Shamik Bafna, MD: Over the past several years, the landscape of refractive surgery has begun to change. Now, in addition to LASIK and PRK, we can offer patients not only lens-based refractive surgical correction but also the relatively new, less-invasive option of small-incision lenticule extraction (SMILE). The purpose of today’s discussion is to share our experiences with refractive surgery in general and with SMILE specifically. We will also talk about our reasons for incorporating SMILE into our armamentariums and share our best practices with this novel procedure.
Dr. Rebenitsch, why don’t you start by telling us the top three reasons that you’ve chosen to incorporate the SMILE procedure into your refractive surgery practice.
R. Luke Rebenitsch, MD: The No. 1 reason I like SMILE is because it’s a gentle procedure. My patients hardly feel anything from the moment the procedure begins to the moment it ends. Second, the postoperative period is simple for patients. We have them follow the same postoperative drop regimen that we have patients follow after LASIK, but the amount of dry eye and irritation that my patients experience after SMILE is much less than what patients experience after LASIK. And finally, just the idea of having a stronger cornea—a very strong cornea—when we’re finished, was very appealing to us and to our patients. I could keep going, but those are the top three.
Dr. Bafna: Dr. Visco, what are the three things that have changed in your practice since incorporating SMILE?
Denise M. Visco, MD, MBA: I think the first thing that we changed in our practice is the way in which we talk to patients about laser vision correction surgery because we have more options for them. We talk more about avoiding dry eye, the safety of only having a pocket instead of a flap like in LASIK, and about a more rapid visual recovery than what patients might get with PRK. So, I think the conversation has changed, and it has gotten more valuable. Second, our marketing is different; we altered the way in which we present refractive surgery to our community. Our interest is in customized surgery for patients. All the procedures we have to offer are very good. Based on the patient exam and desired outcome, we can select the technology that delivers the best experience and outcome. Lastly, I think that SMILE has enhanced the excitement patients see in our practice. They can see how much the staff loves the SMILE procedure, in part because patients have a wonderful surgical experience, are more comfortable, and have an easier follow-up.
Gregory D. Parkhurst, MD, FACS: I want to echo Dr. Visco’s point. One of the most important things we do for our patients is to offer them options, and this is because, as we know, certain patients can benefit from certain procedures. For example, a 65-year-old with a cataract would not be a good candidate for laser vision correction; he or she would benefit more from a lens-based procedure. Likewise, in a presbyopic patient, we likely would not recommend SMILE. In my experience, it’s nice to have a menu of options that we can offer to patients. Certain patients, depending on their corneal health, their ocular surface, and their age, are definitely going to do better with SMILE. With that said, SMILE is one of the important procedures that we offer.
Dr. Bafna: Dr. Piracha, what are the top three things that you’ve changed in your refractive practice since incorporating the SMILE procedure?
Asim R. Piracha, MD: In my viewpoint, SMILE has provided us with an additional option, and as Dr. Parkhurst said, it’s nice to have a menu of options for our patients to be able to select something other than LASIK. Further, acquiring SMILE as another procedure that we can perform has broadened the scope of refractive surgery. In other words, more patients are now candidates for refractive surgery, including those with issues like dry eye or pseudoexfoliation as well as patients who are concerned about flaps and flap-related issues, trauma, and continuing to participate in athletic activities. In short, it’s nice to be able to offer SMILE as an additional option, especially to those patients who may not be ideal candidates for the LASIK procedure.
Dr. Bafna: I agree. At this time, the VisuMax femtosecond laser (Carl Zeiss Meditec) is the only laser that’s available to perform the SMILE procedure. In addition to using it for SMILE, the VisuMax is a fantastic flap maker. Dr. Piracha, what has been your experience with the VisuMax as a flap maker?
