Dr. Wong demonstrates a multitude of problems encountered in an eye with zonular dialysis and shares his solutions.
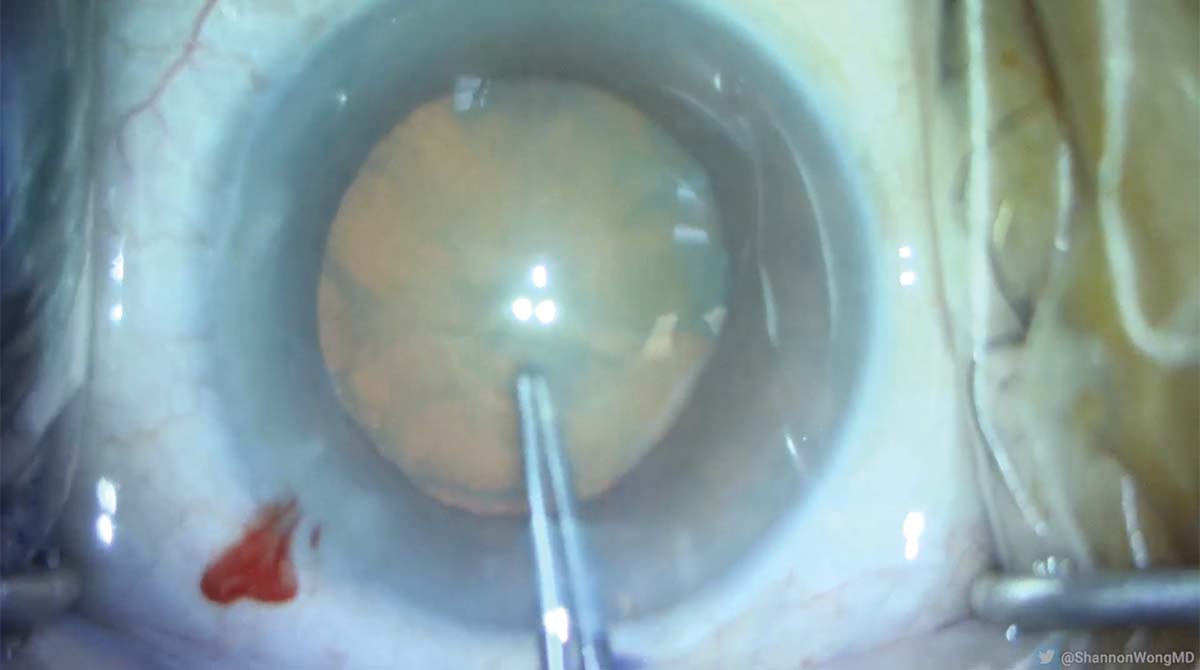
1. Routine cataract surgery with planned placement of a Synergy IOL (Johnson & Johnson Vision) begins. The patient does not speak or understand English. The capsulorhexis is completed safely using Utrata forceps, and hydrodissection is performed.

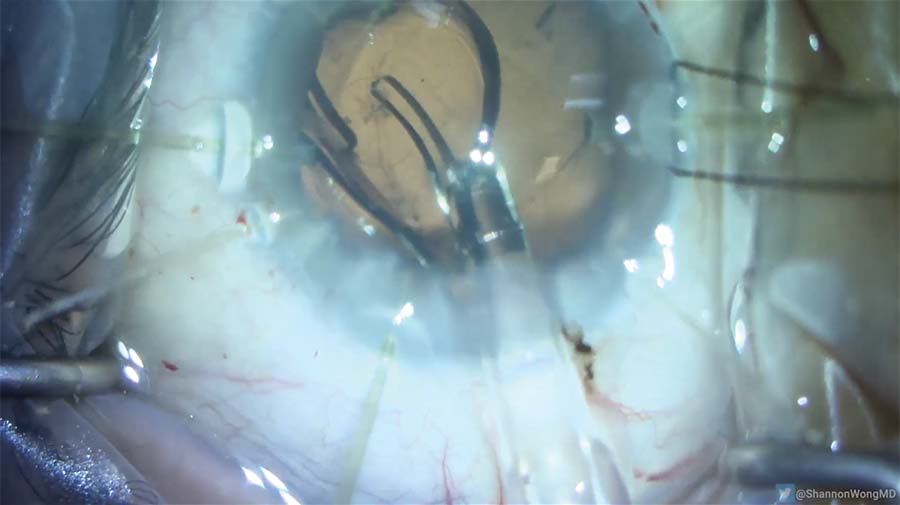
2. As the phaco needle is inserted, the iris prolapses into the needle.

3. A viscoelastic cannula is used to sweep the iris. An OVD is then infused between the phaco needle and the iris to allow safe passage of the phaco needle into the eye to clear the iris.
