
Differences between CONTOURA Vision (Alcon) and other LASIK diagnostic procedures were clear from the start. When you read that after a CONTOURA Vision procedure, over 30% of eyes have UCVA that exceeds preoperative BCVA,1 you know that CONTOURA’s WaveLight Topolyzer Vario (Alcon) component is producing measurements that are different from manifest refraction. The highly individualized topography-guided procedure produces excellent visual outcomes while reducing symptoms associated with LASIK, telling us that it, too, is different from previous technologies.1
When I began using CONTOURA Vision 12 months ago, I saw these differences firsthand. I did not embrace the system immediately. Instead, I spent time double-checking CONTOURA Vision against other technologies and cautiously integrating it into my treatment protocols. Over a 6-month period, I grew very satisfied with both the accuracy of the data and the surgical outcomes as well as surprised at the system’s ability to correct cases previously untreatable with LASIK. I learned to trust measured over manifest refraction and put my well-earned faith in the technology.
After CONTOURA Vision, patients are noticing vision clarity and detail that are very impressive, results in line with what the FDA study showed. I recently treated a 47-year-old dentist who had suffered with irregular astigmatism for years. His glasses and contact lenses were designed for “normal” patients with “normal” linear astigmatism. Because his astigmatism was not perfectly linear on topography, glasses and contacts helped his vision but did not perfect it. Following treatment with CONTOURA Vision, he was thrilled with his crisp vision and realized how much detail he had been missing.
“Now, even off-the-shelf reading glasses are amazing! It is as if I am wearing surgical loops,” he told me. He also notes that he no longer sees starbursts while driving.
Here, I share three cases in which I used CONTOURA Vision during this learning curve period, illustrating how the system compared to other tests and how it performed in surgery. The cases range from a straightforward procedure to a case that was untreatable with other standard LASIK technologies. Note: Because CONTOURA Vision requires surgeons to treat in minus cylinder, all refractions are presented in minus cylinder to prevent confusion.
Case 1: Close Manifest and Measured Astigmatism
This is an example of the simplest and easiest type of case for using CONTOURA Vision. The patient is a 31-year-old man with mild myopia and low astigmatism. The manifest refraction (-3.00 -0.50 x 25 20/15) matched well with Vario measured cylinder for both magnitude and axis (-0.34D x 5) (Figure 1A). Orbscan (Bausch + Lomb) measurements were -0.2D x 15 (Figure 1B).
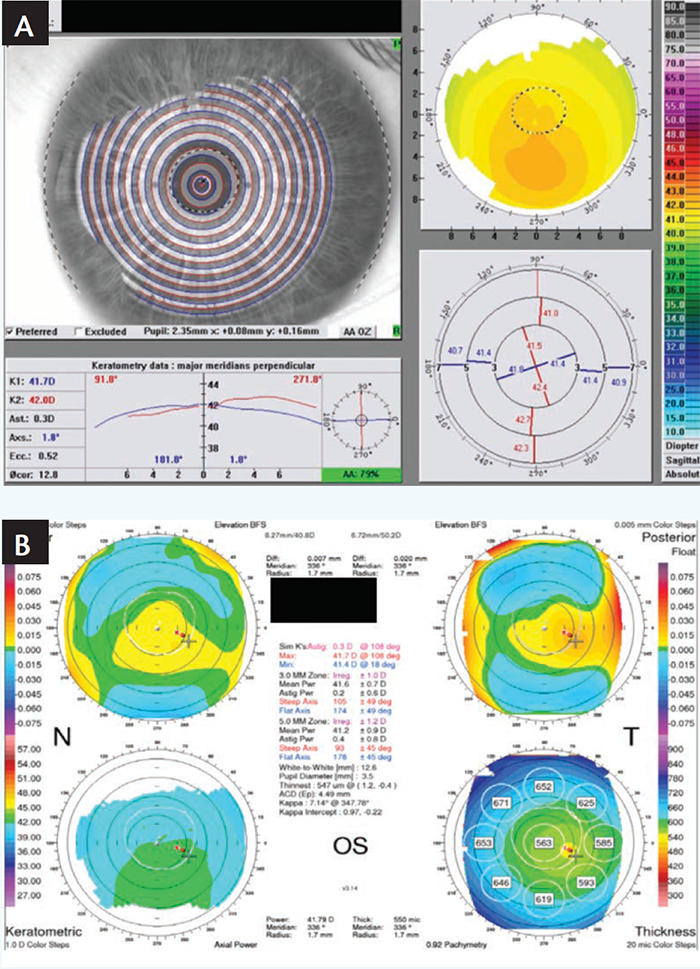
Figure 1. Preoperative Vario scan (A) and Orbscan (B) of a patient with mild myopia and low astigmatism.
