Although awareness of Demodex blepharitis has increased among eye care practitioners, Demodex infestations are still underdiagnosed and often misunderstood. This is important because if we see signs of Demodex infestation and offer a blanket diagnosis of blepharitis and standard treatments, then treatments will not work. The inflammatory effects will continue, affecting the patient’s ocular health and quality of life. In fact, it is common to see the condition among patients referred to us for dry eye disease, where the absence of a Demodex diagnosis has been the primary reason that previous dry eye treatments were not fully effective.
To treat this very common problem, first we need to diagnose it. The good news is that it’s easy to see Demodex blepharitis—examine the superior lid margin at the slit lamp with the patient’s eyes closed and look for collarettes.
What Is Demodex Blepharitis?
Demodex is the most common ectoparasite that lives on human skin. There are two species of Demodex: D. folliculorum and D. brevis. The smaller species, D. brevis (about 0.15 to 0.2 mm in length), live in the meibomian glands.1 D. folliculorum are twice as large as D. brevis (about 0.3 to 0.4 mm long)1 and live in the hair follicles. Both types of Demodex are commonly found in the eyelashes and eyebrows and around the nose, and they both have a lifecycle of about 14 to 18 days.2
Sometimes, the Demodex population multiplies to become an infestation, causing an inflammatory pathological condition of the eyelid called Demodex blepharitis. The reasons for this change are not completely understood, but Demodex blepharitis likely involves both D. brevis and D. folliculorum. The smaller D. brevis are difficult to detect, but in the meibomian glands, they contribute to inflammation and clogging.2 Unlike D. brevis, D. folliculorum are visible to the naked eye. More importantly, the products of D. folliculorum, called collarettes or cylindrical dandruff, are quite evident when you look in the right place.
Burrowed densely together deep inside the eyelash follicles, D. folliculorum consume epithelial cells and sebum in a process of external digestion. Their large salivary glands release proteases and lipases, and then the Demodex absorbs most of the digested cellular material. Although Demodex have no excretory system, this process does produce waste in the form of follicular dandruff and lipids, which collect in collarettes around the base of the eyelashes. The collarettes are composed of undigested material, combined with epithelial cells, keratin, digestive proteases and lipases, and Demodex eggs. This process continues for the life of the mite, which itself becomes part of the lash debris every 14 to 18 days.
Demodex infestation causes blepharitis in part through this process—the release of enzymes in the hair follicles, destruction of epithelial cells, exudation of digestive waste when they die, and ongoing presence of all of these accumulated chemicals and waste in collarettes on the lid margin. Dead mites and collarettes can also obstruct the hair follicle opening, leading to further inflammation.