4. The lens is cracked into two hemi-nuclei, and each hemi-nucleus is then chopped into quadrants.
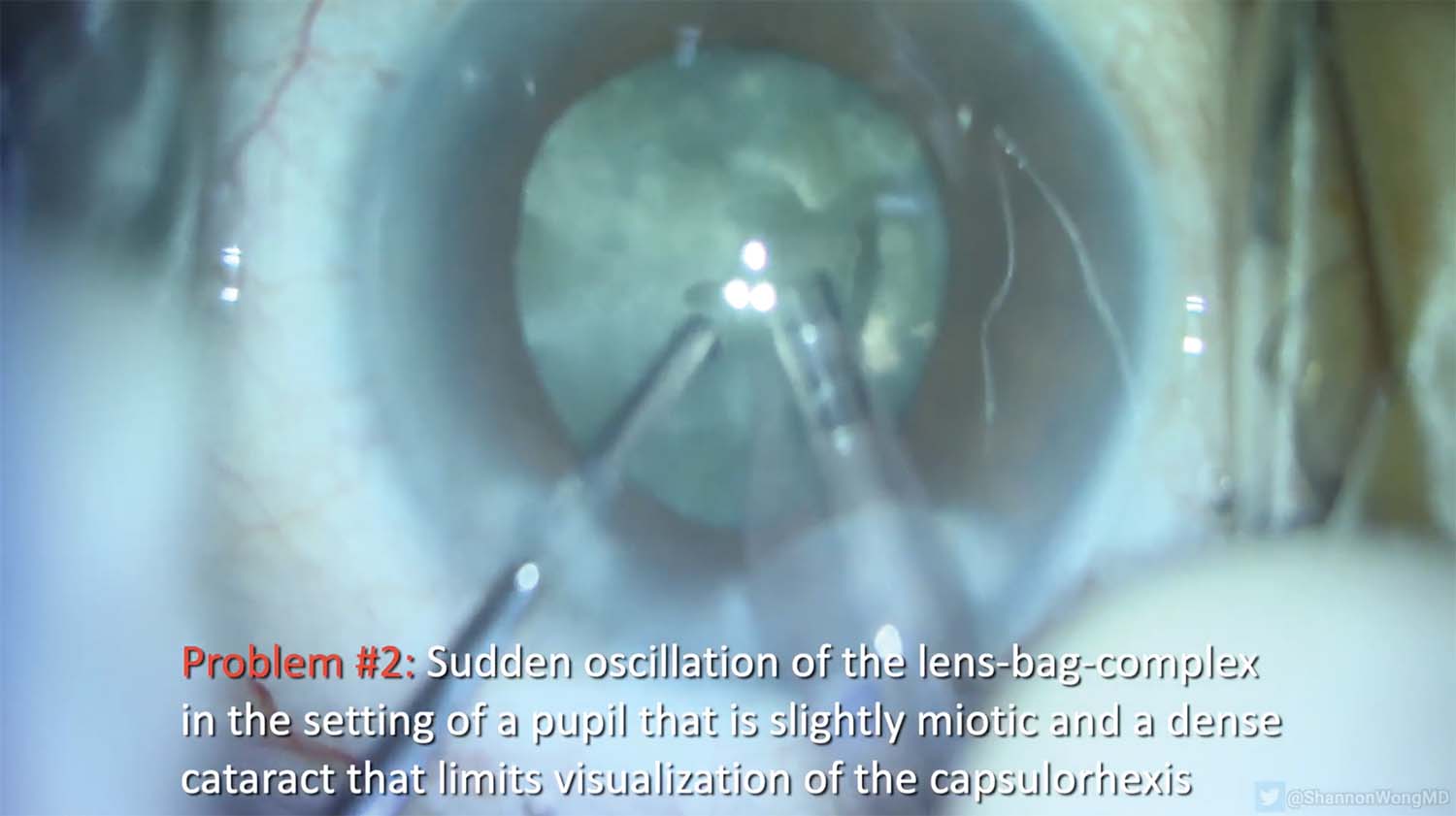
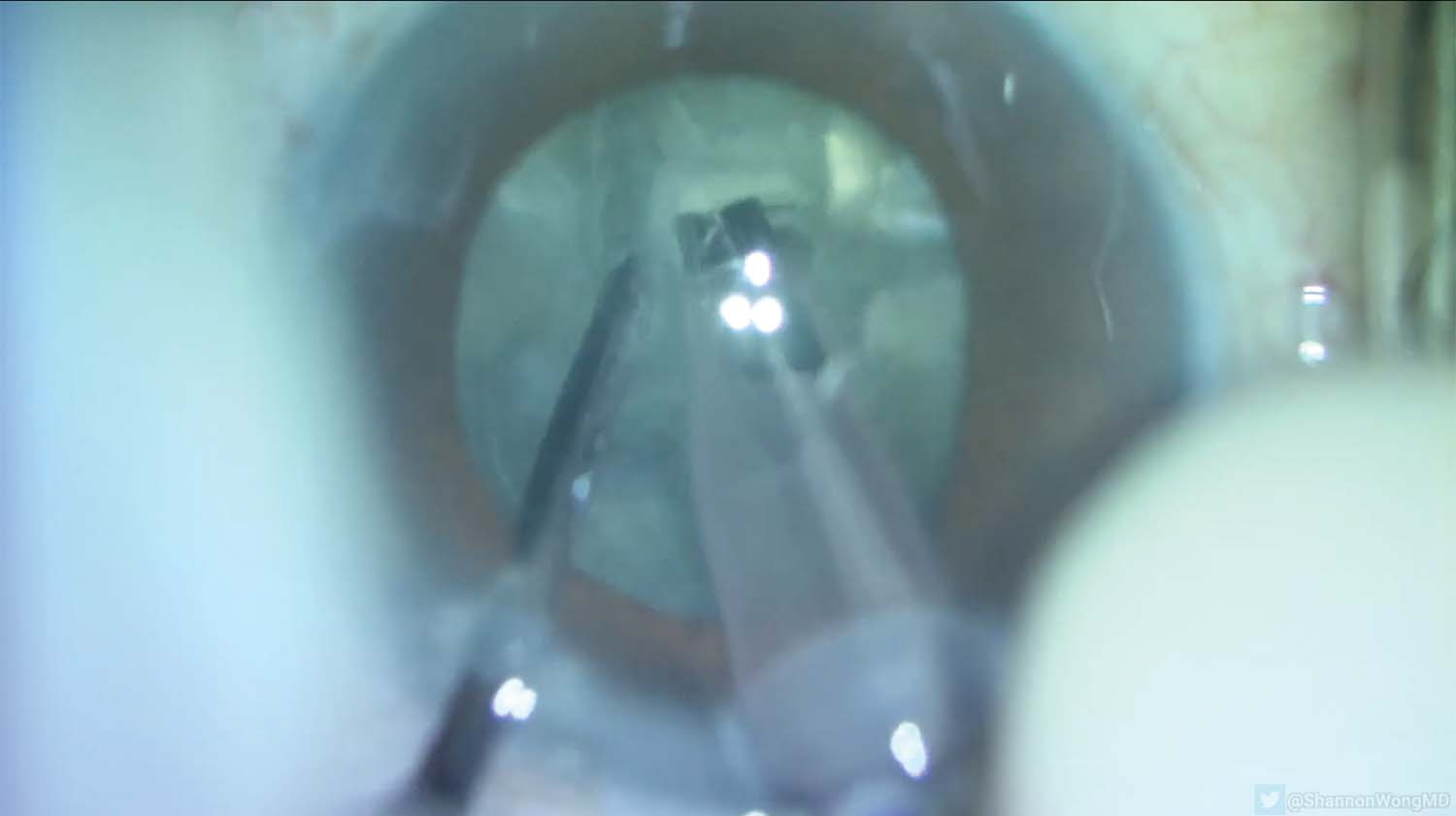
5. Vacuum is increased to remove the first quadrant, causing sudden (and abnormal) oscillation of the lens-bag complex.

6. Before proceeding with surgery, the situation is assessed.

