Tracking Outcomes After Laser Vision Correction
Erica T. Liu, MD

Tracking outcomes is important for optimizing outcomes with any surgical procedure. Our initial SMILE nomogram was created with Datagraph-med version 5.70 (Datagraph-med) after we had collected data on 60 eyes using a service provided by Carl Zeiss Meditec. We eventually purchased our own software license to take advantage of robust data analysis features and make faster adjustments as more data were acquired.
Our clinic typically examines patients 2 to 3 days, 1 month, and 6 to 12 months after they undergo SMILE. We check their UCVA at distance and near at all visits and their BCVA at 1 month and 6 to 12 months.
We enter each patient’s age, starting refraction, BCVA, planned treatment, target and follow-up refraction, and postoperative UCVA and BCVA into Datagraph-med. The software then produces a nomogram look-up table and numerous graphs. When additional data such as keratometry readings, optical zone, pachymetry reading, and pupil size are entered, it is possible to make more specific nomogram adjustments and to track results more closely.
We have achieved refractive results within ±0.50 D of the target in 100% of SMILE patients since implementing our nomogram, compared to 91% previously. More staff time is required to gather and enter data, but the effort is rewarded with lower enhancement rates, greater patient satisfaction, and confident staff.
Power in the Palm of Your Hand
Mohammed Muhtaseb, FRCOphth

The cataract and lens exchange analysis and register logbook (CLEARlog) is a product of my strong desire to analyze my cataract surgery and refractive lens exchange outcomes in terms of both objective and subjective parameters. The software, which can be accessed via an app or a website, is easy to use and efficient so that it fits into surgeons’ busy schedules.1
ASSESSING SURGICAL SAFETY
Surgeons often compare their refractive outcomes and their rate of posterior capsular rupture with those of peers and national and international standards for benchmarking purposes (Figures 1 and 2). Surgeons may also use their surgical data to meet regulatory requirements such as the annual appraisal in the United Kingdom and for patient counseling, informed consent that can be customized to both the patient and the surgeon, and academic and marketing presentations.
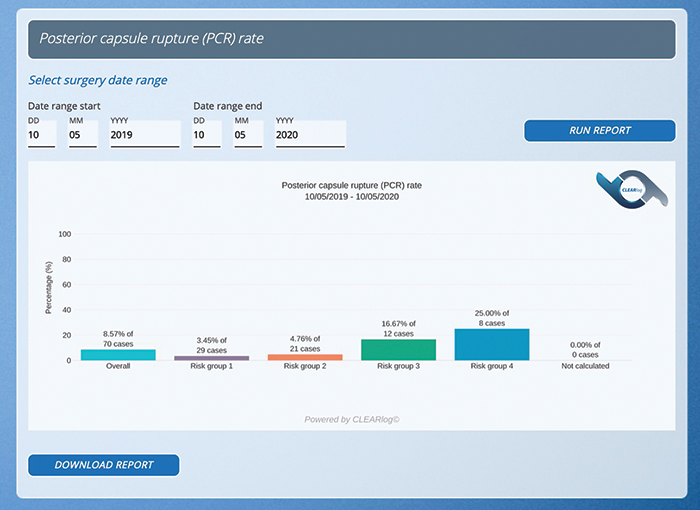
Figure 1. Risk stratification of posterior capsular rupture rate.