Other factors contribute to inflammation as well. First, Demodex have eight legs that scrape the lash and the lid margin throughout its process of feeding, growth, and reproduction (Figure 1). That mechanical damage triggers inflammation. Demodex mites can also carry bacteria on their surface or in their gut that contribute to inflammation.
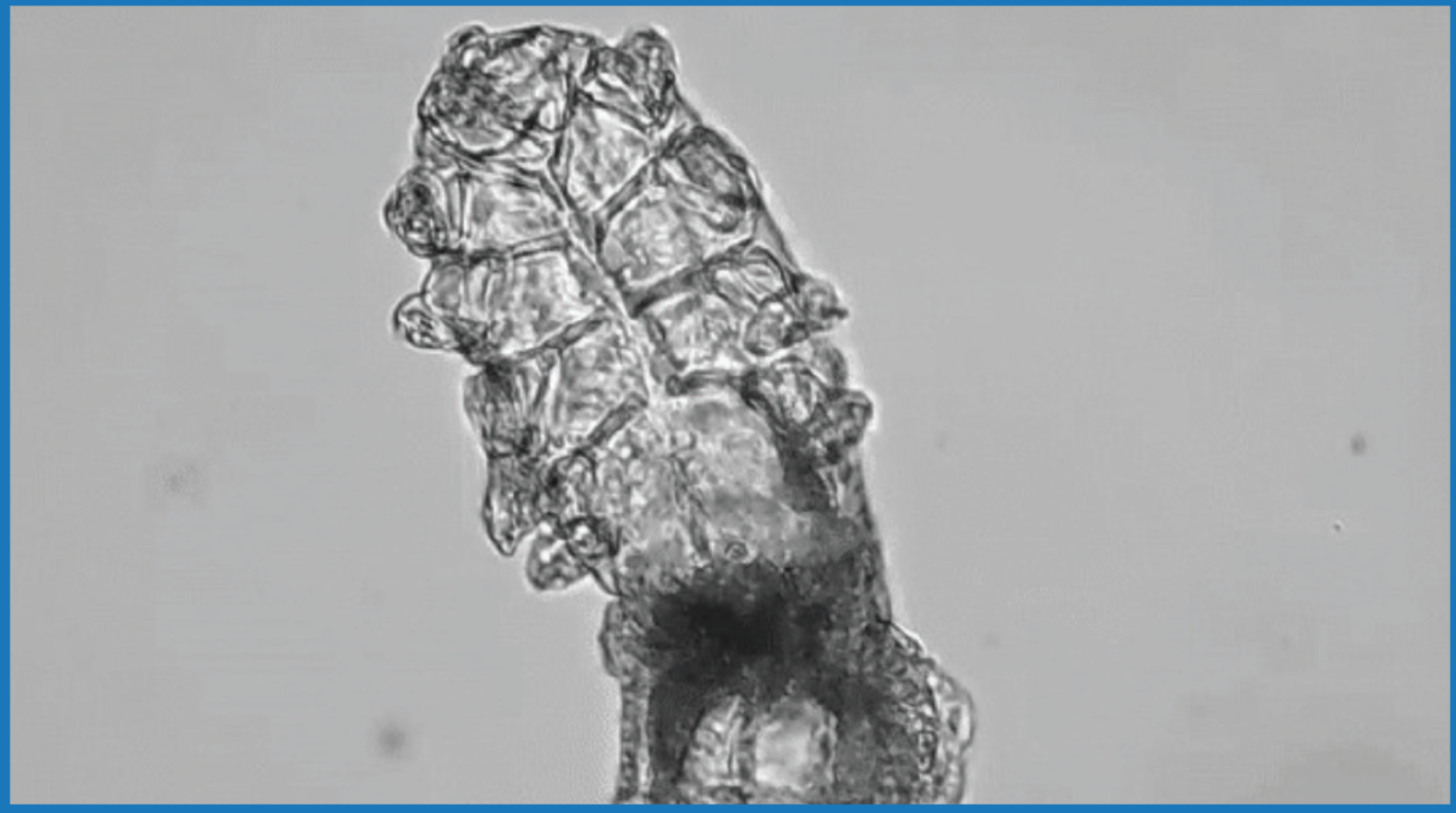
Figure 1. This is a magnified image of a Demodex mite, which spends its entire life cycle burrowed into the eyelash follicles. Its process of eating epithelial cells and sebum, reproducing, and creating waste produces collarettes around the eyelashes.
All of this mechanical, chemical, and bacterial damage triggers an immune response in an effort to heal the eyelids, including the release of inflammatory cytokines. It contributes to ocular surface inflammation, too, evidenced by significantly higher tear matrix metallopeptidase 9 (MMP-9) testing in patients who are positive for Demodex infestation.3 We see patients with itchy, red-rimmed lids, which we might easily diagnose as general blepharitis, if we are not aware of the clinical significance of collarettes as a visible sign of Demodex blepharitis.
Why Does Demodex Blepharitis Occur?
Demodex mites, are a normal part of the body’s biome. What makes the normal Demodex population turn into an infestation with pathological consequences? The precise reasons are not completely understood, but overpopulation is more common in patients of advanced age and in the presence of certain underlying conditions.
Much like bacteria that reside on our bodies in normal numbers, Demodex mites can multiply beyond healthy levels when the body cannot control them as it normally would. One of the problems allowing that to happen may be the natural weakening of the immune system that occurs with aging. Demodex mites are present at all ages, but the number of D. folliculorum and D. brevis increase directly with age.4 One study showed that Demodex infestation is present in about 84% of people at age 60 and 100% of people over 70.5 The same way natural changes to the immune system make older patients more susceptible to various health problems, these changes also seem to make patients more susceptible to Demodex infestation.
In addition, patients with diabetes are significantly more likely to have Demodex infestation,6 and that likelihood is higher if their blood glucose is not controlled.7 Diabetes is a chronic inflammatory condition that lowers immune function, so the immune system may not be able to maintain healthy levels of Demodex. In one study, patients with type 2 diabetes had significantly lower natural killer cell activity compared to non-diabetics (768.01 vs. 2,435.31).8 This decline makes diabetics more susceptible to infection, and it may also mean that their bodies cannot counteract overpopulation of Demodex.
