CASE PRESENTATION
A 17-year-old girl with a history of iris and ciliary body tumor presents with reduced vision and light sensitivity in her right eye. The patient’s ocular history is significant for iridocyclectomy performed on her right eye when she was a young child, with a tumor recurrence several years later that was treated with radiation. She is now cancer-free and was referred by her ocular oncologist for a cataract evaluation.
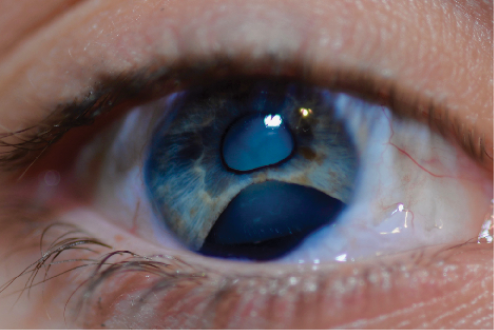
Figure 1. Clinical examination of the patient’s right eye showed an inferior iris defect and a white cataract.
(All images courtesy of Brandon D. Ayres, MD)
The patient’s visual acuity is count fingers in her right eye and 20/20 in her left. The pupil of the patient’s right eye is irregular, whereas the pupil of her left is normal with no afferent pupillary defect. A slit-lamp examination of the right eye shows mild scarring of the inferior conjunctiva and a clear cornea. A large inferior iris defect and a white cataract are evident (Figure 1). The lens equator is irregular in shape and visible through the iris defect. A slit-lamp examination of the patient’s left eye is essentially normal. B-scan ultrasonography of her right eye is normal, and a dilated fundus examination of her left is normal. The IOP is in normal range in both eyes.
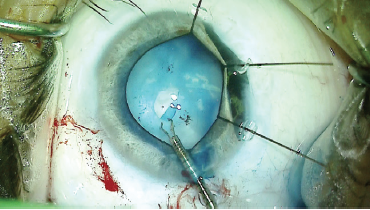
Figure 2. Iris hooks held the iris defect out of the surgical area while Dr. Ayres created a CCC with microforceps.
The patient has traveled with her family for the consultation, and she expresses interest in cataract removal and management of the light sensitivity or glare. How would you proceed?
—Case prepared by Brandon D. Ayres, MD

MARIE-JOSÉ TASSIGNON, MD, PhD, FEBO
Cataract formation was inevitable in the patient’s right eye, which is why some ophthalmologists have proposed performing cataract surgery prior to irradiation. The challenges associated with this approach are unpredictable eye growth and an eventual need for postoperative refractive correction by IOL exchange or corneal refractive laser treatment. When the bag-in-the-lens technique is used with a Bag-in-the-Lens IOL (type 89A, Morcher), IOL exchange can easily be accomplished. Obviously in this case, the preventive cataract surgery approach was not chosen.
The patient has a white cataract and an iridectomy of about 90º or a little more. My cataract surgery approach would be Bag-in-the-Lens IOL implantation. I would use trypan blue ophthalmic solution (VisionBlue, Dutch Ophthalmic USA) to facilitate the anterior continuous curvilinear capsulorhexis (CCC). I would color only within the Tassignon ring caliper (Morcher) so as not to affect the stiffness of the remaining capsule, which will already be quite stiff from irradiation.
Figure 1 does not show the iris dilated, but I presume dilation would be sufficient to allow cataract surgery. If not, I would place iris hooks but not an iris ring dilator, which could damage the remaining iris bridge and the intact sphincter. I would not expect the posterior CCC to be more difficult than in nonirradiated eyes.
I would perform iris repair as a second procedure so that I could better evaluate the options after the primary surgery. One approach would be suturing alone. Alternatively, a flexible silicone color-matched artificial iris (CustomFlex ArtificialIris, HumanOptics, US distributor VEO Ophthalmics) could be sutured with three stitches, one at the limbus (embedded in a Hoffman pocket) and one on each side of the iris rim.1

MITCHELL WEIKERT, MD
This case presents two main challenges: (1) removing a white, possibly intumescent cataract with 3 to 4 clock hours of zonular loss and (2) managing a large iris defect.