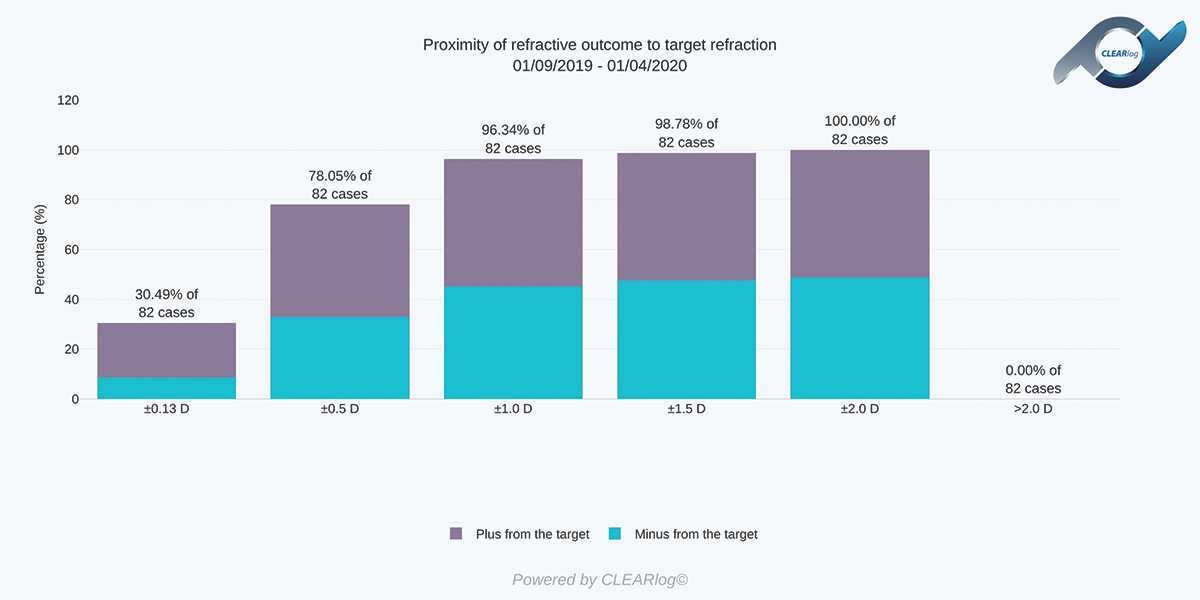
Figure 2. Comparison of actual refractive outcomes to the preoperative target. The first column fulfils the requirement for publication in many peer-reviewed journals.
I use reports from CLEARlog to help me prepare a risk stratification of my case mix, provide customized options to each patient, monitor my refractive outcomes, and guide modifications to my practice to drive improvements. I can enter data into the software program while I am in the clinic or the OR, or one of my team members can enter the data in the office. I often generate reports on my smartphone so that I can check my most recent performance data.
IMPROVING PATIENT OUTCOMES
CLEARlog helps me analyze or evaluate my overall outcomes by specific parameters such as the biometry formula used or the IOL chosen. I can also factor in patient satisfaction. This information can guide changes I make to improve my outcomes. For example, a better understanding of the rate of spectacle independence at distance, intermediate, and near that my patients are achieving with various IOLs helps me to improve patient counselling and my preoperative recommendations (Figures 3 and 4).
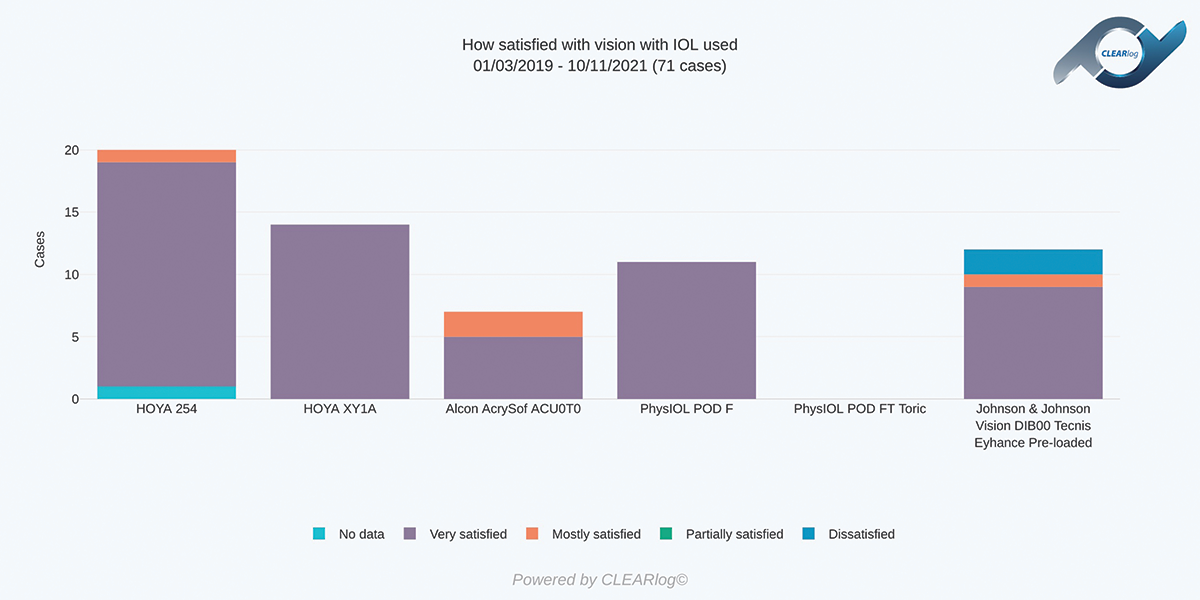
Figure 3. Patient satisfaction with vision is categorized by the IOL used.