The skin condition rosacea is also associated with higher rates of Demodex infestation.9 This chronic inflammatory condition, characterized by facial redness, inflammation, papules, and telangiectasia, often includes the eyelid area in the inflammatory picture. A meta-analysis of 1,513 patients showed those with erythematotelangiectatic or papulopustular rosacea were nine times more likely to have Demodex mite infestation than patients without rosacea.10 Demodex infestation may have a cause or effect relationship with rosacea; perhaps the condition permits the mite population to grow, or perhaps Demodex infestation is an underlying cause of the condition. Importantly for lid margin disease, in patients with rosacea, one of the highest densities of Demodex is found in the ocular adnexa.11
Clinical Signs of Demodex Blepharitis
Symptoms of Demodex blepharitis are similar to other inflammatory eye conditions, including other types of blepharitis and ocular surface disease. Patients might feel discomfort, dryness, itching, or burning. Some patients, particularly older people who may regard discomfort as a normal part of aging, might not complain about their symptoms. As a result, it is important to always screen for signs of the condition. Clinical signs of Demodex blepharitis include the mites’ direct impacts, as well as sequelae from chronic inflammation:
Collarettes – The telltale clinical sign of Demodex blepharitis is collarettes. In fact, Demodex mites are found on 100% of lashes with collarettes (Figure 2).12 Collarettes can contribute to symptoms by creating a gritty feeling on the lids, and they may be unsightly.
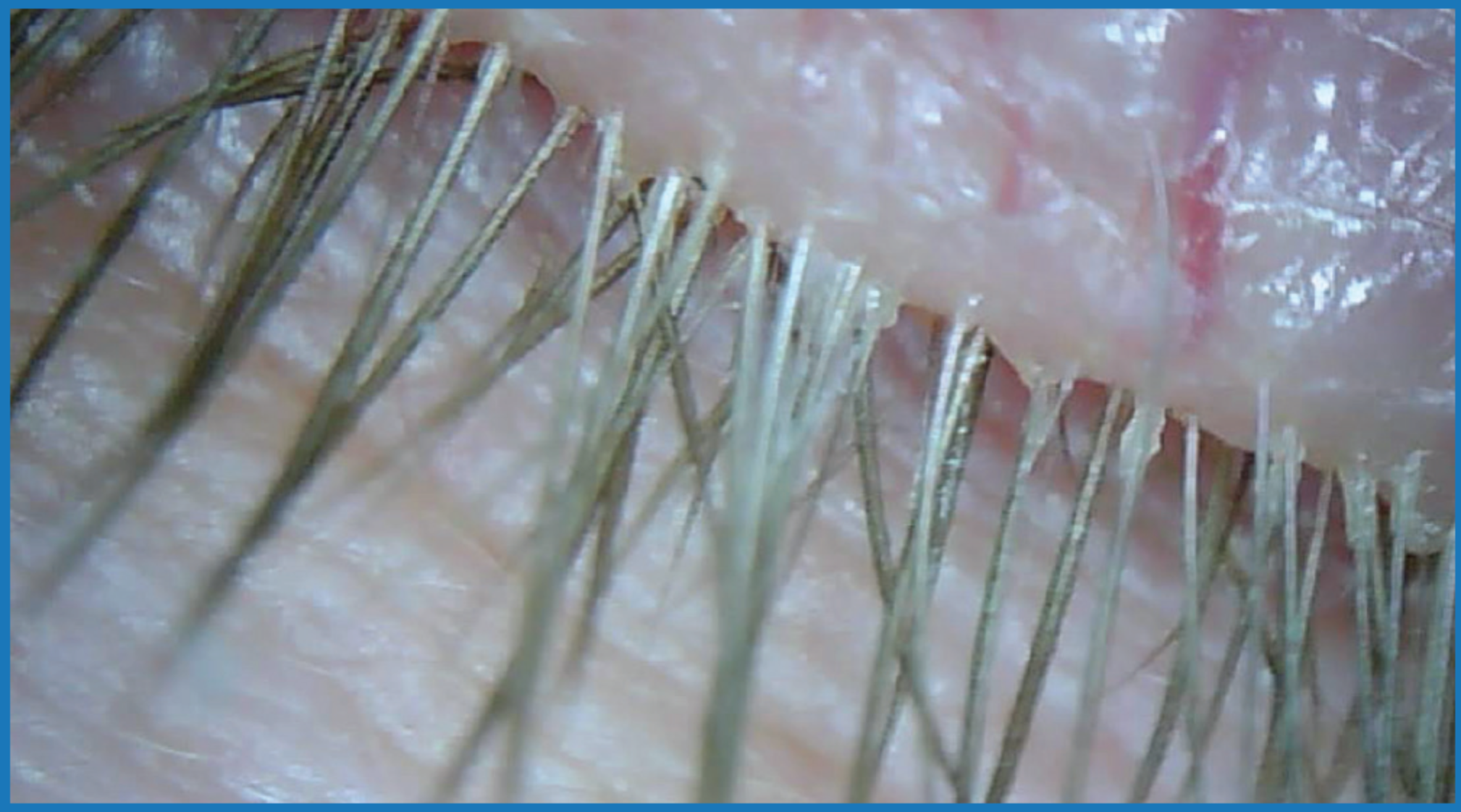
Figure 2. Slit-lamp examination of the closed eye reveals collarettes along the upper lid margin. One hundred percent of patients with collarettes have Demodex blepharitis, making them the telltale clinical sign that Demodex infestation is the underlying cause of the condition.
