
The temporal clear corneal incision remains one of the most popular choices in cataract surgery.1 Although this step takes just a few seconds to complete, a well-constructed main incision sets the foundation for a successful cataract procedure and postoperative recovery. Understanding how the construction of this incision can go wrong assists with the prevention and management of the problem.
Back to Basics: The Ideal Incision
Before diving into the ways irregular incisions can occur, it is worth reviewing the fundamentals of creating an ideal incision. There are three main considerations.
Consideration No. 1: Where to place the incision around the circumference of the cornea. A temporal corneal incision has been shown to induce less astigmatism than a superior corneal incision.2 Surgeons may also elect to place the main incision along the steep axis of preoperative astigmatism to reduce postoperative astigmatism.
Consideration No. 2: Where to place the entry site of the incision. Limbal incisions are preferred because they have been shown to elicit a fibroblastic response that enhances wound stability and healing compared to incisions made entirely within the avascular clear cornea.3 Once initiated, the ideal incision tunnels through the corneal stroma to create a tunnel floor and roof of equal thickness (Figure 1A).
Consideration No. 3: Architecture. The length and width of the incision tunnel match, ideally, because square and nearly square incisions have been shown to seal well with minimal leakage (Figure 1B).4
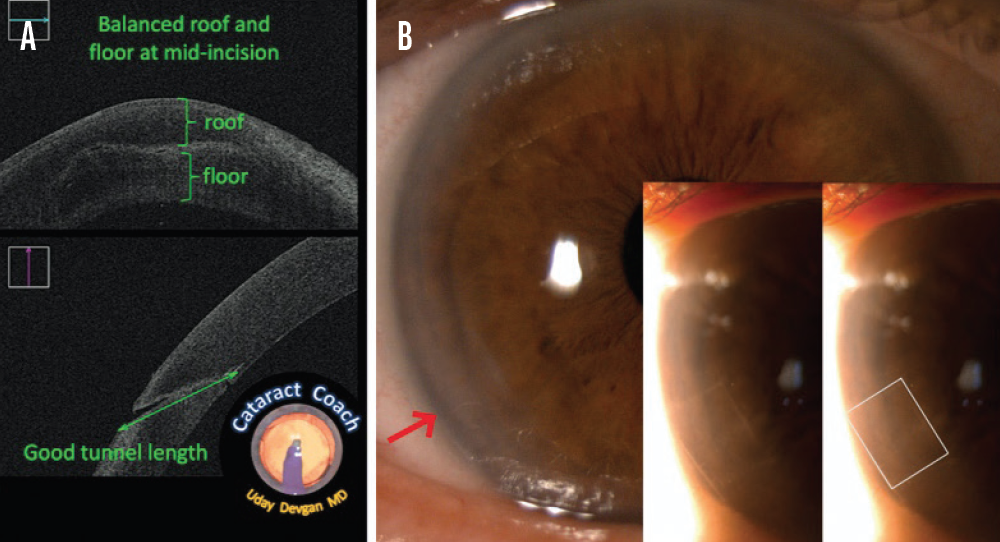
Figure 1. The ideal main incision. OCT shows that the roof and floor of the tunnel are of equal thickness (A). The entrance of the incision starts at the limbus (red arrow, B), and the length of the tunnel creates a nearly square incision (inset, B).
OCT images courtesy of Uday Devgan, MD; slit-lamp images courtesy of Joanne C. Wen, MD
IRREGULAR INCISIONS
Example No. 1: The location of the incision is too anterior. The ideal incision is initiated at the limbus. Some surgeons prefer to nick the limbal vessels lightly with the keratome entry to improve wound healing. Problems can arise if the location of the wound is too far anterior (Figure 2A).
Associated problems. Intraoperatively, the surgical view may be compromised, especially if significant hydration of the wound occurs. The incision may also induce a significant amount of astigmatism (Figure 2B). Moreover, when an incision is completely within the clear cornea, it can be difficult to achieve a watertight seal. Subsequent healing may be slow and impaired because of the avascularity of the tissue.