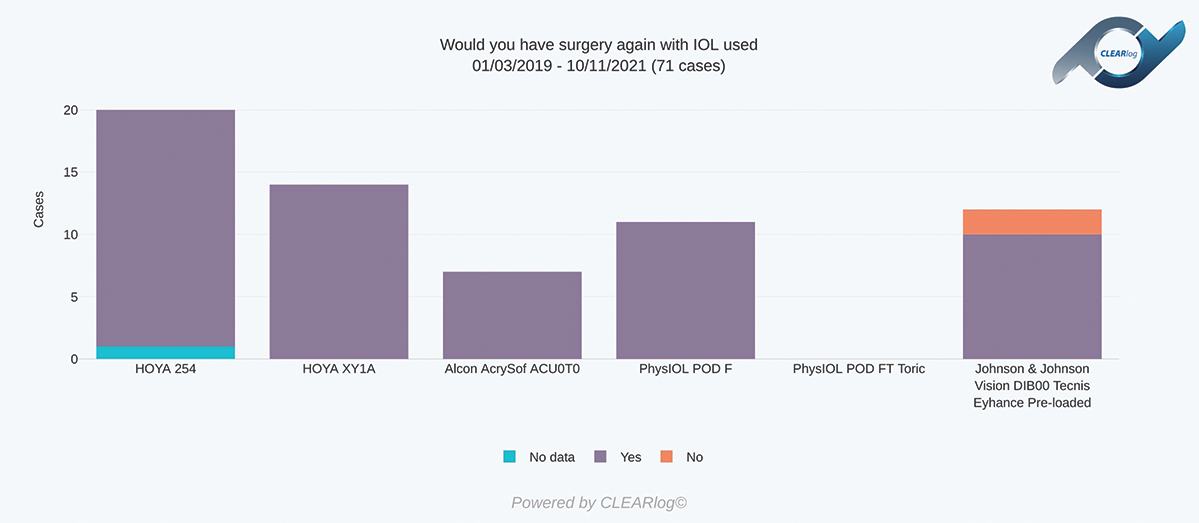
Figure 4. Would patients undergo the surgery again or recommend it to a friend? Responses are categorized by the IOL used.
USING REAL PRACTICE DATA TO OPTIMIZE PATIENT COUNSELING
By viewing outcomes over time, I can see how patients’ vision changes after surgery. This information allows me to refine my recommendations based on objective and patient-reported outcomes. It also allows me to counsel patients with confidence, both during the initial consultation and on early follow-up calls.