7. More OVD is infused into the eye before the phaco needle is removed.
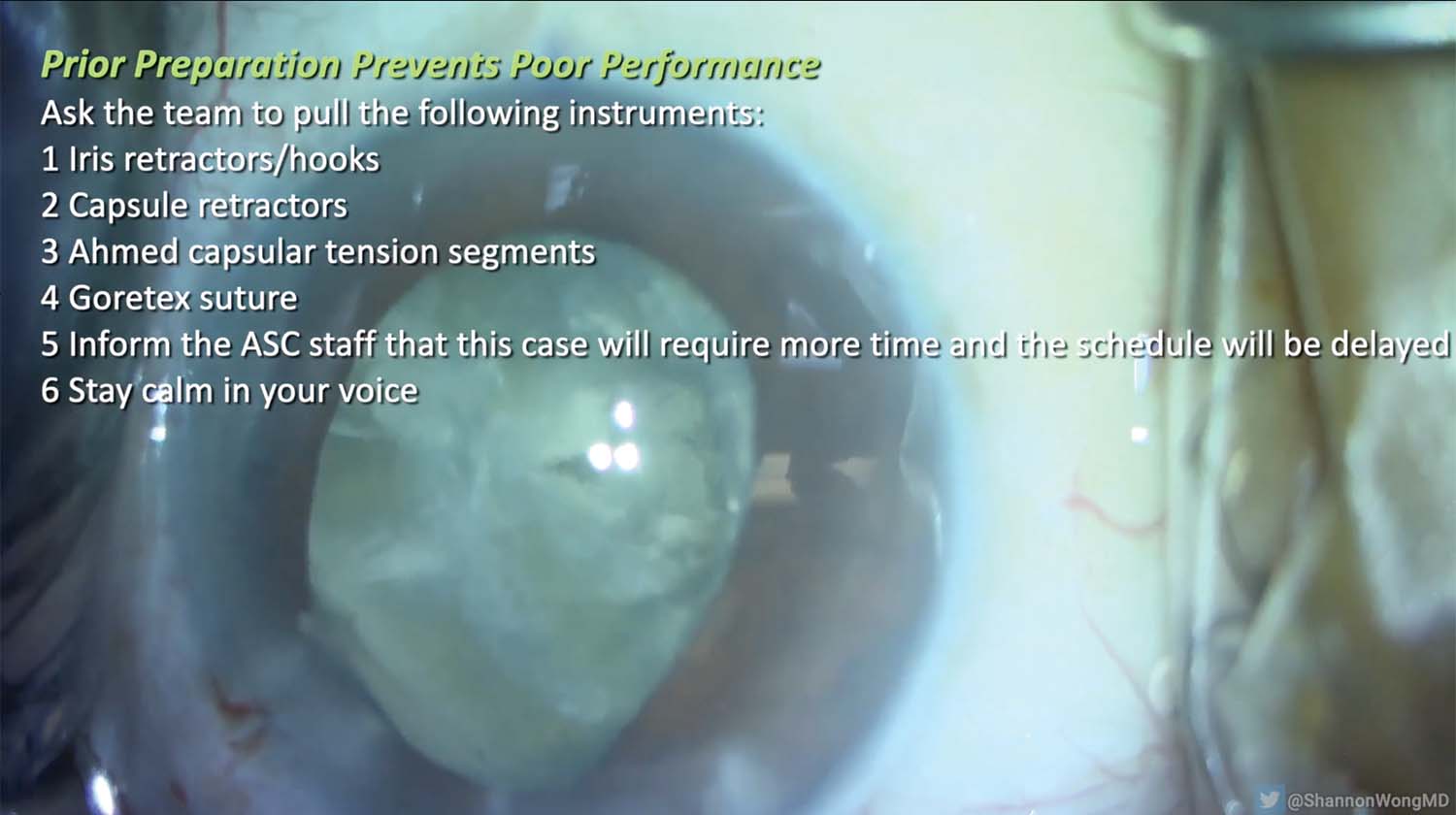
8. The pupil is relatively miotic. The team prepares the following instruments: iris and capsule retractors, Ahmed Segments (Morcher), and PTFE sutures. The staff is informed that the case will require more time than usual and the remaining day’s schedule will be delayed.

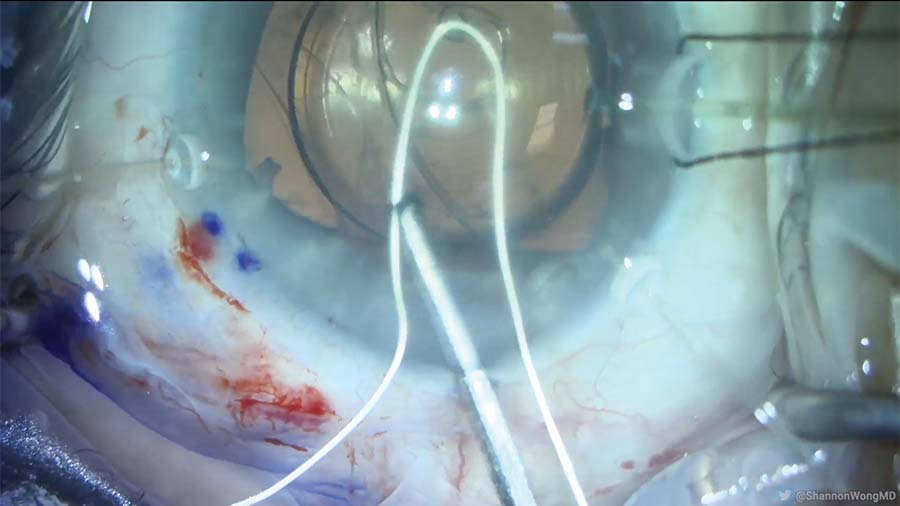
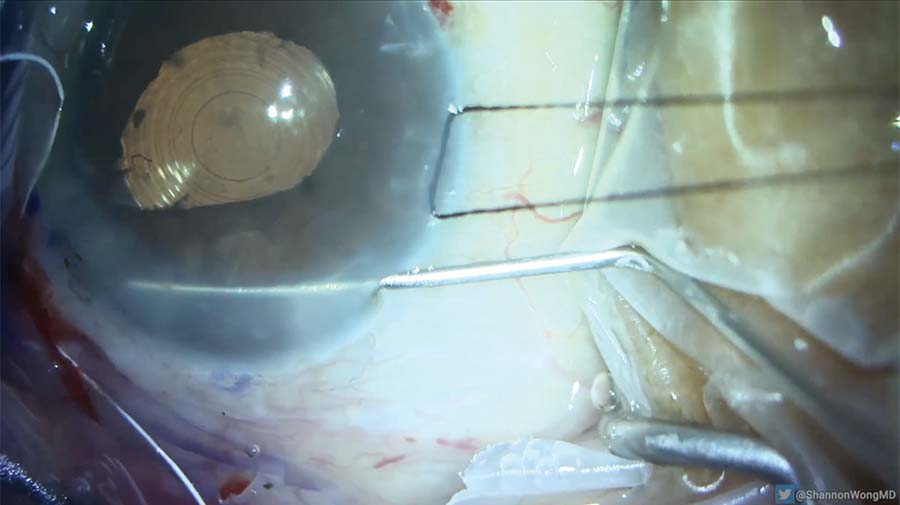