On my CONTOURA Vision treatment screen, I looked at the Vario measurements and zeroed out the sphere and cylinder treatments on the “Modified” line. This triggered the system to display the pure topographic treatment planned by CONTOURA Vision on a color map, which indicates the amount of tissue to be removed in different areas (Figure 2).
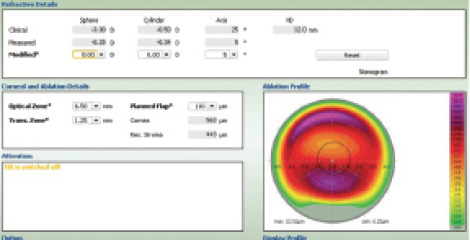
Figure 2. The CONTOURA Vision treatment screen.
The final treatment programmed for this patient was -3.25 -0.34 x 5 (the measured, not the manifest refraction). Treatment was perfectly centered thanks to the highly sensitive pupil-tracking technology. One day after surgery, the Vario scan showed that the treated cornea of the patient’s left eye had smooth, even contours (Figure 3). UCVA was 20/20 day 1 and 20/15 at 2 months, with plano sphere.
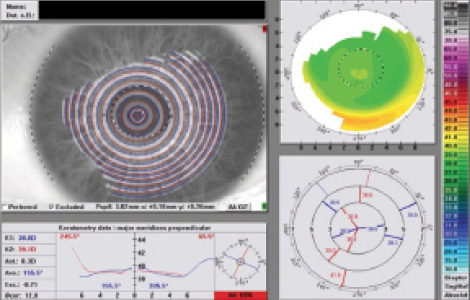
Figure 3. One day after surgery, the Vario scan showed that the treated cornea of the patient’s left eye had smooth, even contours.
Case 2: Measured Astigmatism Exceeds Manifest
I commonly encounter cases where the manifest refraction shows less astigmatism than the Vario measured refraction. I must decide whether to fall back on my previous LASIK experience and treat the manifest or trust the Vario measurement and treat based on its recommendation.
In one such case, a 39-year-old man with moderate myopia and no astigmatism on manifest (OS -4.50 sph 20/15) showed measured astigmatism with Vario (OS -0.99 x 174). In the early stages of using CONTOURA Vision, I found it important to prove to myself that the Vario measured astigmatism was “real” when it differed from the manifest. To verify the measurement, I would compare the Vario’s results to those of a second topographer. It is hard to break years of LASIK experience, and trusting measurements over manifest feels somehow “wrong” at first. No surgeon wants to make a mistake and treat a full 1.00 D of cylinder not seen on manifest. Satisfied with the verification, I learned to trust the technology and treat the true measured astigmatism when using CONTOURA Vision.
In this case, the Orbscan (OS -1.00 x 1) verified the Vario measurements. The Vario and the Orbscan topographers both showed about -1.00 D of cylinder at an axis of about 180° (Figure 4). This assured me that the astigmatism measured by Vario was correct, despite the manifest showing a purely spherical correction.