I can view results with various IOLs on a single graph or several outcome parameters with a single IOL on the same graph (Figures 5 and 6).
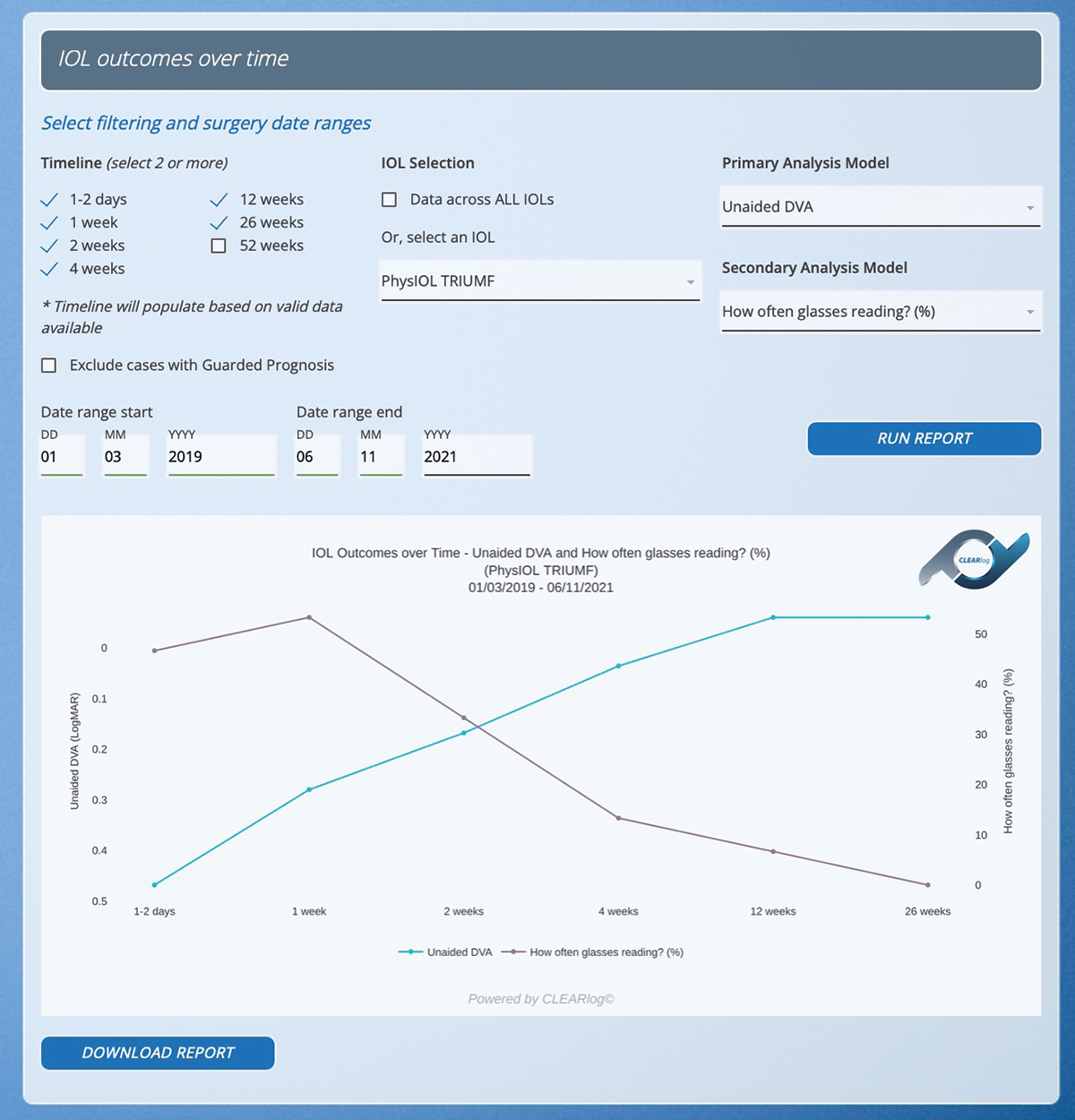
Figure 5. A double y-axis report shows patients’ uncorrected distance visual acuity and their need for reading glasses over time.
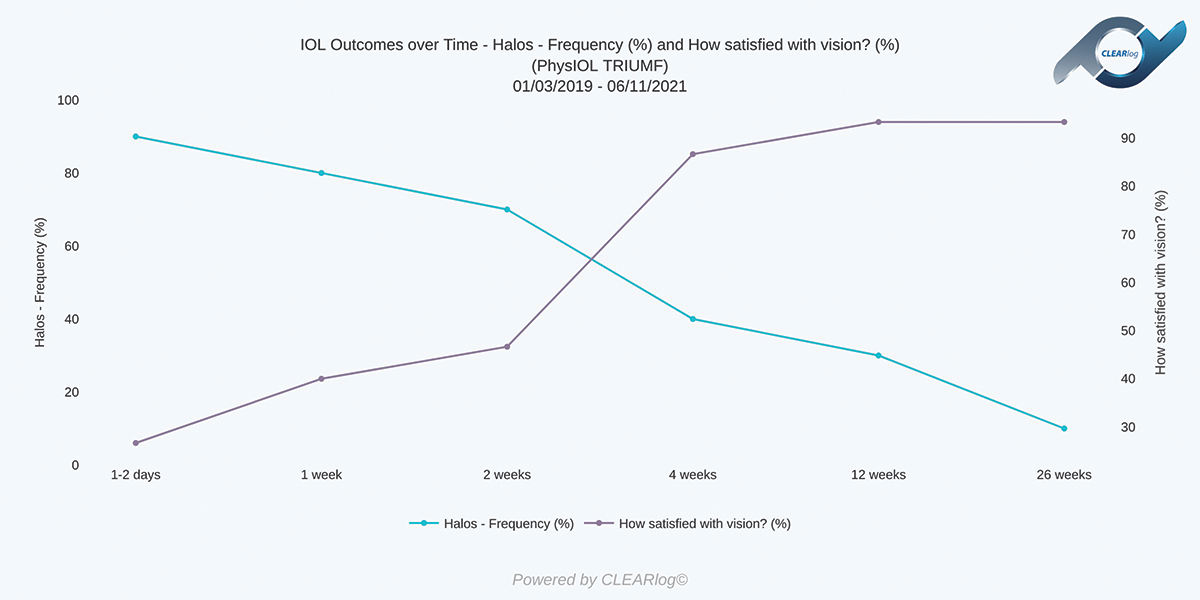
Figure 6. The frequency with which patients see halos is contrasted with their satisfaction with their outcomes over time.