9. Iris retractors are inserted to improve visualization.
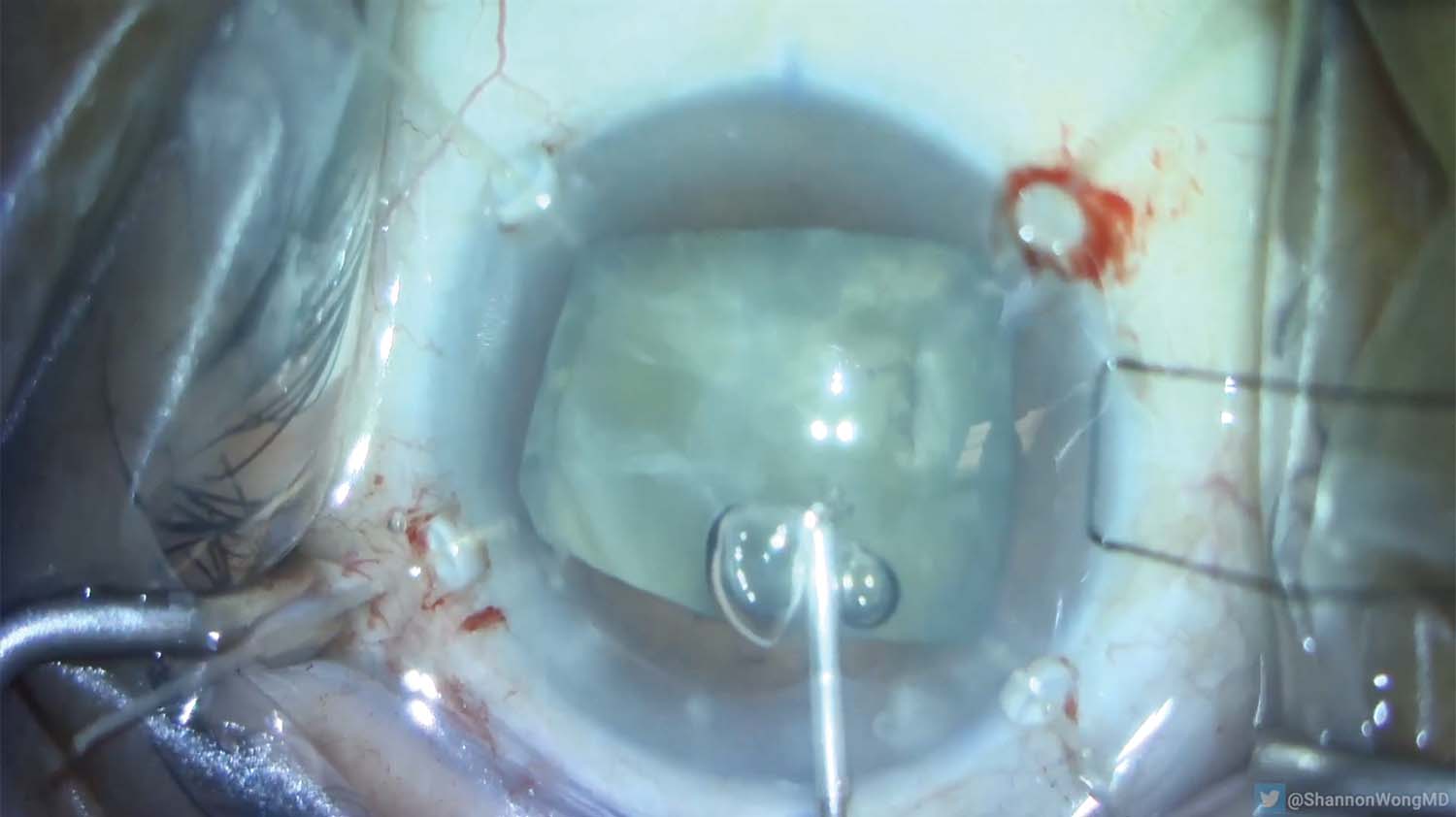
10. The patient looks down and to the left. The globe is fixated with a 7-0 silk suture because the patient cannot understand English to follow instructions to redirect her gaze. The suture needle is passed through the peripheral cornea and through the surgical drape. This maneuver positions the eye for surgery to proceed safely.