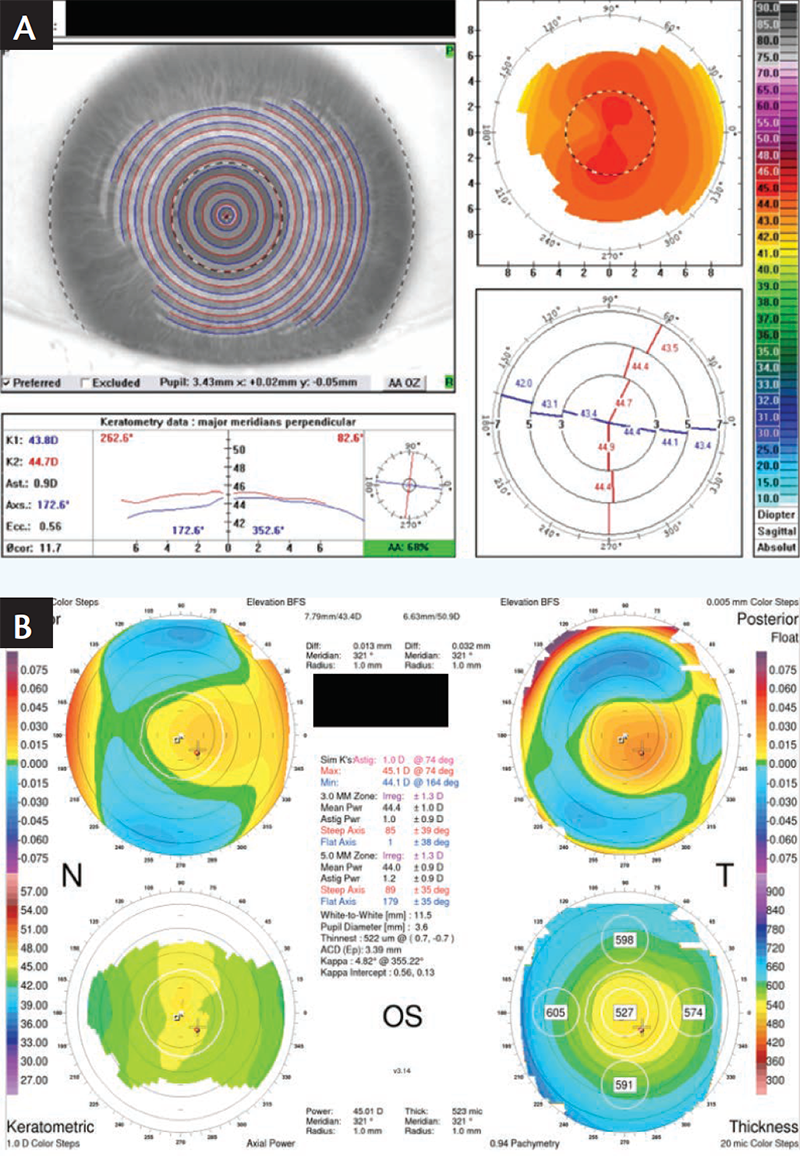
Figure 4. Preoperative Vario scan (A) and Orbscan (B) of a patient with moderate myopia.
I examined the sagittal images of multiple Vario scans for the left eye and found them to be of good quality and in close agreement (Figure 5). On the CONTOURA Vision treatment screen, I zeroed out the sphere and cylinder and viewed the purely topographic treatment that CONTOURA Vision would place on the eye.
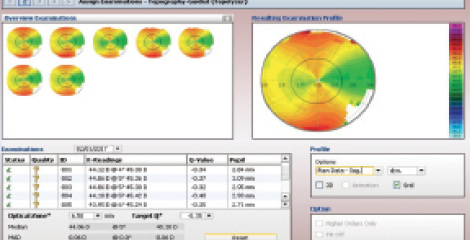
Figure 5. Sagittal images of multiple Vario scans of the patient’s left eye.
The ablation profile showed why the manifest showed no astigmatism while Vario did. Looking at the topographic treatment map, two of the three purple areas where CONTOURA Vision was planning the most tissue removal were located in a vertical line. These elevated areas bend light as if they are cylinders. Because the axis of these raised topographic areas was located at 90° but the true Vario measured astigmatism was located at 180°, the two counterbalanced one another (Figure 6). Thus, the image reaching the retina (the manifest) showed sphere only and no astigmatism.
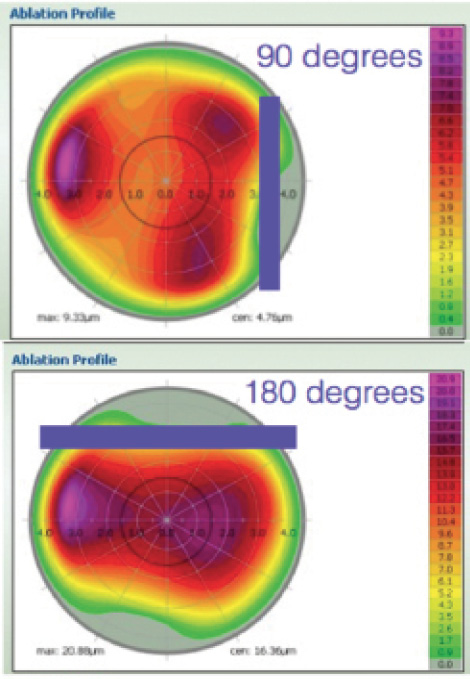
Figure 6. Topography treatment map versus Vario-measured cylinder treatment only.
Treatment was programmed at -4.13 -0.75 x 174, slightly less than the -0.99 x 174 that the Vario had measured. At the time, I did not trust the technology enough to treat 1.00 D more than manifest. This was a mistake. Three months after surgery, the manifest refraction was OS plano -0.25 x 160 20/15. With the topography treated and perfected by CONTOURA Vision, the true cylinder was reflected in the manifest. Had I treated the full -0.99 measured by Vario, the patient would not have had a residual -0.25 at 160. Now I trust the technology and treat the full magnitude and axis that Vario measures to remove the topographic abnormalities of a cornea.
