Since we began using the KAMRA corneal inlay (CorneaGen), we’ve learned a lot about best practices in surgical technique that yield the greatest postoperative outcomes. One of the most important strategies learned is that the inlay’s happy place is deeper in the cornea than previously thought.
When the FDA approved the KAMRA inlay, implantation was initially targeted for a shallow depth of about 200 µm below the corneal surface. After reviewing analysis of KAMRA inlay outcomes, stratified by implant depth as a percent of total corneal thickness (Figure 1), we gradually began inserting it deeper into the cornea, where there are fewer keratocytes, in order to limit inflammation. Now, we aim to implant the inlay in the posterior two-thirds of the cornea, at a depth of 40% of the total corneal thickness, or at least 250 µm deep.
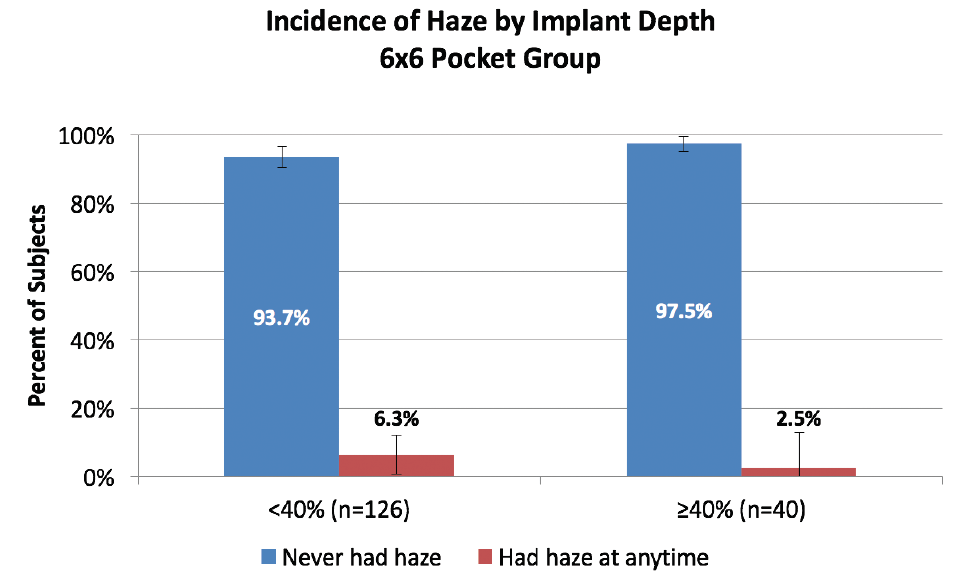
Figure 1. Implantation at or deeper than 40% of the total corneal thickness resulted in a reduced incidence of corneal haze in patients treated in the US IDE clinical trial for the KAMRA inlay.
DIFFERENCES IN VISUAL OUTCOMES
We believe there are three main advantages to deep implantation:
No. 1: Faster visual recovery. In short, patients will get to their endpoints sooner if the inlay is implanted at a depth of 40% of the total corneal thickness than they would if the inlay were implanted shallower. Now, we usually find that within a few weeks patients are seeing much better.
No. 2: Less likely to experience keratocyte activation. This translates into a reduced incidence of dry eye and of associated halos and glare. In going deeper, we found that it is rare for inflammation to develop around the inlay.
No. 3: Less likely to experience a hyperopic shift over time. The bottom line is results are more stable over time when it is implanted deeper in the cornea.
CONCLUSION
In our experience with KAMRA inlay implantation, we have found that deeper is best. Inserting the inlay at 40% of the total corneal depth or deeper helps patients to achieve faster visual recovery, with less risk of inflammation and less risk of a postoperative hyperopic shift.
Now that we have the collective knowledge of so many of our peers, the KAMRA inlay procedure is more refined. For those surgeons who are considering adopting the procedure, or for those who are still perfecting their technique, it is imperative that you follow the guidelines outlined in this supplement: a slightly myopic refraction preoperatively, a pristine ocular surface, and deeper implantation. These are the keys to success with the KAMRA inlay.
KAMRA is a trademark of CorneaGen. All other trademarks are property of their respective owners.