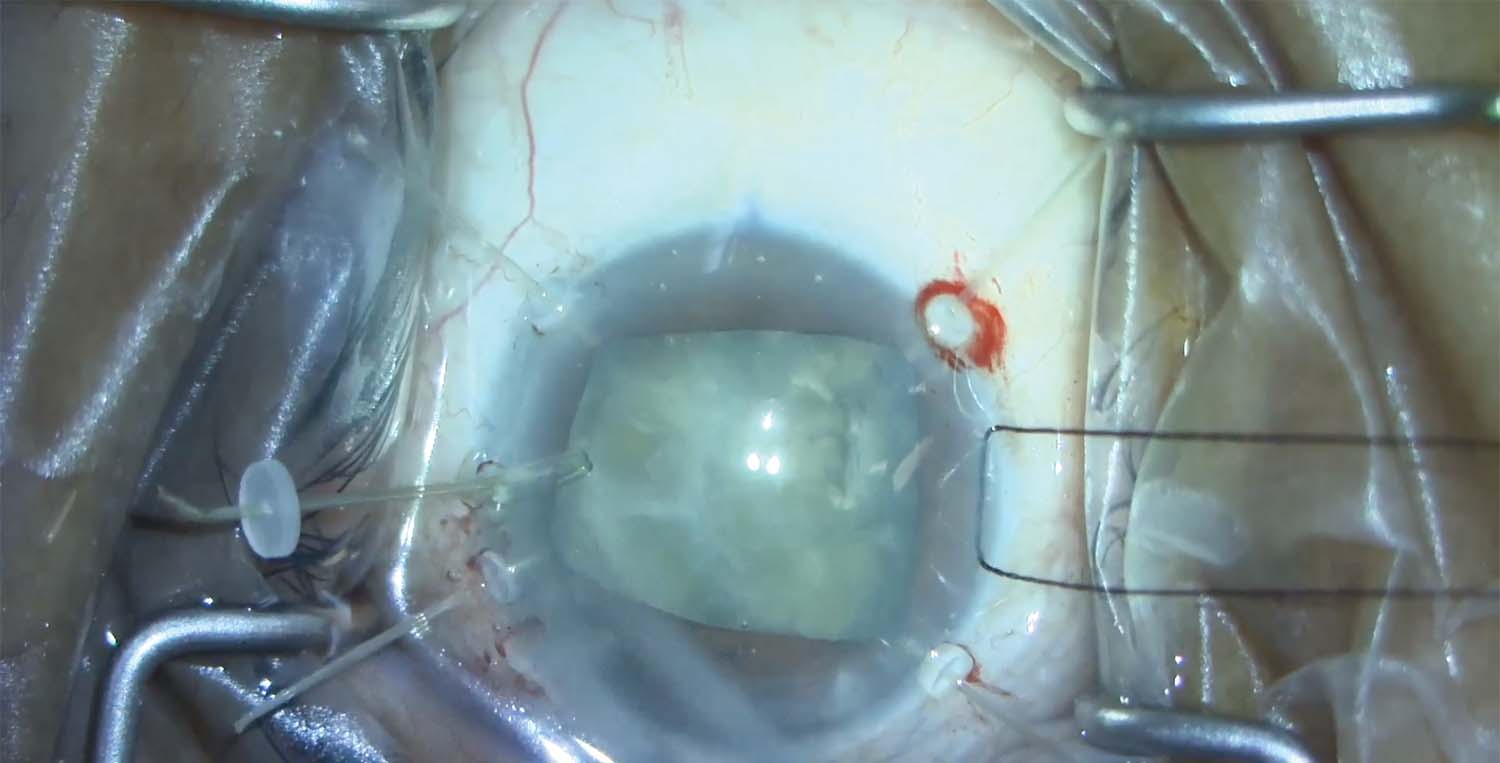
11. Four capsule retractors are placed to stabilize the lens-bag complex in the presence of zonular dialysis at the 9 clock position.
