Dr. Bettis walks through the steps he took during cataract surgery on an eye with a preexisting posterior capsular opening to ensure the patient achieved full visual recovery.

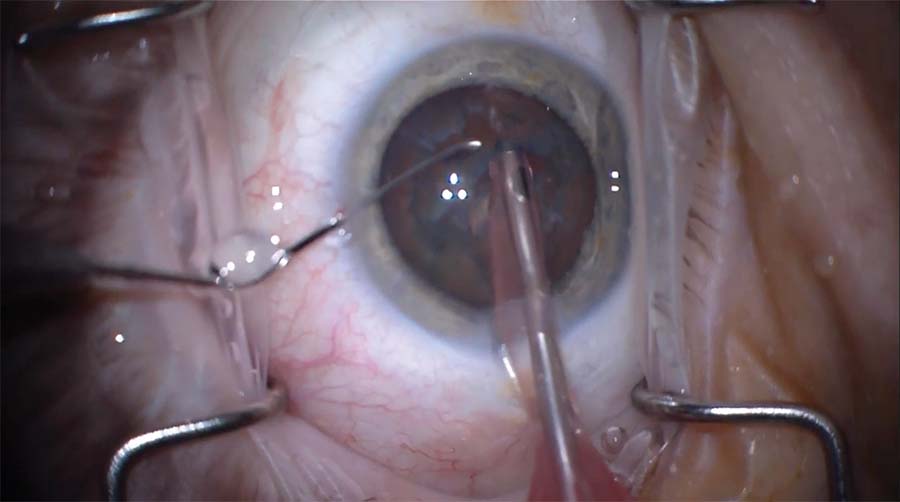
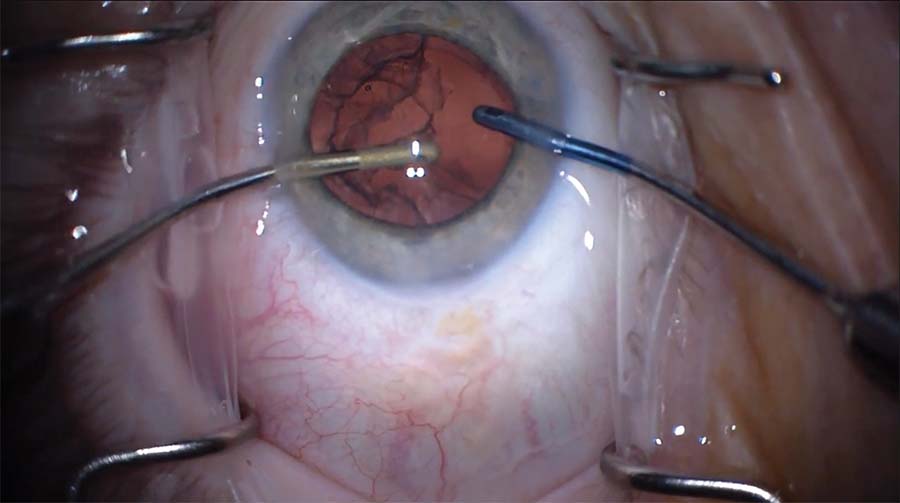
1. The patient presents following the rapid onset of a cataract after pars plana vitrectomy. A careful surgical technique is planned to avoid disturbing a potential preexisting posterior capsular opening. First, the capsulorhexis is made large enough to facilitate optic capture of a three-piece IOL in the sulcus if needed.