CONCLUSION
Interested parties can test out the software for 1 week by accessing the demo account, which contains fictitious data. Users may add new records, edit fictitious and new records, and generate reports. More information may be obtained at clearlogportal.com.
1. Muhtaseb M. CLEARlog: a new electronic registry and outcomes analysis software for cataract and refractive lens exchange. Poster presented at: 38th Congress of the ESCRS; October 2–4, 2020; Amsterdam, Netherlands.
Building a Wholly Integrated and Customized Platform
Filomena Ribeiro, MD, PhD, FEBO

Any system for tracking outcomes that a practice uses must be tied into surgical workflow—from preoperative evaluation through final result. The platform should also be customized to suit the individual practice. My hospital is in the process of integrating preoperative and biometric data from all our diagnostic devices with patient records so that everything is in one place and can be accessed remotely by surgeons and staff.
This is a lot to manage. The system we build must be compatible with our surgical suite of tools and the software we use to manage patient information. The goal is to track outcomes and improve upon them (eg, eliminating transcription errors that can occur during cataract surgery planning). Implantation of the incorrect IOL and surgery on the wrong eye are the most common errors in ophthalmology.1
An integrated platform can increase procedural accuracy. We are also looking to connect the system with a patient-facing app so that patients can report subjective outcomes and these data can be incorporated into our analyses.
Several platforms on the market integrate data, and many are companions to specific surgical devices. We are working on a universal system that will allow us to import information from all devices and patient software platforms regardless of manufacturer. The hope is that a customized system will allow us to determine the formulas that work best for our specific population’s average biometric measurements, our surgical methods, and the IOLs that we use. In addition to optimizing IOL power calculations, we wish to study surgically induced astigmatism and build our own nomograms to further improve our results.
The software, in turn, should make IOL selection easier. AI can quickly correlate data and identify measurement errors. Ultimately, this technology should help us to personalize IOL power calculations and profiles and customize our offerings.
What really matters to our patients is performing their activities of daily living without limitations. Surgical solutions are not universal; they must be customized. By tracking and refining outcomes, engaging patients in decision-making with questionnaires and vision simulators, and setting realistic expectations, we hope to maximize patient satisfaction.
1. Steeples LR, Hingorani M, Flanagan D, Kelly SP. Wrong intraocular lens events—what lessons have we learned? A review of incidents reported to the National Reporting and Learning System: 2010–2014 versus 2003–2010. Eye (Lond). 2016;30(8):1049-1055.
Long-Term Tracking has the Potential to Improve Outcomes
Thilo Schimitzek, MD, FEBOS-CR

To improve care, I believe it is important to track patient satisfaction and listen to their feedback. While practicing in the United Kingdom, it was part of my standard processes to undertake quality audits of patients. Similarly, in my current practice in Germany, I track and respond to patient-reported outcomes. This effort helps me to measure patient satisfaction and identify areas to improve.
GATHERING FEEDBACK
I began using the RayPro digital platform (Rayner) about a year ago to track and report patient feedback and other data points from individuals who received Rayner IOLs. Data are tracked for a period of 3 years after surgery. There is a simple registration process for clinical teams and an online questionnaire interface for patients. Participation is free for patients, and it gives them an opportunity to rate their experiences over time. I hope to use these real-time data to gain a better perspective on the full patient experience—from first contact through postoperative follow-up.
Previously, my practice depended on the Quality Assurance System, AQS1. This mail-in questionnaire tracks patient feedback on ambulatory surgical experiences based on 14 clinical indicators.
I believe in the value of patient-reported outcomes that focus on their satisfaction with aspects of their surgical experience.
Example No. 1: Increase support. Patient feedback provided through the AQS1 identified an opportunity for my practice to help patients feel supported throughout their surgical experience by having a staff member escort them from the OR and ensure that they had transportation home.
Example No. 2: Track and share complication rates. We have found that tracking postoperative complication rates over time and sharing this information as appropriate can reassure to patients. Being transparent about complication rates with them enhances the trust in the relationship between the patient and the surgeon. Patients feel safer about the procedure when they know the risks of surgery are minimal (Figures 7 and 8).