12. The cataract is removed. Routine irrigation and aspiration of the residual lens cortex begin.
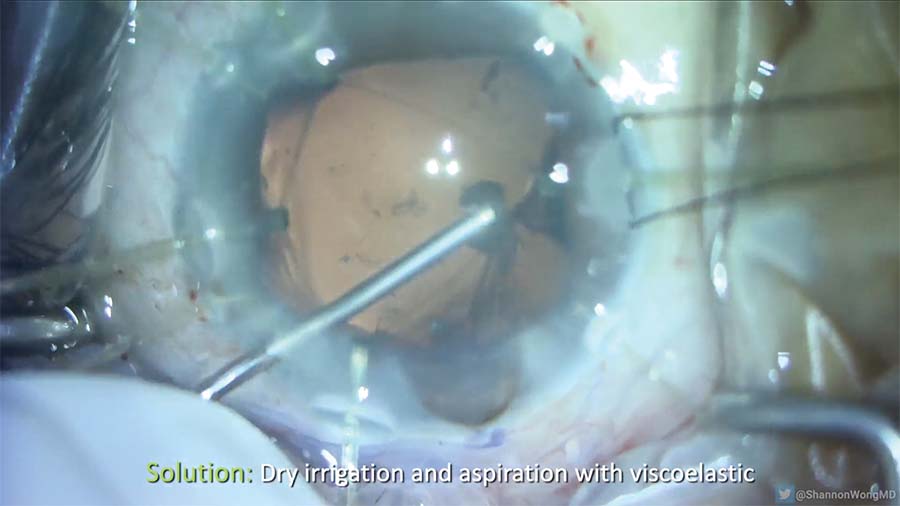
13. The capsular bag is under tension. OVD is injected under a dry I/A technique to safely remove the subincisional cortex and avoid extension of the anterior capsule.
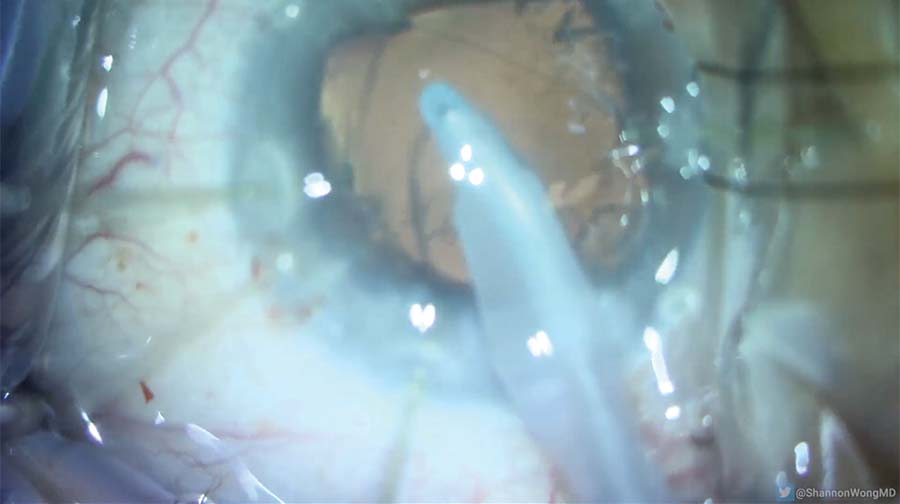
14. The iris prolapses. An additional amount of OVD is injected into the capsular bag, the iris is moved into a normal position, and the IOL is implanted.

15. The capsule retractors are removed. A zonular dialysis of 3 to 4 clock hours is noted from the 6 to 10 clock positions.