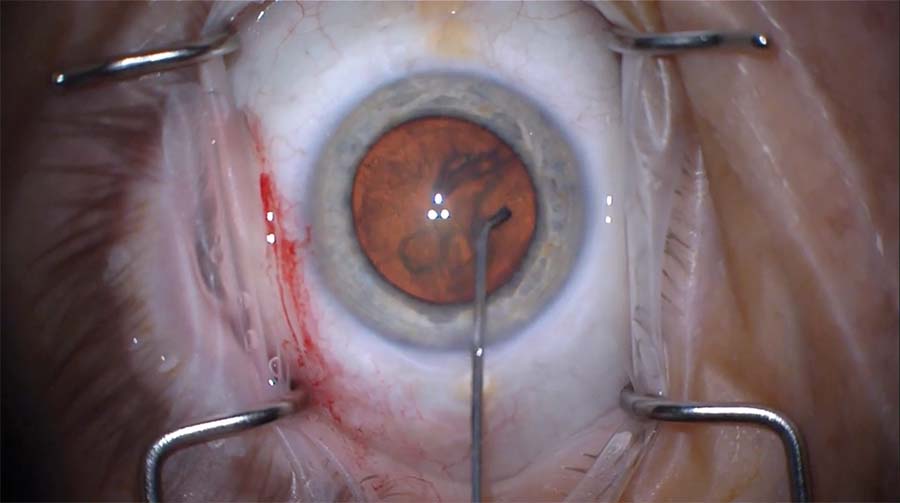
2. Hydrodelineation is performed. The irrigating cannula is angled slightly posteriorly so that fluid travels within the lamellae of the lens to separate the cortex and the endonucleus without disturbing the posterior capsule.
3. A phaco needle is used to remove the anterior cortex and epinucleus and to expose the endonucleus. A central groove is created slowly and carefully to minimize displacement of the lens. The groove propagates across the lens nucleus with the help of a Drysdale nucleus manipulator and the phaco needle.
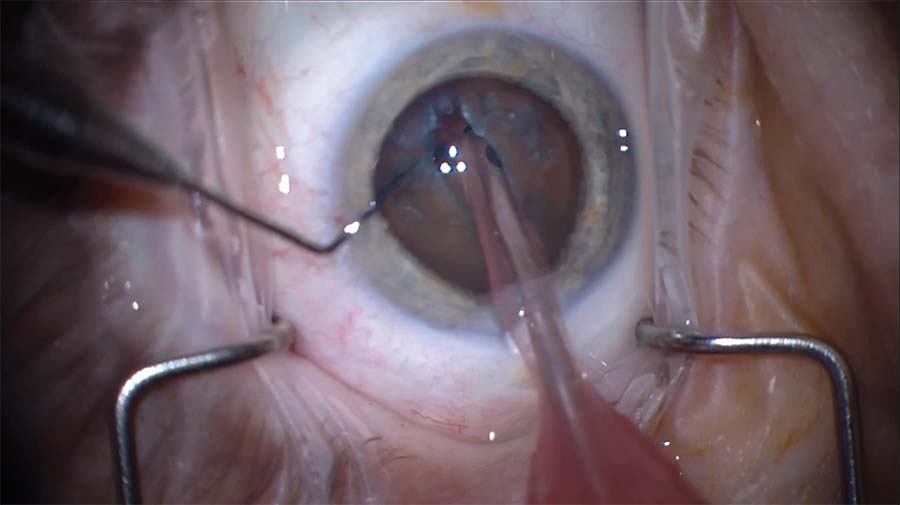
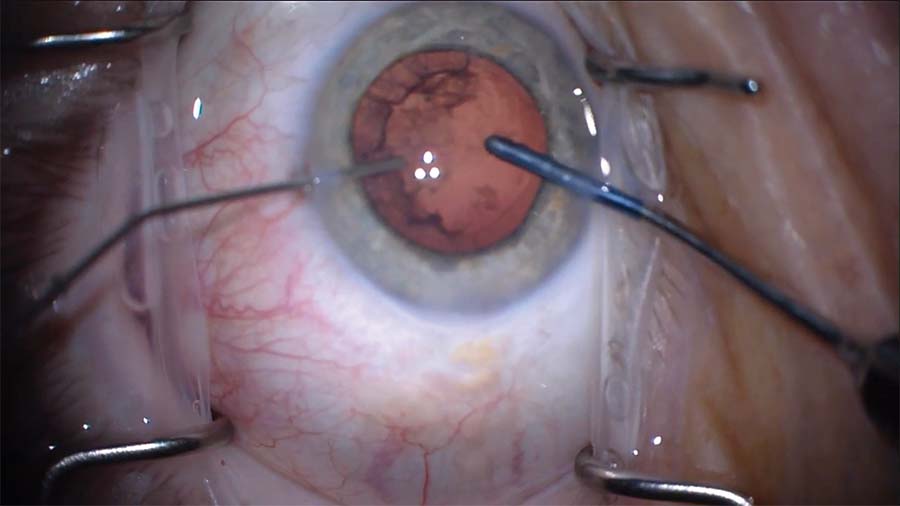
4. The nucleus is rotated slightly clockwise to facilitate engagement, and a piece of the nucleus is flipped up into the anterior chamber and emulsified. The second half of the nucleus is then impaled, drawn toward the phaco tip, and emulsified.