UCVA for this patient was 20/20 at day 1 and 20/20+1 at 3 months. Vario scan showed a beautiful, smooth topographic contour to the cornea with virtually no astigmatism or irregularities. With the topographic abnormalities treated, there was nothing to counterbalance the true cylinder that remained on the cornea. The postoperative Vario scan measured 0.30 D cylinder at 172.4°, very close to the manifest of 0.25 D of cylinder at 160 (Figure 7).
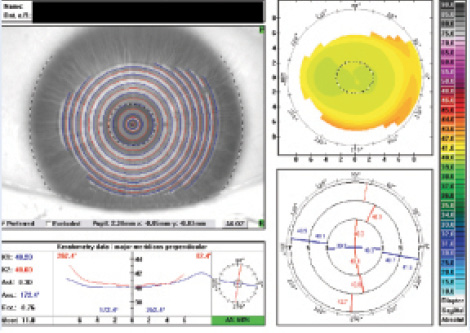
Figure 7. Postoperative Vario scan measured 0.30 D cylinder at 172.4°, very close to the manifest of 0.25 D of cylinder at 160.
Case 3: Choosing Measured Over Manifest
In another case where the manifest astigmatism and Vario measured astigmatism varied, a 28-year-old man had an OD manifest refraction of -6.75 -0.50 x 175 sph 20/15-2, compared to a Vario measurement of -1.50 D at axis 1.5°. Orbscan measured -1.10 D at axis 30 (Figure 8). Once again, I had to make the critical decision to treat based on the manifest cylinder or the Vario measurements.
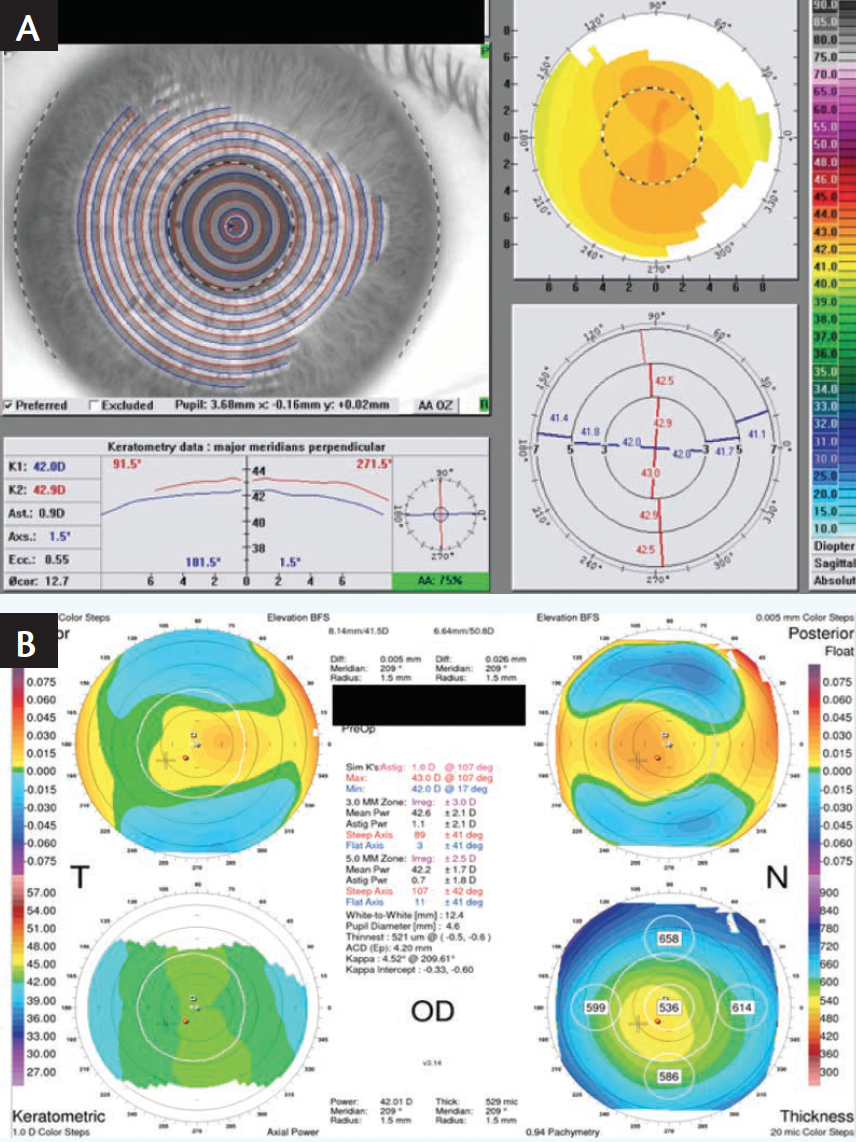
Figure 8. Preoperative Vario scan (A) and Orbscan (B) of a 28-year-old patient.