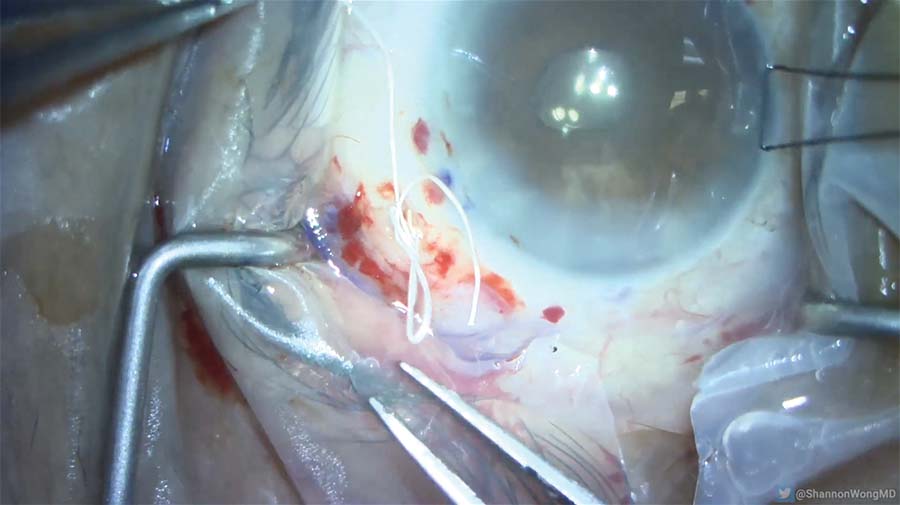
16. An Ahmed Segment is placed in the capsular bag and secured to the sclera 2 mm posterior to the limbus.
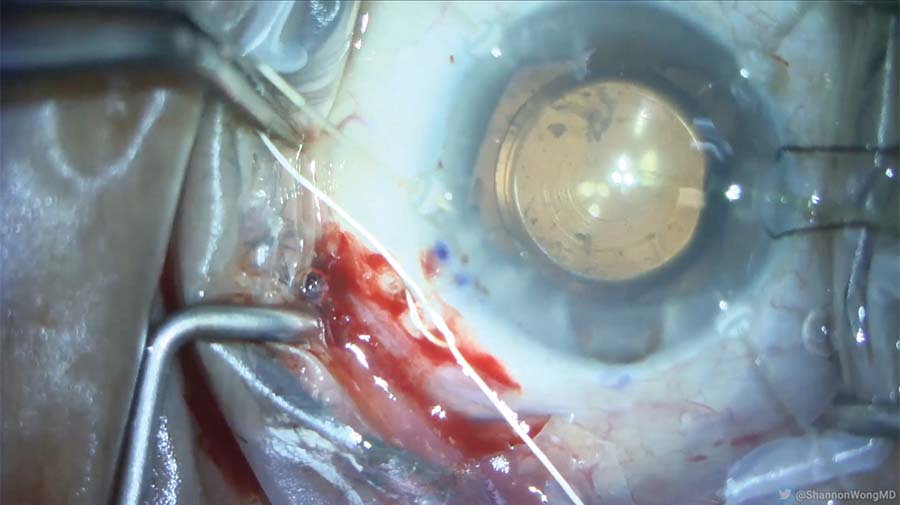
17. The position of the lens is titrated using a slipknot in the PTFE suture, the last capsule retractor is removed, and irrigation and aspiration are performed.
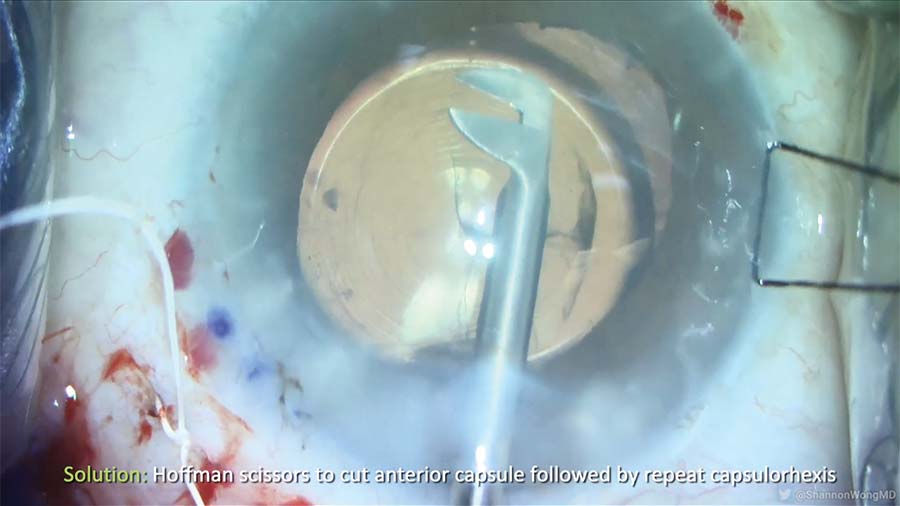
18. At this point, it is noticed that the anterior capsule overlaps the optic of the lens. Hoffman scissors are used to nick the anterior capsule, and the anterior capsular opening is widened with forceps.
19. Fibrous material is noted near the I/A port, underneath the iris at the 10 clock position. Carbachol intraocular solution is injected, and a cyclodialysis spatula is used to resolve the iris prolapse around one of the secondary incisions. Vitreous prolapse through that incision is resolved with anterior vitrectomy.
20. At the end of the case, the lens is centered by titrating the suture tension, and the knot is locked and buried in the sclera.