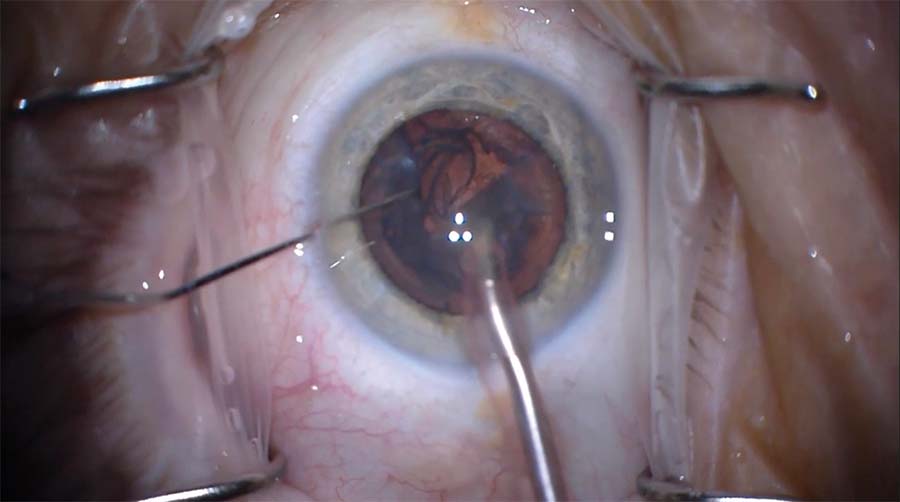
5. Slow engagement of the epinucleus is attempted by beginning away from the capsular opening and working toward it. When that fails, a Drysdale nucleus manipulator is placed back inside the eye and slowly worked around the epinucleus to reposition it and help draw it into the anterior chamber.
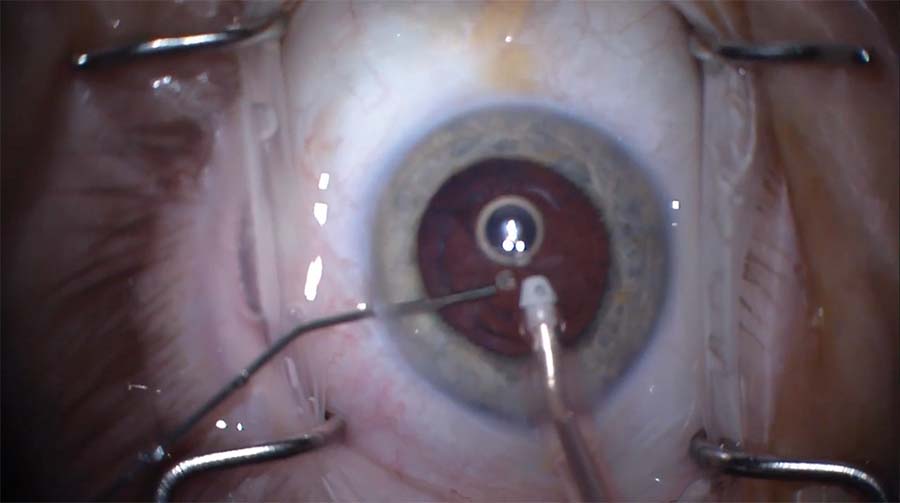
6. An I/A handpiece is inserted into the eye to complete removal of the epinucleus. At this point, the opening in the posterior capsule is noticeable. A dispersive OVD is injected directly through the hole to tamponade the anterior vitreous face and hold it back.