By removing the sphere and cylinder from the topographic treatment map, surgeons can see an isolated view of the topographic abnormalities that CONTOURA Vision will treat. In this case, this view showed why the manifest cylinder was different in magnitude than the Vario measured cylinder. While some of the topographic abnormalities were mimicking a minus cylinder at 180°, more abnormalities mimicked a minus cylinder at 90°. The topographic abnormalities at the 90° axis counterbalanced both the topographic abnormalities at the 180° axis and the true corneal cylinder measured by Vario. The result was the manifest, which showed astigmatism lower in magnitude than that measured by Vario (Figure 9).
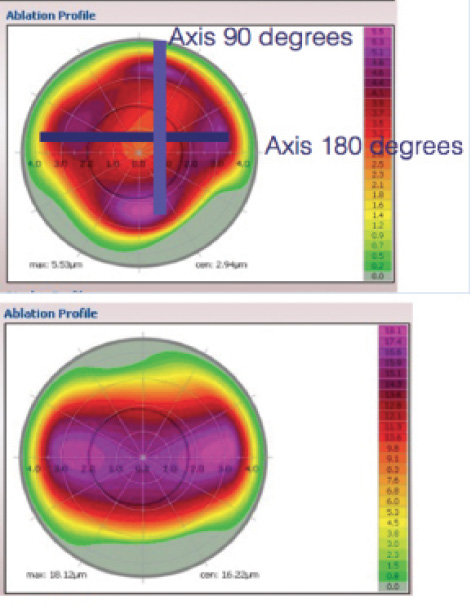
Figure 9. Topography treatment map versus Vario-measured cylinder treatment only.
CONTOURA Vision treatment was programmed to -6.40 -1.00 x 2. Here the spherical portion of the treatment was purposely reduced below the manifest sphere. Because I increased the treated negative cylinder above the manifest negative cylinder, I needed to reduce the spherical treatment by one half the delta (change) in cylinder to keep the spherical equivalent of the treatment equal to the spherical equivalent of the manifest. A small adjustment was also made to the sphere based on the nomogram for my Wavelight Ex500 Excimer Laser (Alcon).
UCVA was 20/20 at day 1. At 1 month, OD UCVA was 20/20, and OD manifest refraction was plano +0.25 x 05 20/20. The 1 month postoperative Vario topographic analysis showed how CONTOURA Vision treatment left a smooth, beautiful topographic contour to the cornea with virtually no topographic abnormalities remaining. Vario’s postoperative scan shows the pupil marked in a hashed line of black and white, with the circular myopic treatment pattern on the vertex of the cornea, not centered on the pupil (Figure 10). This is a key feature of how CONTOURA Vision delivers such exceptional results. The Orbscan topography taken 1 month postoperatively showed perfection in the axial power map.
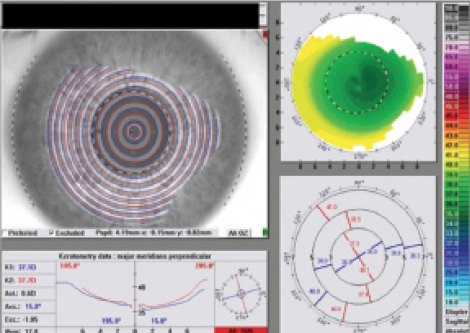
Figure 10. Vario’s postoperative scan shows the pupil marked in a hashed line of black and white, with the circular myopic treatment pattern on the vertex of the cornea, not centered on the pupil.
CONTOURA Vision Inspires Confidence
Every cornea has some topographic abnormalities, but in the past our standard or wavefront-optimized treatments left them in place. CONTOURA Vision treats the cornea completely.
We all want to routinely boost LASIK visual outcomes while reducing the residual symptoms of the procedure. To acquire this capability, we need to use topography-guided treatments such as CONTOURA Vision. To best use CONTOURA Vision, we need to make a mental leap and trust measured refraction over the manifest refraction we have relied on for so long. It is not easy to do that at first, but if you learn to trust the technology, CONTOURA Vision will improve your patients’ results. Better results and happier patients will convince you to embrace this next-generation technology with confidence.
