CASE PRESENTATION
A 49-year-old man with blurry vision in his left eye presents for a cataract consultation. The patient is a commercial airline pilot, and by Federal Aviation Administration (FAA) requirements, his visual acuity must be correctable to 20/20 OU. Although his current BCVA is 20/20, he had some difficulty passing his most recent FAA physical exam. The patient would like to resolve the problem before it prevents him from passing the exam and flying. He is also bothered by a decline in the vision in his left eye and experiences some glare. He would like to improve his quality of vision and night vision.
The patient’s ocular history is notable for keratoconus in the left eye, which was treated outside the United States with CXL followed by the placement of one intrastromal corneal ring segment (ICRS; Keraring, Mediphacos) and topography-guided PRK. He wears a distance soft contact lens on the left eye to fly. By FAA requirements, his monocular corrected distance and near visual acuity must be 20/20, so he keeps his readers available when flying. Given that the right eye is phakic with 20/15 and J1 UCVA, he does not wear reading glasses outside of the cockpit.
Upon presentation, the patient’s UCVA is 20/15-2 and J1-2 OD. His UCVA is 20/40-3 and J16 OS. His BCVA is 20/20-2 OS with a manifest refraction of +2.00 -2.75 x 104º. With glare testing, the visual acuity in his left eye is light perception.
An examination finds a normal right eye. In the left eye, one ICRS is located inferiorly and surrounded by stromal scarring, and the central visual axis is clear. A fundus examination of the left eye finds a retinal tear that has received laser treatment as well as the postoperative scarring and pigmentation one would expect. Preoperative testing results are shown in Figures 1 to 4.

Figure 1. Pachymetry analysis of the patient’s eyes.

Figure 2. Corneal topography with the Pentacam.

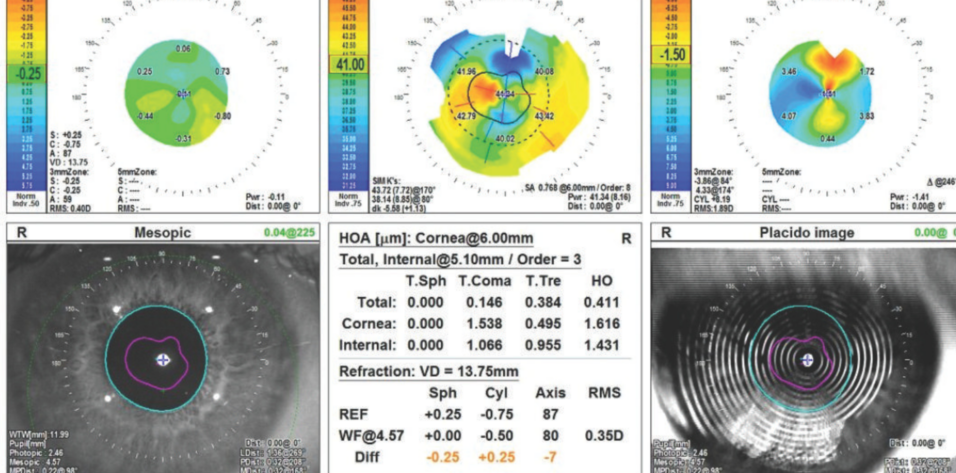
Figure 3. Corneal analysis of the right (A) and left (B) eyes with the OPD-Scan (Nidek).

Figure 4. Biometry measurements.
The patient is intrigued by the possibility of spectacle independence but understands that his options may be limited by his profession and complex ocular pathology. He is willing to wear glasses or contact lenses after cataract surgery or to undergo a PRK enhancement.
What IOL and refractive targets would you recommend? If you favor a monofocal lens, which one would you recommend given the patient’s history of PRK, ICRS placement, and keratoconus? How would you perform the IOL power calculation; which formula would you use? Would you consider a Light Adjustable Lens (LAL; RxSight)? How would the presence of scarring affect your surgical plan?
—Case prepared by Neda Nikpoor, MD

SUMITRA S. KHANDELWAL, MD
The patient’s history of several corneal procedures combined with underlying corneal disease renders keratometry and IOL power calculations challenging. The presence of an ICRS surrounded by haze suggests the eye may have higher-order aberrations (HOAs) and a propensity toward glare regardless of the cataract. I would therefore be reluctant to offer a trifocal or bifocal IOL. Additionally, I would prefer to avoid an extended depth of focus IOL that would reduce his contrast sensitivity. Although a small-aperture IOL can be an option for individuals with irregular corneas, I would avoid this style of lens and any other that could dim the patient’s nighttime vision.
Instead, I would recommend a monofocal toric lens, ideally an aspheric design. I would offer a toric model because his refraction matches what is shown on topography and the axis of corneal astigmatism found with biometry. An LAL would be a reasonable alternative, but I would speak with the patient about his goals. If he desires the crispest possible distance vision with no HOAs, I would limit the first postoperative adjustment of the LAL to less than 0.50 D. This would curtail the depth of focus delivered by the LAL but also avoid HOAs. That said, based on the patient’s history, he may be willing to accept some HOAs. If so, the first LAL adjustment would be greater than 0.50 D to increase depth of focus.
Another possible option would be an IC-8 Apthera lens (Bausch + Lomb). Its pinhole optic might correct the patient’s irregular astigmatism and provide an extended depth of focus. The most common complaint with this lens, however, is dim nighttime vision. I therefore would not recommend an Apthera lens to this patient until and unless the FAA issues guidance allowing the IOL’s use in pilots.
Scarring from the ICRS may compromise the view for performing LAL adjustments. The good news from the preoperative exam is that the central visual axis seems to be clear. The timing of treatment could also present a challenge. I often perform the first adjustment as early as 3 weeks postoperatively, but a delay may be required for this patient. He would be asked to return to the office 4 and 6 weeks after surgery to check his refraction and to commit to wearing UV protection during this time. I would ask my most skilled technician to refract the patient at each visit because astigmatism measurements can fluctuate in keratoconic eyes.