7. A bimanual I/A technique is used. Irrigation and aspiration begin in the area away from the preexisting capsular opening and move toward the opening with slow and controlled movements.
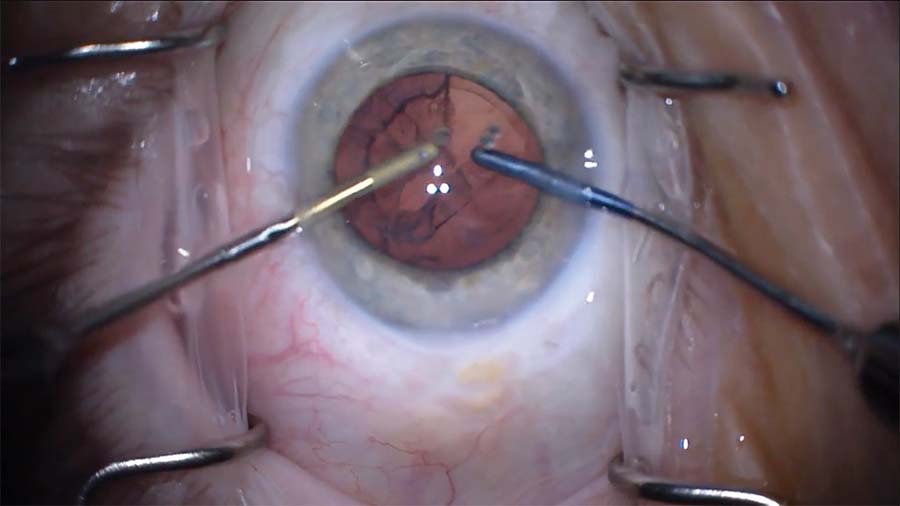
8. Vacuum is used to manipulate the remaining cortex toward the aspiration handpiece. The cortex is pulled when required but only in a tangential fashion rather than radially toward the center to distribute the forces more evenly.
9. Every time the handpiece enters and exits the eye, an additional amount of OVD is injected into the eye to hold back the vitreous.
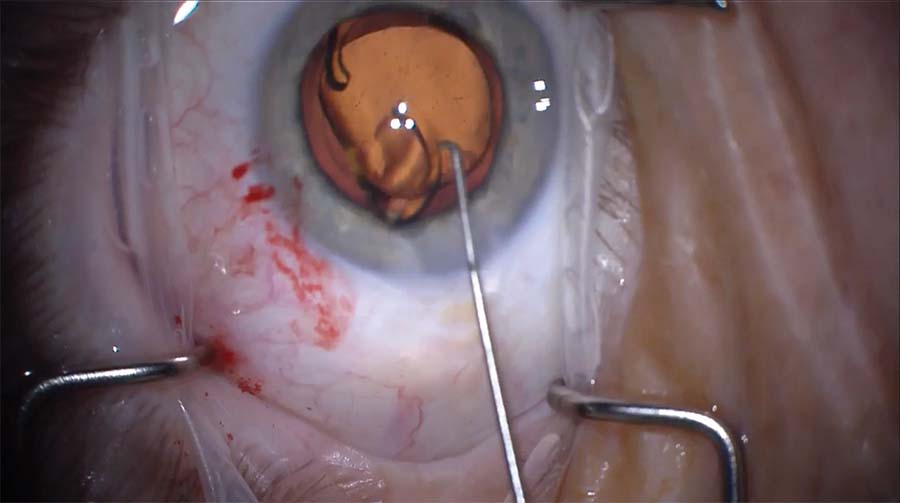
10. The posterior capsular opening is centrally located. The opening does not propagate during the surgery, and anterior vitreous prolapse is avoided. A one-piece acrylic IOL is implanted in the capsular bag, and the OVD is aspirated. At the end of the case, the pupil is round, the lens is well centered, and the wounds are watertight.