In cataract removal, I would expect pupil expansion to be necessary; with the large iridectomy, the pupil likely will not dilate fully or evenly. In this case, I would prefer to use iris retractors rather than a ring-based expansion device. I would place a dispersive OVD to tamponade vitreous in the area of zonular loss. Next, I would stain the capsule with trypan blue dye to facilitate visualization of the capsulorhexis. Initial needle aspiration might help decompress the lens and thus reduce the risk of a capsular tear or Argentinean flag sign. Use of a femtosecond laser to create the capsulotomy could also be considered, but this approach might prove difficult if the pupil did not dilate adequately and/or the location of the laser did not permit sterile docking.
Capsular hooks or an Ahmed Capsular Tension Segment (Morcher, US distributor FCI Ophthalmics) could be used to support the bag inferiorly during phacoemulsification. Given the patient’s age, I would expect the lens to be soft, which might allow its removal with aspiration alone. Additionally, I would make sure to inject OVD prior removal of irrigation. The strength of the remaining zonules should be normal, so a standard capsular tension ring (CTR) would probably provide adequate long-term support. If not, a sutured capsular tension segment could be considered, but the inferior scarred conjunctiva and scleral thinning could increase the complexity of this maneuver.
Although the iris defect is large, repair using McCannel sutures could be attempted. With small-gauge retina scissors, I would try to mobilize additional iris material via peripheral, paralimbal cuts near its insertion on each side. I would expect there to be a residual peripheral defect, but the repair would nevertheless help to establish a round, centered pupil and reduce postoperative glare. The CustomFlex ArtificialIris would be another option. The prosthesis, customized to match the patient’s iris color, could be inserted into the capsule after implantation of the CTR and IOL.

WHAT I DID: BRANDON D. AYRES, MD
I had an extensive discussion with the patient and her family about the risks and benefits of cataract surgery; the increased complexity, given the maturity of the cataract and her prior surgery; and the inability to predict how much vision she would recover. We also discussed the placement of a CustomFlex ArtificialIris, as part of an ongoing FDA study sponsored by Clinical Research Consultants, to see whether the device would reduce the glare and light sensitivity she was experiencing. After careful consideration, the patient and her family decided to proceed with cataract surgery and placement of an artificial iris.
My surgical plan was to remove the cataract and place a CTR and IOL. Provided the surgery to this point was uncomplicated, I would then place the artificial iris in the capsular bag. As with many complex cataract procedures, I knew it would be crucial to make a CCC because a defect in the capsulorhexis would prevent placement of the artificial iris in the capsular bag. I stained the capsule with trypan blue dye and used a 25-gauge needle to decompress the liquefied lenticular material to help prevent a tear-out of the capsulorhexis. With iris hooks, the pupil was dilated in the area of the iridocyclectomy, and microcapsulorhexis forceps were used in creation of the CCC (Figure 2). Next, a capsular retracting hook was placed in the area of zonulopathy to provide support during lens removal.
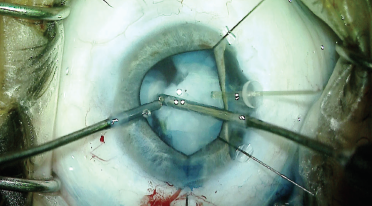
Figure 3. Capsular support was placed in the area of a known zonular defect. Dr. Ayres then removed the lens with bimanual irrigation and aspiration.
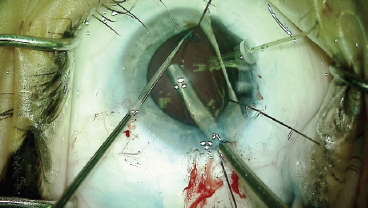
Figure 4. A CTR was placed in the capsular bag.