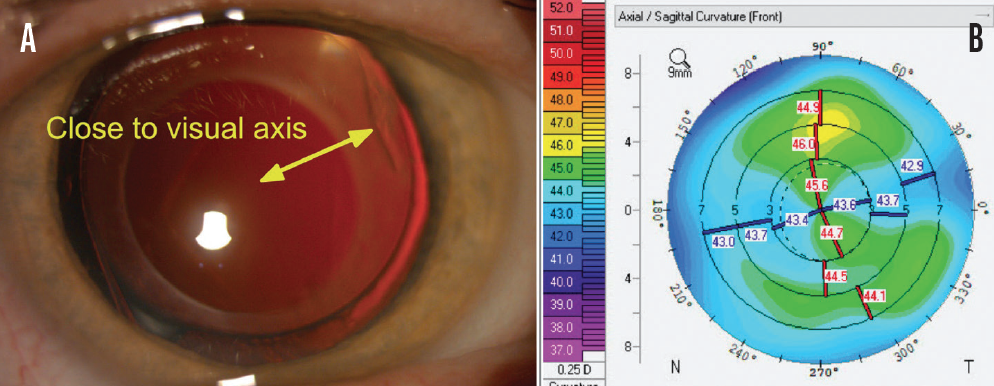
Figure 2. Example of an anterior incision. Note the proximity of the incision entrance to the center of the visual axis (yellow arrow, A). Corneal topography shows steepening 90º from the axis of the anterior incision. This patient had significant postoperative astigmatism (B).
Example No. 2: The location of the incision is too posterior. Creating the incision such that its location is too far posterior can disrupt conjunctival tissues.
Associated problems. Intraoperatively, the fluid egress from the main incision can flow into the subconjunctival space, leading to significant chemosis. This can cause fluid to pool over the cornea and affect the surgical view. Patients may also become increasingly uncomfortable as the chemosis grows. A snip incision through the conjunctiva may be required to drain the subconjunctival fluid. Given the proximity to the iris insertion, a posterior incision can also lead to significant iris prolapse throughout surgery (Figure 3).
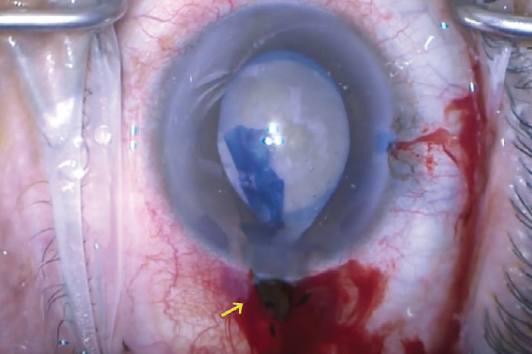
Figure 3. Example of a short, posterior incision that led to a significant subconjunctival hemorrhage and recurrent iris prolapse (yellow arrow). This wound was sutured closed, and a new, better-constructed incision was created superiorly.
Courtesy of CataractCoach.com
Example No. 3: The incision is too short. When the tunnel of the incision is too short, it can lead to a number of intraoperative issues.
Associated problems. The iris tissues can prolapse more easily through the incision (Figure 3). Moreover, the incision may not seal well around the phaco handpiece, and fluid egress may contribute to an unstable anterior chamber. At the end of surgery, the incision may not seal well, and suturing may be required to provide a watertight closure. Additionally, a short tunnel can have a greater astigmatic effect than anticipated.
Example No. 4: The incision is too long. Although long tunnel incisions resist leakage better than short tunnel incisions, an excessively long tunnel can cause a number of issues.
Associated problems. A long tunnel can lead to wound distortion and intraoperative corneal striae that can compromise the surgical view. If the duration of surgery is long, hydration of the wound may also compromise the surgical view. Further, a long tunnel creates a tight fit around the phaco handpiece and increases the risk of a wound burn, especially if the cataract is dense.
MANAGEMENT
The most important step in managing an irregular incision is to recognize it early. By understanding the principles underlying the ideal incision and identifying the features of an irregular incision (see Key Points), surgeons can avoid many of the subsequent complications. Once an irregular incision has been identified, the next step is fairly straightforward: Abandon the initial incision, suture it if necessary to create a watertight closure, and start over in a different location.
Key Points
- A well-sized, well-positioned main incision establishes the foundations for a successful cataract procedure.
- The early recognition of an irregular, poorly constructed incision can help to avoid subsequent complications.
- If an irregular main incision is identified, it should be closed, and the surgeon should start over in a different location.
1. Leaming DV. Practice styles and preferences of ASCRS members–2003 survey. J Cataract Refract Surg. 2004;30(4):892-900.
2. Park CY, Chuck RS, Channa P, Lim CY, Ahn BJ. The effect of corneal anterior surface eccentricity on astigmatism after cataract surgery. Ophthalmic Surg Lasers Imaging. 2011;42(5):408-415.
3. Ernest P, Tipperman R, Eagle R, et al. Is there a difference in incision healing based on location? J Cataract Refract Surg. 1998;24(4):482-486.
4. Masket S, Belani S. Proper wound construction to prevent short-term ocular hypotony after clear corneal incision cataract surgery. J Cataract Refract Surg. 2007;33(3):383-386.