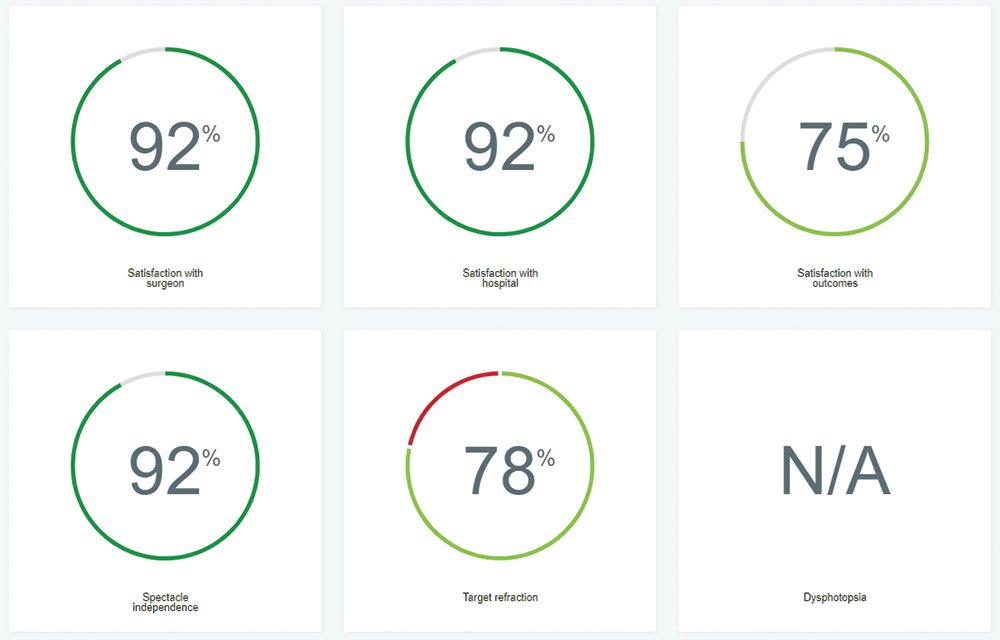
Figure 7. RayPro data overview.
Figures 7–11 courtesy of Thilo Schimitzek, MD, FEBOS-CR
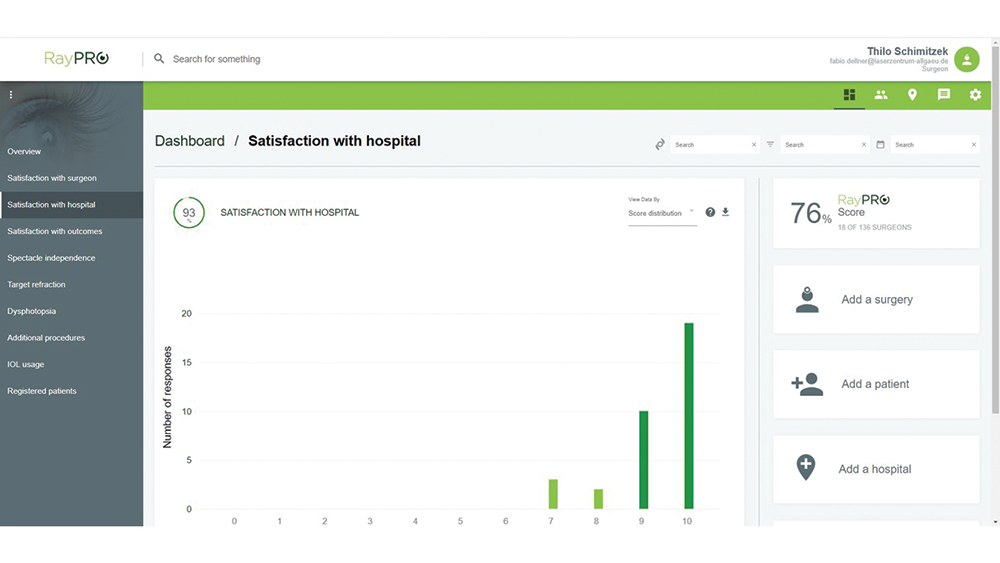
Figure 8. RayPro dashboard data.
ADOPTING A NEW TOOL
RayPro is a relatively new online patient-engagement tool, and it may take our practice some time to encourage more people to use it. Approximately 50% of our patients responded to the AQS1 questionnaire, and about 25% have used the RayPro platform since we implemented it a year ago. It could be that some patients do not participate because they consider providing feedback to be a hassle, and others may not be technologically savvy. I hope that, in the future, additional options for completing the questionnaires will help to improve participation. Currently, the RayPro platform sends five questionnaires over the course of 3 years. Each questionnaire consists of no more than six questions.