PRIYA M. MATHEWS, MD, MPH
First, I would perform a thorough slit-lamp examination and assess the placement and stability of the ICRS. If any part of the ICRS appears to be on the verge of extruding, I would discuss with the patient possible removal of the device, followed by stabilization of the cornea, before refractive cataract surgery.
Assuming that the ICRS is embedded and stable, I would describe the various options for cataract surgery to the patient. Given the unpredictability of IOL calculations due to keratoconus, prior PRK, and the presence of an ICRS, I would recommend an LAL if the patient desires some degree of spectacle independence. A monofocal toric lens could also be considered because the magnitude and axis of astigmatism are consistent between the Pentacam (Oculus Optikgeräte) and IOLMaster (Carl Zeiss Meditec). There would be a high margin of error, however, so the patient would have to be prepared to wear corrective lenses after surgery.
Emmetropia would be the target if the patient prioritizes optimal distance vision. Alternatively, -0.50 D could be targeted in the nondominant eye to provide some degree of reading vision; this could be refined if an LAL is implanted. I would calculate the lens power with multiple formulas, including the Barrett True-K, Barrett Keratoconus, and Kane Keratoconus.
The LAL would be my strong preference for this patient, particularly given his age and profession.

P. DEE STEPHENSON, MD, FACS
The thinness of the cornea and the presence of an ICRS, a stromal scar, and a retinal tear warrant concern. For toric correction, I typically employ the Barrett True-K toric formula. For patients with keratoconus, regardless of whether they have an ICRS, I prefer the Kane formula. Given this patient's history of PRK, I would likely use the ASCRS post-refractive IOL calculator and perform intraoperative aberrometry with the ORA System (Alcon). The retinal tear treated with a laser is a contraindication for the IC-8 Apthera, and the patient’s need for good night vision makes this lens a suboptimal choice. Instead, I would consider implanting either an enVista Aspire toric lens (Bausch + Lomb), which induces minimal spherical aberration, or an enVista IOL (model MX60ET, Bausch + Lomb), which is aspheric and induces no spherical aberration. Both IOLs are designed to deliver excellent intermediate visual acuity. Targeting -0.50 D sphere might offer the patient some near vision as well.
Although he has 2.00 D of against-the-rule astigmatism, his keratoconus makes me hesitate to offer a toric monofocal IOL. Given the thin cornea, an LAL would be a viable choice, and its postoperative adjustability would be an advantage.

WHAT I DID: NEDA NIKPOOR, MD
As the panelists articulate beautifully, there are several key points to consider in this case. Given the patient’s profession as a pilot and his irregular cornea due to keratoconus, I advised him against selecting an extended depth of focus, multifocal, or small-aperture lens. Instead, I recommended either an LAL or a toric monofocal lens. I explained that the LAL was more likely to achieve the refractive target because of his complex cornea. I also noted, however, that there was a small chance that scarring would obstruct the postoperative light adjustments or that this altered pattern of light could result in HOAs that reduced his BCVA. I explained that the LAL could be exchanged for a monofocal lens if either of these scenarios occurred. I counseled the patient that the implantation of a toric monofocal lens (an enVista for the reasons Dr. Stephenson outlines) would not induce HOAs and that his postoperative recovery would probably be quicker with this option, but I also noted that he was more likely to need glasses or contact lenses for optimal vision after surgery.
The patient and I discussed the pros and cons of his IOL options at length. Ultimately, he chose the toric monofocal lens with a refractive target of distance/plano with the understanding that he could consider a PRK enhancement in the future.
Using the Zeiss Veracity Surgery Planner (Carl Zeiss Meditec), I compared IOL calculations with the Barrett True K Toric and Kane formulas as well as the software’s built-in post–myopic PRK calculator. Measurements were obtained on 2 separate days while the patient received treatment to optimize the ocular surface. The IntelliAxis feature on the Ally Adaptive Cataract Treatment System (Lensar) allowed me to align the IOL on the implantation axis I selected, and I confirmed IOL power with the ORA system.
Six weeks after surgery, the patient’s UCVA was 20/15-2 OS. He had a residual refractive error of +0.25 -1.00 x 136º that was correctable to 20/15. The UCVA in his fellow eye was 20/15-2. The patient achieved spectacle independence at distance and was highly satisfied with his outcome.