Photo courtesy of Leslie O'Dell, OD, FAAO
Collarettes have a very specific appearance that’s easy to identify. These cylindrical deposits look like waxy plugs around the base of the eyelashes at the lid margin. They also can migrate up the lash. They do not resemble the flaky skin on the lid margins we see with seborrheic blepharitis. Collarettes can be physically difficult to remove, even with micro-exfoliation, and will not dissolve with warm compresses. When the collarettes are exfoliated, the tails of the Demodex mites are visible protruding from the hair follicles under the slit lamp.
It’s important to note that for routine screening, there is no need to epilate an eyelash and count the mites. Collarettes can be seen with a routine slit-lamp exam just as reliably as epilating and using a microscope. If you have patients close their eyes at the slit lamp, you can get a good look at the lash follicles on the upper lid, which is typically where you will find collarettes. Collarettes are highly correlated with Demodex blepharitis and are, in fact, caused only by Demodex infestation, so their presence is enough to tell us with very high confidence that Demodex blepharitis is the problem. From our perspective, epilation just causes unnecessary trauma for the patient and adds time to the exam.
Lash distension or loss – As Demodex mites eat, lay eggs, and die, they add bulk inside the eyelash follicles. It is common to see a distended lash pulled down, which can be an irritant in itself. Some patients have lash thinning and lost eyelashes, or madarosis.
Eyelid redness – Lid margin inflammation, evidenced by red eyes and eyelids, is a frequent complaint of patients with Demodex blepharitis. They have typically tried artificial tears to reduce redness, to no avail. The red eyelids affect their appearance, which is distressing. It also affects their social interactions, and they get tired of people asking, “What’s wrong with your eyes?” These signs of inflammation are often accompanied by symptoms of dryness and discomfort.
Recurrent styes or chalazia – It makes sense that a mite that infests the lash follicle can obstruct the follicle and cause recurrent styes. Similarly, recurrent chalazia from blocked meibomian glands are common among patients with Demodex blepharitis, likely a result of debris from both D. brevis and D. folliculorum. These signs can be present in young patients as well as old, so it’s important to examine young patients with these recurrent problems for the presence of collarettes.
Changes to the lid tissue – When Demodex blepharitis is not treated effectively, the lid margin will thicken over time. This may be a direct result of Demodex or part of a larger picture where the Demodex contributes to both posterior and anterior blepharitis. This fits what we already know about how meibomian gland dysfunction affects eyelid morphology. Women often notice while applying makeup that the lid margin is no longer a smooth curve.
Corneal scarring – Chronic, progressive Demodex blepharitis contributes to keratoconjunctivitis, which in turn can result in damage to the corneal epithelium visible with staining. This sign of Demodex blepharitis is a downstream effect, so it is most likely to be seen in patients who have gone some time without diagnosis or treatment for chronic inflammation.
Just as a history of related systemic conditions helps us identify those at greater risk for Demodex blepharitis, familiarity with the condition’s signs can help us identify it accurately. The “nice part” of collarettes is that they allow us to make the diagnosis, even in the absence of patient complaints. That’s important because we want to work efficiently, but it’s most important because if we can break down Demodex blepharitis screening into simple collarette identification, then we can make screening a routine part of every eye exam to ensure we understand the underlying cause of disease.
Seeing What’s in Plain Sight
Despite the prevalence of Demodex blepharitis and the clear sign it presents with collarettes, eye care practitioners are not screening for the problem on a consistent basis, particularly if the patient is not complaining. When we ask colleagues to estimate how many of their patients with blepharitis have Demodex infestation, they usually say the number is about 10 to 15%. But according to a meta-analysis of nearly 5,000 cases, 45% of blepharitis cases involve Demodex infestation.13 And in a sequential assessment of over 1,000 patients across eight ophthalmic practices, 55% of patients presented with some amount of collarettes, regardless of the reason for their visit.14
When we don’t try to characterize lid disease, blepharitis becomes a blanket diagnosis where we might micro-exfoliate and give patients instructions for warm compresses and lid scrubs like hypochlorous acid. Instead, we need to be able to identify collarettes at the slit lamp and know that they indicate Demodex blepharitis, just as other characteristics indicate angular blepharitis or involvement of bacterial infection. This is very similar to how we characterize ocular surface disease before making a treatment plan.