Tracking data on 3-year outcomes is valuable. Otherwise, the only way to know that patients are satisfied is when they refer others to our practice. The RayPro can also help us evaluate how patient satisfaction changes over time (Figures 9 and 10). This area is of particular interest with multifocal IOLs, for example, because progressive improvement is to be expected in the months after their implantation. Additionally, collected data may allow us to evaluate patient satisfaction with various lens types (Figure 11) and thus inform the patient selection process in the future.
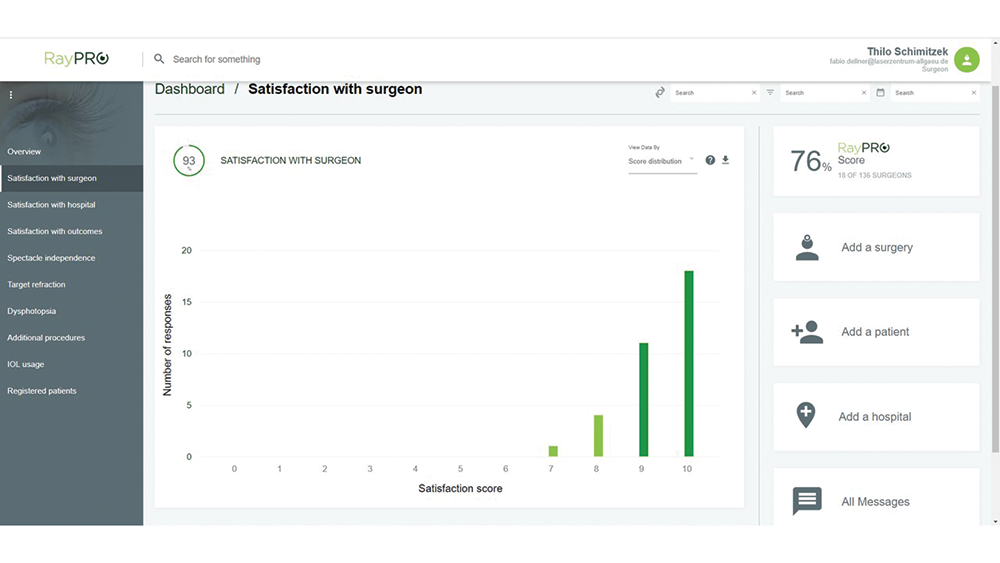
Figure 9. Patient satisfaction with the hospital.
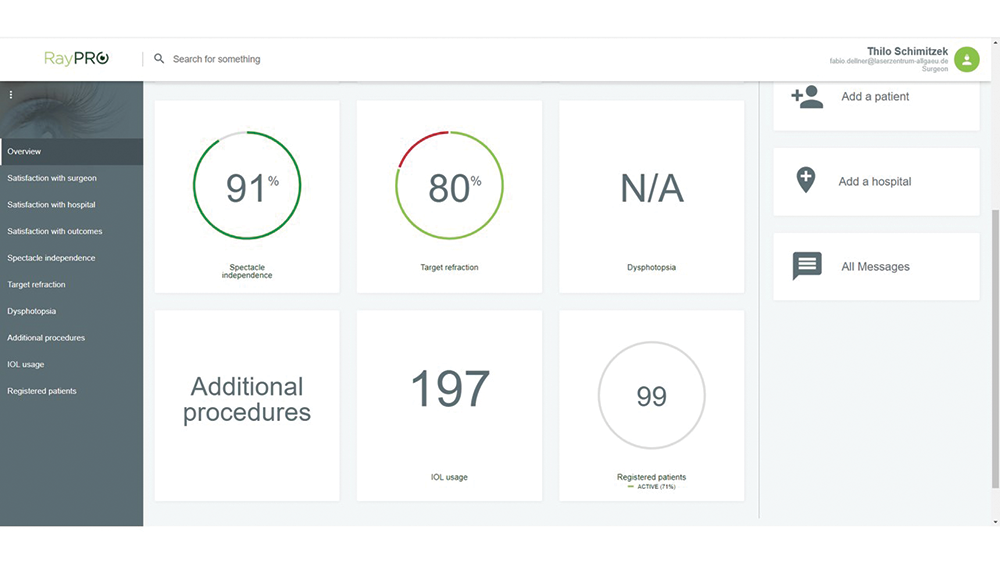
Figure 10. Patient satisfaction with the surgeon.
