measures performed during an OMNI procedure are a critical step in their lifelong journey in the management of their glaucoma disease.
Our outcomes are based on the specific goals of each patient. There are several scenarios we see repeatedly. If a patient is taking several medications and the IOP is not adequately controlled, then we target a 20% drop in IOP. If the patient’s IOP is adequately controlled, but they are having issues with administering medicated drops or having ocular surface issues, then our target is to maintain pressure but reduce the dependency on the medicated drops.
As a cataract/refractive surgeon who also treats glaucoma, I see a fair number of patients who have already had cataract surgery and who would also benefit from a MIGS procedure to address their glaucoma. These are great cases where OMNI stands above and beyond. With OMNI, surgeons can offer phakic and pseudophakic patients a safe and effective option that reduces and stabilizes IOP while reducing or removing medication use. OMNI also allows us to possibly avoid more aggressive surgical interventions down the road.
Patient Case Study
An exemplary case demonstrating the versatility of OMNI can be appreciated here. During our patient education and treatment plan discussion, we concluded that the patient would need cataract surgery in the future. Placing her on further topical medications was not a great option as she was already showing signs of dry eye disease and complained of redness and irritation with her current medications. A laser or surgical intervention could help avoid more preservative-containing medications. We discussed selective laser trabeculoplasty but decided on OMNI to target a significant enough reduction in IOP along with the potential for a decrease in topical medications, leaving the option of a stent or additional MIGS procedure at the time of her future cataract surgery. When we do address her cataract, we can determine if she will need further glaucoma intervention at that time, or if her IOP is stable with reduced medications. We decided to proceed with a plan for OMNI, performing 360° canaloplasty and 180° trabeculotomy, leaving 180° for a future stent procedure.
Patient Presentation
- Early mild cataract and primary open-angle glaucoma
- Prescribed tafluprost ophthalmic solution (Zioptan, Santen), timolol ophthalmic solution, and brimonidine tartrate ophthalmic solution
- Patient experienced difficulties with compliance and complained of unacceptable hyperemia and itching
- Evidence of the progression of glaucoma disease showed on OCT and Humphrey visual field (Figure)
- IOP of 21 mm Hg OU
- BCVA of 20/25 with no complaints of glare or halos at night
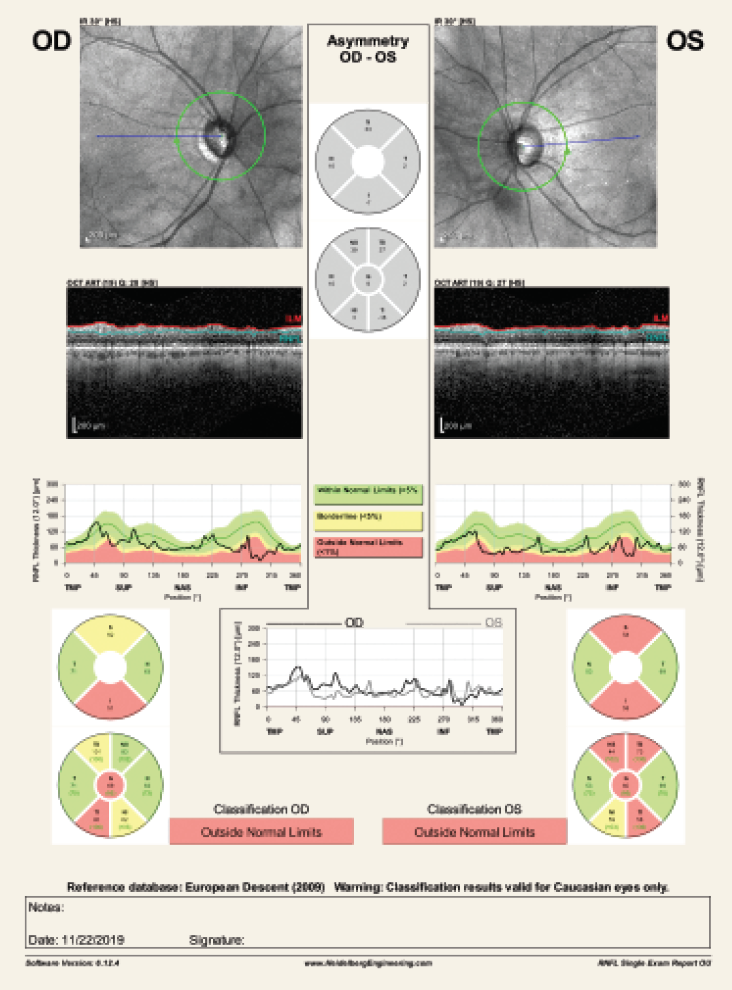
Figure. Patient pre-surgery OCT and Humphrey visual field.