1. Stulting RD, Fant BS; T-CAT Study Group. Results of topography-guided laser in situ keratomileusis custom ablation treatment with a refractive excimer laser. J Cataract Refract Surg. 2016;42:11–18.
This information pertains to all WaveLight Excimer Laser Systems, including the WaveLight ALLEGRETTO WAVE, the ALLEGRETTO WAVE Eye-Q, and the WaveLight EX500.
Caution: Federal (U.S.) law restricts the WaveLight Excimer Laser Systems to sale by or on the order of a physician. Only practitioners who are experienced in the medical mangement and surgical treatment of the cornea, who have been trained in laser refractive surgery (including laser calibration and operation) should use a WaveLight Excimer Laser System.
Indications: FDA has approved the WaveLight Excimer Laser systems for use in laser-assisted in situ keratomileusis (LASIK) treatments for:
- the reduction or elimination of myopia of up to –12.00 D and up to 6.00 D of astigmatism at the spectacle plane;
- the reduction or elimination of hyperopia up to +6.00 D with and without astigmatic refractive errors up to 5.00 D at the spectacle plane, with a maximum manifest refraction spherical equivalent of +6.00 D;
- the reduction or elimination of naturally occurring mixed astigmatism of up to 6.00 D at the spectacle plane; and
- the wavefront-guided reduction or elimination of myopia of up to –7.00 D and up to 3.00 D of astigmatism at the spectacle plane.
In addition, FDA has approved the WaveLight ALLEGRETTO WAVE Eye-Q Excimer Laser System, when used with the WaveLight ALLEGRO Topolyzer and topography-guided treatment planning software for topographyguided LASIK treatments for the reduction or elimination of up to –9.00 D of myopia, or for the reduction or elimination of myopia with astigmatism, with up to –8.00 D of myopia and up to 3.00 D of astigmatism.
The WaveLight Excimer Laser Systems are only indicated for use in patients who are 18 years of age or older (21 years of age or older for mixed astigmatism) with documentation of a stable manifest refraction defined as ≤0.50 D of preoperative spherical equivalent shift over one year prior to surgery, exclusive of changes due to unmasking latent hyperopia.
Contraindications: The WaveLight Excimer Laser Systems are contraindicated for use with patients who:
- are pregnant or nursing;
- have a diagnosed collagen vascular, autoimmune or immunodeficiency disease;
- have been diagnosed with keratoconus or if there are any clinical pictures suggestive of keratoconus;
- are taking isotretinoin (Accutane*) and/or amiodarone hydrochloride (Cordarone*);
- have severe dry eye;
- have corneas too thin for LASIK;
- have recurrent corneal erosion;
- have advanced glaucoma; or
- have uncontrolled diabetes.
Warnings: The WaveLight Excimer Laser Systems are not recommended for use with patients who have:
- systemic diseases likely to affect wound healing, such as connective tissue disease, insulin dependent diabetes, severe atopic disease or an immunocompromised status;
- a history of Herpes simplex or Herpes zoster keratitis;
- significant dry eye that is unresponsive to treatment;
- severe allergies;
- a history of glaucoma;
- an unreliable preoperative wavefront examination that precludes wavefront-guided treatment; or
- a poor quality preoperative topography map that precludes topography-guided LASIK treatment.
The wavefront-guided LASIK procedure requires accurate and reliable data from the wavefront examination. Every step of every wavefront measurement that may be used as the basis for a wavefront-guided LASIK procedure must be validated by the user. Inaccurate or unreliable data from the wavefront examination will lead to an inaccurate treatment.
Topography-guided LASIK requires preoperative topography maps of sufficient quality to use for planning a topography-guided LASIK treatment. Poor quality topography maps may affect the accuracy of the topography-guided LASIK treatment and may result in poor vision after topography-guided LASIK.
Precautions: The safety and effectiveness of the WaveLight Excimer Laser Systems have not been established for patients with:
- progressive myopia, hyperopia, astigmatism and/or mixed astigmatism, ocular disease, previous corneal or intraocular surgery, or trauma in the ablation zone;
- corneal abnormalities including, but not limited to, scars, irregular astigmatism and corneal warpage;
- residual corneal thickness after ablation of less than 250 microns due to the increased risk for corneal ectasia;
- pupil size below 7.0 mm after mydriatics where applied for wavefront-guided ablation planning;
- history of glaucoma or ocular hypertension of >23 mm Hg;
- taking the medications sumatriptan succinate (Imitrex*);
- corneal, lens and/or vitreous opacities including but not limited to cataract;
- iris problems including, but not limited to, coloboma and previous iris surgery compromising proper eye tracking; or
- taking medications likely to affect wound healing including (but not limited to) antimetabolites.