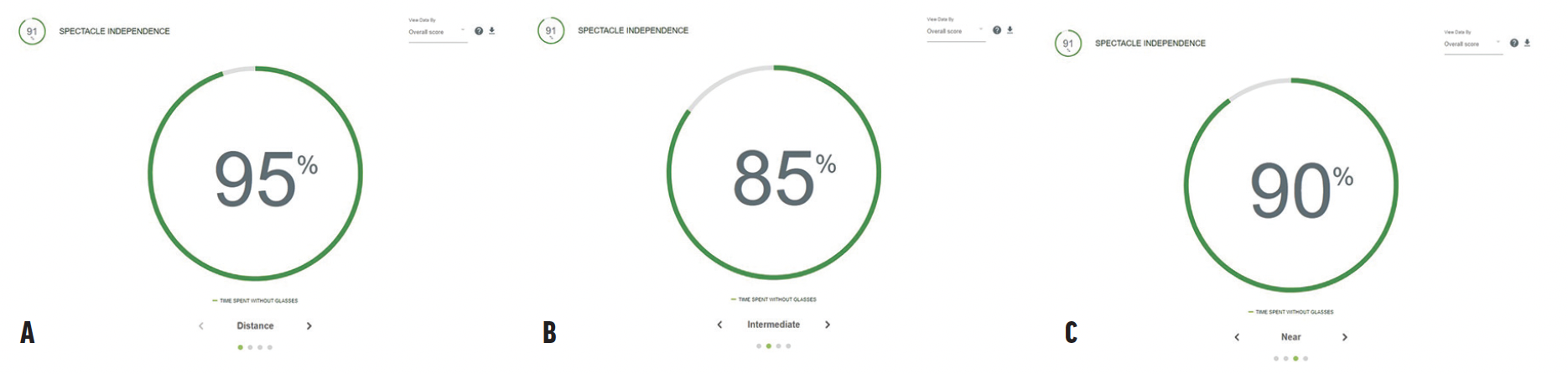
Figure 11. Spectacle independence at distance (A), intermediate (B), and near (C).
Tracking Refractive Results
Harvey S. Uy, MD

Despite myriad technological advances, the refractive accuracy of cataract surgery is not always what patients and surgeons could wish. Tracking refractive results, adjusting IOL constants, and accounting for surgically induced astigmatism can help practitioners improve their outcomes. Better still, in my experience, is to use a single digital platform for all aspects of cataract surgery workflow—biometry, IOL planning and ordering, surgical guidance, outcomes tracking, and fine-tuning of IOL constants.
METHODS OF OUTCOMES ANALYSIS
Personalized IOL constants. For most surgeons, using the latest IOL constants derived from the pooled data of many optical biometers is the simplest method of achieving good outcomes.1 Surgeons who wish to personalize their IOL constants can record their clinical data (ie, axial length, phakic anterior chamber depth, keratometry, postoperative visual acuity, manifest refraction, target and calculated spherical equivalent) for each specific IOL model in a spreadsheet and transmit it to the website of either Wolfgang Haigis, PhD, or Warren E. Hill, MD, to have an individualized IOL constant calculated. Data from at least 225 eyes are needed to maximize results. This process entails a significant amount of effort, including data extraction from medical records and biometry machines followed by encoding into the spreadsheet.
Digital software platforms. Fortunately, digital software platforms such as the ORA System (Alcon), EyeSuite on the Lenstar (Haag-Streit), and Veracity Surgical (Carl Zeiss Meditec) can streamline cataract surgery workflow and help to fine-tune IOL selection. The Zeiss EQ Workplace (Carl Zeiss Meditec) has greatly improved productivity and efficiency at my practice by allowing IOL planning and ordering on a single workstation. Patients’ clinical data and optical biometry measurements with the IOLMaster 700 (Carl Zeiss Meditec) are imported and integrated into a single planning page. The software database can be prepopulated with the surgeon’s surgically induced astigmatism, preferred IOLs, and updated IOL constants. The preferred IOL is selected, and the system then generates a purchase order. The EQ Workplace also sends data to Callisto eye (Carl Zeiss Meditec), which guides the capsulorhexis, toric IOL alignment, and creation of relaxing incisions. Finally, postoperative data may be entered into the software to generate a database for IOL constant customization.
1. Aristodemou P, Knox Cartwright NE, Sparrow JM, Johnston RL. Intraocular lens formula constant optimization and partial coherence interferometry biometry: refractive outcomes in 8108 eyes after cataract surgery. J Cataract Refract Surg. 2011;37(1):50-62.