A cyclodialysis cleft is a separation of the longitudinal fibers of the ciliary muscle from the scleral spur. This separation creates a direct connection between the anterior chamber and suprachoroidal space, which can lead to low IOP and clinical manifestations of hypotony due to the increase in aqueous outflow. Cyclodialysis clefts occur mainly from trauma and are rare after intraocular surgery. Inadvertent cyclodialysis clefts, however, can occur when MIGS is combined with cataract surgery. The use of MIGS devices in the aqueous outflow pathway at the time of cataract surgery is increasing, so it is important for surgeons to have a heightened awareness of this possible intraoperative complication.
CAUSES
Cyclodialysis cleft creation during standalone cataract surgery is rare with modern clear corneal phaco techniques, but cleft creation after phacoemulsification with a scleral tunnel and after extracapsular cataract extraction has been reported.1,2 The exact cause of the clefts during these procedures is unclear, but it is thought to be related to angle trauma during iris manipulation or lens implantation. In a series of three cases of cyclodialysis cleft after routine phacoemulsification, all of the patients had a history of blunt ocular trauma in the affected eye, and the postoperative cleft was thought to be related to activation of a dormant cleft in the traumatized eye during surgery.3
Combining MIGS with cataract surgery increases the possibility of inadvertent cleft creation during surgery. The malpositioning of MIGS devices and poor intraoperative visualization of angle structures can lead to inadvertent injury of the ciliary body and cyclodialysis cleft formation. Iatrogenic cyclodialysis clefts have been reported after procedures involving a Trabectome (MicroSurgical Technology),4 surgery with a Kahook Dual Blade (New World Medical),5 and microhook trabeculotomy.6 The recalled CyPass Micro-Stent intentionally created a controlled cyclodialysis cleft, but those larger than 2 mm were not found to be associated with hypotony or the need for reoperation.7
DIAGNOSIS
Intraoperatively, a cyclodialysis cleft may be identified with a gonioscopic view under the microscope if heme, corneal edema, and other opacities do not block the surgeon’s view of the angle. Under gonioscopy, a cleft appears as an abnormal region posterior to the scleral spur with posterior displacement of the ciliary body and iris root (Figure 1). The cleft region may vary in appearance and color (white, black, or gray). If angle injury is suspected after intraoperative difficulty with a MIGS device, an OVD can be injected into the area where the MIGS device was used to improve the gonioscopic view and search for a potential cleft. If the gonioscopic view is poor, an endoscope can also be used intraoperatively to search for a cyclodialysis cleft.
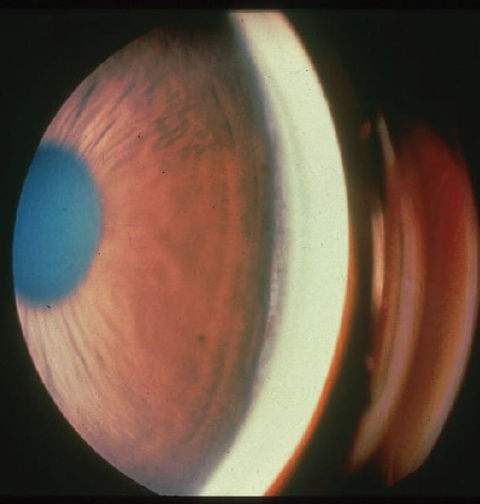
Figure 1. Gonioscopic view of a cyclodialysis cleft.
Courtesy of Joseph Caprioli, MD
Postoperatively, a high index of suspicion makes the prompt identification of an iatrogenic cyclodialysis cleft more likely. Suspicious findings include low IOP and/or clinical signs of ocular hypotony in the absence of a wound leak after cataract surgery. If there is no significant corneal edema, a cleft may be visualized with gonioscopy in the clinic. To aid with diagnosis, ultrasound biomicroscopy (Figure 2) and anterior segment OCT may also be used to identify a separation of the ciliary body from the scleral spur.
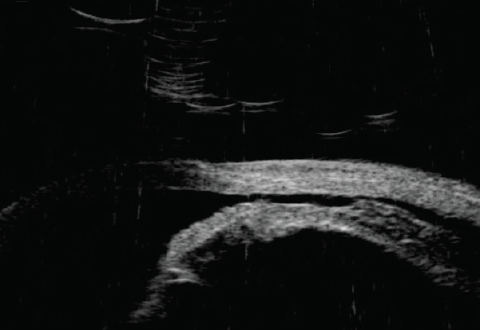
Figure 2. Cyclodialysis cleft on ultrasound biomicroscopy.