In addition, safety and effectiveness of the WaveLight Excimer Laser Systems have not been established for:
- treatments with an optical zone <6.0 mm or >6.5 mm in diameter, or an ablation zone >9.0 mm in diameter; or
- wavefront-guided treatment targets different from emmetropia (plano) in which the wavefront calculated defocus (spherical term) has been adjusted.
In the WaveLight Excimer Laser System clinical studies, there were few subjects with cylinder amounts >4 D and ≤6 D. Not all complications, adverse events, and levels of effectiveness may have been determined for this population.
Pupil sizes should be evaluated under mesopic illumination conditions. Effects of treatment on vision under poor illumination cannot be predicted prior to surgery.
Adverse Events and Complications
Myopia: In the myopia clinical study, 0.2% (2/876) of the eyes had a lost, misplaced, or misaligned flap reported at the 1 month examination.
The following complications were reported 6 months after LASIK: 0.9% (7/818) had ghosting or double images in the operative eye; 0.1% (1/818) of the eyes had a corneal epithelial defect.
Hyperopia: In the hyperopia clinical study, 0.4% (1/276) of the eyes had a retinal detachment or retinal vascular accident reported at the 3 month examination.
The following complications were reported 6 months after LASIK: 0.8% (2/262) of the eyes had a corneal epithelial defect and 0.8% (2/262) had any epithelium in the interface.
Mixed Astigmatism: In the mixed astigmatism clinical study, two adverse events were reported. The first event involved a patient who postoperatively was subject to blunt trauma to the treatment eye 6 days after surgery. The patient was found to have an intact globe with no rupture, inflammation or any dislodgement of the flap. UCVA was decreased due to this event. The second event involved the treatment of an incorrect axis of astigmatism. The axis was treated at 60 degrees instead of 160 degrees.
The following complications were reported 6 months after LASIK: 1.8% (2/111) of the eyes had ghosting or double images in the operative eye.
Wavefront-Guided Myopia: The wavefrontguided myopia clinical study included 374 eyes treated; 188 with wavefront-guided LASIK (Study Cohort) and 186 with Wavefront-Optimized LASIK (Control Cohort). No adverse events occurred during the postoperative period of the wavefront-guided LASIK procedures. In the Control Cohort, one subject undergoing traditional LASIK had the axis of astigmatism programmed as 115 degrees instead of the actual 155 degree axis. This led to cylinder in the left eye.
The following complications were reported 6 months after wavefront-guided LASIK in the Study Cohort: 1.2% (2/166) of the eyes had a corneal epithelial defect; 1.2% (2/166) had foreign body sensation; and 0.6% (1/166) had pain. No complications were reported in the Control Cohort.
Topography-Guided Myopia: There were six adverse events reported in the topographyguided myopia study. Four of the eyes experienced transient or temporary decreases in vision prior to the final 12 month follow-up visit, all of which were resolved by the final follow-up visit. One subject suffered from decreased vision in the treated eye, following blunt force trauma 4 days after surgery. One subject experienced retinal detachment, which was concluded to be unrelated to the surgical procedure.
Clinical Data
Myopia: The myopia clinical study included 901 eyes treated, of which 813 of 866 eligible eyes were followed for 12 months. Accountability at 3 months was 93.8%, at 6 months was 91.9%, and at 12 months was 93.9%. Of the 782 eyes that were eligible for the uncorrected visual acuity (UCVA) analysis of effectiveness at the 6-month stability time point, 98.3% were corrected to 20/40 or better, and 87.7% were corrected to 20/20 or better. Subjects who responded to a patient satisfaction questionnaire before and after LASIK reported the following visual symptoms at a “moderate” or “severe” level at least 1% higher at 3 months post-treatment than at baseline: visual fluctuations (28.6% vs. 12.8% at baseline).
Long-term risks of LASIK for myopia with and without astigmatism have not been studied beyond 12 months.