Because of the patient’s youth, I was able to remove the lenticular material with bimanual irrigation and aspiration (Figure 3), while taking care not to worsen the existing zonulopathy. Next, a CTR was placed to help support the equator of the capsular bag and prevent capsular contraction around the IOL and artificial iris (Figure 4). After filling the capsular bag with OVD, I measured the size of the bag with a microruler (Figure 5). A one-piece acrylic IOL was then placed in the bag; the targeted postoperative refraction was -0.50 D.
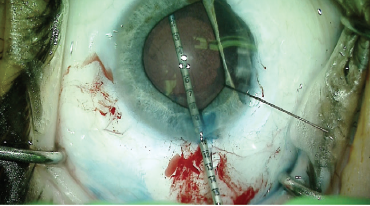
Figure 5. Using an intraocular ruler, Dr. Ayres measured the capsular bag to be approximately 10 mm.
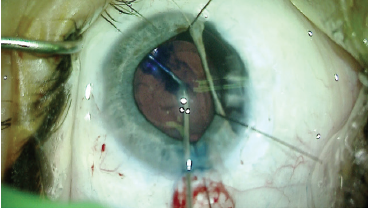
Figure 6. After implantation of the IOL, Dr. Ayres restained the capsular bag with trypan blue dye to improve visualization during placement of the CustomFlex ArtificialIris.
After IOL implantation, the capsular bag was restained with trypan blue dye to improve visualization for placement of the iris prosthesis (Figure 6). The silicone implant was trephined to 10 mm (as measured by the intraocular ruler) and placed in an insertion device. The artificial iris was delivered into the capsular bag and positioned using microforceps. I have found that, with careful manipulation, these prostheses can be unfolded and placed fully within the capsular bag (Figure 7).
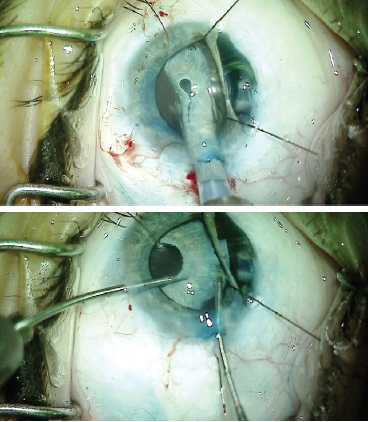
Figure 7. The iris prosthesis was placed in an inserter and partially delivered into the capsular bag (top). Dr. Ayres used microforceps to fully unfold the implant and place it in the capsular bag. The capsulorhexis must be visualized to ensure that the prosthesis is in the capsular bag (bottom).
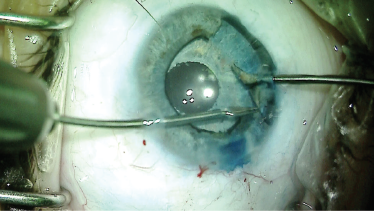
Figure 8. Dr. Ayres removed the iris remnant to keep it from interfering with the new prosthetic pupil.
Once the iris prosthesis was secure in the capsular bag, I removed the nonfunctioning iris strand to make sure it would not bisect the artificial pupil (Figure 8). At the conclusion of the case, the iris retractors and OVD were removed from the anterior chamber, and the incisions were hydrated (Figure 9).
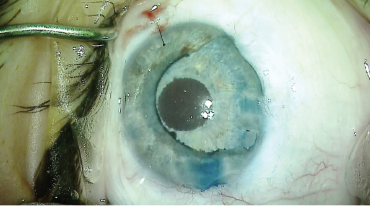
Figure 9. At the end of the case, all incisions were sealed and the OVD was removed. The blue stain of the capsular bag overlying the iris prosthesis confirmed its placement in the bag.

Figure 10. Postoperative appearance of the patient’s right eye. The left eye underwent no surgery.
The patient tolerated surgery very well, and her postoperative course was uneventful. On postoperative day 1, UCVA had returned to 20/60, and it improved to 20/40 by week 1. The patient reported some light sensitivity but noted a significant improvement from preoperative (Figure 10).
1. Magnus J, Trau R, Mathysen DGP, Tassignon MJ. Safety of an artificial iris in a phakic eye. J Cataract Refract Surg. 2012;38(6):1097-1100.