Postoperative Results
- 1 Week: IOP was 10 mm Hg (OD), 15 mm Hg (OS on timolol)
- 2 Weeks: IOP was 14 mm Hg (OD); no data OS
- 1 month: IOP was 14 mm Hg (OD), 15 mm Hg (timolol OS only)
- 3 months: IOP 16 mm Hg (OU at an outside practice due to COVID-19)
- 5 months: 16 mm Hg (OD), 13 mm Hg (OS with stable visual field and OCT on timolol OU)
Case Conclusion
Due to COVID-19, this patient was followed outside of my practice, but we were able to confirm that she was seen locally, and her pressure is stable at 16 mm Hg from a previous 21 mm Hg.
Conclusion
Having a standalone procedure for phakic and pseudophakic patients is valuable. The average age of patients undergoing cataract surgery has been steadily declining. As a result, a number of patients are undergoing cataract surgery well before their glaucoma progresses to the stage of requiring intervention. Thus, our patients will benefit from having the option of a MIGS procedure after having cataract surgery. Until now, we haven’t had an efficacious intervention option, like OMNI, to offer our patients that provides a covered, less invasive way to lower IOP or reduce medication burden as an alternative to more invasive surgical procedures. Having additional effective and safe standalone glaucoma interventions is vital in serving the needs of a growing population of phakic and pseudophakic patients with glaucoma.
1. Grant WM. Experimental aqueous perfusion in enucleated human eyes. Arch Ophthalmol. 1963;69:783-801.
2. Rosenquist R, Epstein D, Melamed S, et al. Outflow resistance of enucleated human eyes at two different perfusion pressures and different extents of trabeculotomy. Curr Eye Res. 1989;8(12):1233-1240.
3. Battista SA, Lu Z, Hofmann S, et al. Reduction of the available area for aqueous humor outflow and increase in meshwork herniations into collector channels following acute IOP elevation in bovine eyes. Invest Ophthalmol Vis Sci. 2008;49(12):5346-52.
OMNI® Surgical System
IMPORTANT PRODUCT INFORMATION:
Indications for Use
The OMNI® Surgical System is indicated for canaloplasty (microcatheterization and transluminal viscodilation of Schlemm’s canal) followed by trabeculotomy (cutting of trabecular meshwork) to reduce intraocular pressure in adult patients with primary open-angle glaucoma.
Contraindications
Do not use the OMNI® in any situations where the iridocorneal angle is compromised or has been damaged (e.g., from trauma or surgery), since it may not be possible to visualize the angle or to properly pass the microcatheter.
Do not use the OMNI® in patients with angle recession; neovascular glaucoma; chronic angle closure; narrow-angle glaucoma; traumatic or malignant glaucoma; or narrow inlet canals with plateau iris.
Do not use the OMNI® Surgical System in quadrants with previous MIGS implants.
Please refer to the full Instructions For Use, available at omnisurgical.com, for warnings, precautions, and adverse event information.
© 2020 Sight Sciences, Inc. 6/21 OM-1167-US.v1