Hyperopia: The hyperopia clinical study included 290 eyes treated, of which 100 of 290 eligible eyes were followed for 12 months. Accountability at 3 months was 95.2%, at 6 months was 93.9%, and at 12 months was 69.9%. Of the 212 eyes that were eligible for the UCVA analysis of effectiveness at the 6-month stability time point, 95.3% were corrected to 20/40 or better, and 69.4% were corrected to 20/20 or better. Subjects who responded to a patient satisfaction questionnaire before and after LASIK reported the following visual symptoms as “much worse” at 6 months post-treatment: halos (6.4%); visual fluctuations (6.1%); light sensitivity (4.9%); night driving glare (4.2%); and glare from bright lights (3.0%).
Long-term risks of LASIK for hyperopia with and without astigmatism have not been studied beyond 12 months.
Mixed Astigmatism: The mixed astigmatism clinical study included 162 eyes treated, of which 111 were eligible to be followed for 6 months. Accountability at 1 month was 99.4%, at 3 months was 96.0%, and at 6 months was 100.0%. Of the 142 eyes that were eligible for the UCVA analysis of effectiveness at the 6-month stability time point, 97.3% achieved acuity of 20/40 or better, and 69.4% achieved acuity of 20/20 or better. Subjects who responded to a patient satisfaction questionnaire before and after LASIK reported the following visual symptoms at a “moderate” or “severe” level at least 1% higher at 3 months post-treatment than at baseline: sensitivity to light (52.9% vs. 43.3% at baseline); visual fluctuations (43.0% vs. 32.1% at baseline); and halos (42.3% vs. 37.0% at baseline).
Long-term risks of LASIK for mixed astigmatism have not been studied beyond 6 months.
Wavefront-Guided Myopia: The wavefrontguided myopia clinical study included 374 eyes treated; 188 with wavefront-guided LASIK (Study Cohort) and 186 with Wavefront-Optimized LASIK (Control Cohort). 166 of the Study Cohort and 166 of the Control Cohort were eligible to be followed at 6 months. In the Study Cohort, accountability at 1 month was 96.8%, at 3 months was 96.8%, and at 6 months was 93.3%. In the Control Cohort, accountability at 1 month was 94.6%, at 3 months was 94.6%, and at 6 months was 92.2%.
Of the 166 eyes in the Study Cohort that were eligible for the UCVA analysis of effectiveness at the 6-month stability time point, 99.4% were corrected to 20/40 or better, and 93.4% were corrected to 20/20 or better. Of the 166 eyes in the Control Cohort eligible for the UCVA analysis of effectiveness at the 6-month stability time point, 99.4% were corrected to 20/40 or better, and 92.8% were corrected to 20/20.
In the Study Cohort, subjects who responded to a patient satisfaction questionnaire before and after LASIK reported the following visual symptoms at a “moderate” or “severe” level at least 1% higher at 3 months post-treatment than at baseline: light sensitivity (47.8% vs. 37.2% at baseline) and visual fluctuations (20.0% vs. 13.8% at baseline). In the Control Cohort, the following visual symptoms were reported at a “moderate” or “severe” level at least 1% higher at 3 months post-treatment than at baseline: halos (45.4% vs. 36.6% at baseline) and visual fluctuations (21.9% vs. 18.3% at baseline).
Long-term risks of wavefront-guided LASIK for myopia with and without astigmatism have not been studied beyond 6 months.
Topography-Guided Myopia: The topographyguided myopia clinical study included 249 eyes treated, of which 230 eyes were followed for 12 months. Accountability at 3 months was 99.2%, at 6 months was 98.0%, and at 12 months was 92.4%. Of the 247 eyes that were eligible for the UCVA analysis at the 3-month stability time point, 99.2% were corrected to 20/40 or better, and 92.7% were corrected to 20/20 or better. Subjects who responded to a patient satisfaction questionnaire before and after LASIK reported the following visual symptoms as “marked” or “severe” at an incidence greater than 5% at 1 month after surgery: dryness (7% vs. 4% at baseline) and light sensitivity (7% vs. 5% at baseline). Visual symptoms continued to improve with time, and none of the visual symptoms were rated as being “marked” or “severe” with an incidence of at least 5% at 3 months or later after surgery.
Long-term risks of topography-guided LASIK for myopia with and without astigmatism have not been studied beyond 12 months.
Information for Patients: Prior to undergoing LASIK surgery with a WaveLight Excimer Laser System, prospective patients must receive a copy of the relevant Patient Information Booklet, and must be informed of the alternatives for correcting their vision, including (but not limited to) eyeglasses, contact lenses, photorefractive keratectomy, and other refractive surgeries.
Attention: Please refer to a current WaveLight Excimer Laser System Procedure Manual for a complete listing of the indications, complications, warnings, precautions, and side effects.
*Trademarks are property of their respective owners.