MANAGEMENT
Small clefts may resolve with observation alone. The mainstay of medical therapy for a cyclodialysis cleft is administering cycloplegic agents to relax the ciliary muscle so that the detached fibers can be reapposed to the scleral spur.8 The role of steroids is less clear; studies have hypothesized that both increasing and decreasing the steroid dose can facilitate cleft closure.9,10
Multiple laser techniques have been reported for cleft repair. The theory is that laser ablation induces a localized inflammatory reaction that promotes cleft closure. Argon laser energy can be applied within the cleft site using a gonioscopy lens. Transscleral diode photocoagulation techniques using the G-probe with a double row of applications have also been reported, and transscleral techniques with an Nd:YAG laser using a noncontact technique with two rows of applications have been described.10
Key Points
- Inadvertent cyclodialysis clefts can occur with the use of MIGS devices during cataract surgery.
- Maintain a high index of suspicion for a cleft in patients who experience postoperative hypotony without a wound leak.
- Several conservative and surgical options exist for cyclodialysis cleft repair.
Clefts that cannot be managed by more conservative measures may require surgical repair. The surgical mainstay is direct cyclopexy to appose the sclera and the wall of the ciliary body. This can be achieved using several different techniques with possible adjunctive treatments and modifications. Most techniques involve the creation of partial- or full-thickness scleral flaps to access the ciliary body, which is then sutured to the undersurface of the sclera. Nylon or polypropylene sutures are passed externally or through the anterior chamber to appose the sclera to the ciliary body.10-12 Cryotherapy is often used as an adjunct to aid with cleft closure.
In addition to direct cyclopexy, other novel surgical techniques, including gas tamponade with cryotherapy,13 internal cerclage with a capsular tension ring,14 placement of an IOL in the sulcus with rotation of the lens to appose the area of the cleft,9 and temporary anterior scleral buckling,10 have been used for cleft repair.
COMPLICATIONS
If a cyclodialysis cleft remains unresolved for a prolonged time, chronic issues can arise from ocular hypotony. Hypotony maculopathy, corneal edema, and disc edema can all lead to a temporary or permanent decrease in visual acuity.
After the successful closure of a cleft, many eyes undergo a period of dramatic and often painful elevation in IOP. The majority of these cases are self-limited and resolve with topical and oral IOP-lowering therapy, but a small proportion may require filtration surgery for adequate IOP reduction.
1. Aminlari A. Inadvertent cyclodialysis cleft. Ophthalmic Surg. 1993;24:331-335.
2. Maffett MJ, O’Day DM. Cyclodialysis cleft following a scleral tunnel incision. Ophthalmic Surg. 1994;25(6):387-388.
3. Mushtaq B, Chiang MYM, Kumar V, Ramanathan US, Shah P. Phacoemulsification, persistent hypotony, and cyclodialysis clefts. J Cataract Refract Surg. 2005;31(7):1428-1432.
4. Berk TA, An JA, Ahmed IIK. Inadvertent cyclodialysis cleft and hypotony following ab-interno trabeculotomy using the Trabectome device requiring surgical repair. J Glaucoma. 2017;26(8):742-746.
5. Shue A, Levine RM, Gallousis GM, Teng CC. Cyclodialysis cleft associated with Kahook Dual Blade goniotomy. J Curr Glaucoma Pract. 2019;13(2):74-76.
6. Ishida A, Mochiji M, Manabe K, Matsuoka Y, Tanito M. Persistent hypotony and annular ciliochoroidal detachment after microhook ab interno trabeculotomy. J Glaucoma. 2020;29(9):807-812.
7. Vold S, Ahmed IIK, Craven ER, et al; CyPass Study Group. Two-year COMPASS trial results: supraciliary microstenting with phacoemulsification in patients with open-angle glaucoma and cataracts. Ophthalmology. 2016;123(10):2103-2112.
8. Ormerod LD, Baerveldt G, Sunalp MA, Riekhof FT. Management of the hypotonous cyclodialysis cleft. Ophthalmology. 1991;98(9):1384-1393.
9. Malandrini A, Balestrazzi A, Martone G, Tosi GM, Caporossi A. Diagnosis and management of traumatic cyclodialysis cleft. J Cataract Refract Surg. 2008;34(7):1213-1216.
10. Ioannidis AS, Barton K. Cyclodialysis cleft: causes and repair. Curr Opin Ophthalmol. 2010;21(2):150-154.
11. Küchle M, Naumann GO. Direct cyclopexy for traumatic cyclodialysis with persisting hypotony: report in 29 consecutive patients. Ophthalmology. 1995;102(2):322-333.
12. Hwang JM, Ahn K, Kim C, Park KA, Kee C. Ultrasonic biomicroscopic evaluation of cyclodialysis before and after direct cyclopexy. Arch Ophthalmol. 2008;126(9):1222-1225.
13. Ceruti P, Tosi R, Marchini G. Gas tamponade and cyclocryotherapy of a chronic cyclodialysis cleft. Br J Ophthalmol. 2009;93(3):414-416.
14. Yuen NSY, Hui SP, Woo DCF. New method of surgical repair for 360-degree cyclodialysis. J Cataract Refract Surg. 2006;32(1):13-17.