The consequences of offering basic treatments that don’t target the underlying cause of Demodex blepharitis are some of the sequelae from chronic inflammation that we consider signs of the condition, such as recurrent hordeolum, recurrent chalazion, and eventual eyelid changes and damage to the corneal surface. There are also significant potential problems for patients who will have cataract or refractive surgery in the future. Untreated Demodex blepharitis is common in senior populations across the board, and when those patients need cataract surgery, for example, the best outcomes are not possible without first treating the Demodex blepharitis. We need to bring inflammation under control and restore the tear film functionality in advance of surgery, particularly if the condition has become advanced, in order to meet high expectations for both visual outcomes and postoperative comfort.
We are all still learning about Demodex. Practitioners who have been seeing patients for decades may not see the need to break down the characteristics of a patient’s blepharitis and know that Demodex infestation is the specific cause, but the reality is that the only way for treatment to succeed is to identify Demodex blepharitis and target the underlying cause. It’s rewarding to bring relief to patients who have struggled with warm compresses and other symptomatic treatments. And perhaps most exciting is the relative ease with which we all can identify Demodex blepharitis by the telltale presence of collarettes and ensure that more patients get the help they need to prevent permanent damage.
1. McBain AJ, O’Neill CA, Oates A. (2016). Skin Microbiology. Elsevier. https://doi.org/10.1016/b978-0-12-801238-3.99217-1
2. Liu J, Sheha H, Tsenga SCG. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol. 2010; 10(5): 505-510. (Accessed online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2946818/)
3. Zhang XB, Ding YH, He W. The association between demodex infestation and ocular surface manifestations in meibomian gland dysfunction. Int J Ophthalmol. 2018;11(4):589-592. (Accessed online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5902361/)
4. Zhong J, Tan Y, Li S, et al. The Prevalence of Demodex folliculorum and Demodex brevis in Cylindrical Dandruff Patients. J Ophthalmol. 2019;2019:8949683. (Accessed online: https://www.hindawi.com/journals/joph/2019/8949683/)
5. Post CF, Juhlin E. Demodex Folliculorum and Blepharitis. Arch Dermatol. 1963;88:298-302.
6. Yamashita LS, Cariello AJ, Geha NM, et al. Demodex folliculorum on the eyelash follicle of diabetic patients. Arq Bras Oftalmol. 2011;74(6):422-424. (Accessed online: https://www.scielo.br/scielo.php?script=sci_arttext&pid=S0004-27492011000600008)
7. Gökçe C, Aycan-Kaya O, Yula E, et al. The effect of blood glucose regulation on the presence of opportunistic Demodex folliculorum mites in patients with type 2 diabetes mellitus. J Int Med Res. 2013;41(5):1752-1758. (Accessed online: https://journals.sagepub.com/doi/10.1177/0300060513494730)
8. Kim JH, Park K, Lee SB, et al. Relationship between natural killer cell activity and glucose control in patients with type 2 diabetes and prediabetes. J Diabetes Investig. 2019;10(5):1223-1228. (Accessed online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6717814/)
9. Kubanov A, Gallyamova Y, Kravchenko A. Clinical picture, diagnosis and treatment of rosacea, complicated by Demodex mites. Dermatol Reports. 2019;11(1):7675.
10. Chang YS, Huang YC. Role of Demodex mite infestation in rosacea: A systematic review and meta-analysis. J Am Acad Dermatol. 2017;77(3):441-447.e6. (Accessed online: https://www.jaad.org/article/S0190-9622(17)30429-2/fulltext)
11. el-Shazly AM, Ghaneum BM, Morsy TA, et al. The pathogenesis of Demodex folliculorum (hair follicular mites) in females with and without rosacea. J Egypt Soc Parasitol. 2001;31(3):867-875. (Accessed online: https://pubmed.ncbi.nlm.nih.gov/11775112/)
12. Gao YY, Di Pascuale MA, Li W, et al. High prevalence of Demodex in eyelashes with cylindrical dandruff. Invest Ophthalmol Vis Sci. 2005;46(9):3089-3094.
13. Zhao YE, Wu LP, Hu L, et al. Association of blepharitis with Demodex: a meta-analysis. Ophthalmic Epidemiol. 2012;19(2):95-102.
14. Tarsus Collarette Prevalence Study, 2020.