Dr. Piracha: We incorporated the VisuMax a year and a half before we started performing SMILE. In a very short time, we were impressed with the laser’s capabilities for making the LASIK flap. I think it provides patients with the most comfortable treatment, as compared with other femtosecond laser systems. So, from that aspect, having the VisuMax and using it as a flap maker has changed the patient experience. When patients are very comfortable and asking you when you’re going to get started (even though you already finished), as opposed to holding their breath until you stop making the flap, it can only be a positive change. It has been a real game changer for us in terms of patient experience and word-of-mouth referrals.
OPTIMIZING PREOPERATIVE DIAGNOSTICS
Dr. Bafna: Let’s talk about diagnostic steps, not just with SMILE, but with any type of refractive procedure. I think it’s crucial to obtain a good refraction in every refractive surgery patient, because, ultimately, we’re going to be treating that basic refraction. Dr. Visco, what do you feel are the key preoperative protocols you use in terms of optimizing the preciseness of your measurements?
Dr. Visco: First, when obtaining patients’ refraction, we make sure that they have their contact lenses out for a defined period of time prior to the refractive evaluation. Second, we look at the ocular surface and make sure that it’s optimized. If we don’t feel at the time of their examination that their ocular surface is pristine, then we will treat the ocular surface disease and have them come back after a specified amount of time. Also, we look at their meibomian gland function at their initial visit.
Dr. Piracha: I think the most important thing you can do is to hire an experienced refractionist. The second-most important thing is to be consistent with your refractions and make sure that your nomograms are consistent. Third, like Dr. Visco also mentioned, is to optimize the patient’s ocular surface prior to actually scheduling and performing the procedure.
Dr. Parkhurst: One thing that I want to add is that, when treating high myopes of around -8.00, -9.00, or -10.00 D, we do a contact lens over refraction to minimize the effect that comes with their deeper-set or prominent eyes. What we have found is that we are able to hit our target because we’ve had a more accurate preoperative refraction. So, that’s one thing we recently implemented to help us hit our target more often in higher myopes.
Dr. Bafna: I think that works well. The other thing that we oftentimes utilize is the use of the red/green chart in order to determine that you are not actually overminusing an individual. We found that the chart works extremely well from a refraction standpoint. Any other tools, techniques, or strategies to optimize diagnostics in this setting?
Dr. Rebenitsch: In addition to ensuring an optimal ocular surface, we get two topographies and a wavefront autorefraction on every patient. We found that this helps to determine if there is indeed astigmatism that we may be missing. We’ve also developed our own nomogram, which I think is very important in order to track your results in any refractive procedure. We pride ourselves in being a comprehensive refractive surgery center, and being able to track your outcomes over time and change your treatments accordingly is very important to optimization of patient satisfaction.
Dr. Piracha: In addition to what has been mentioned, we use the AcuTarget HD Analyzer (Visiometrics) to measure light scatter. I think it’s a helpful tool to determine the status of the ocular surface and also the optimum quality of the ocular system itself. It has been helpful for us to correlate that with the clinical exam.
Dr. Bafna: In my opinion, the HD Analyzer is probably one of the most critical diagnostic tools because, like you mentioned, it can objectively quantify the tear film. The other advantage to the HD Analyzer is its ocular scatter index (OSI). I think it’s been helpful from a lens perspective, in terms of trying to determine when it’s better to work on the cornea versus when it’s better to work on the lens. We tend to use that device to screen any patient who comes in, irrespective of whether they want LASIK or a lens procedure.
Dr. Visco: We also look at the angle kappa, because with the SMILE procedure, you want to make sure that the focus of the green light is on fixation. Sometimes that needs to be adjusted.
Dr. Bafna: That’s an excellent point, Dr. Visco. With regard to femtosecond LASIK flaps, they are created during the treatment, but it’s not the actual treatment. In the situation of SMILE, like you alluded to, the laser cut is actually your treatment, and so centration is extremely crucial. If there is an angle kappa, I know that when the patient is fixating during the laser dock, I have to make sure that the centration is perfect in order to try to get the best optimal results.
OPTIMIZE THE OCULAR SURFACE
Dr. Bafna: Let’s go back to discussing the ocular surface. Regardless of the refractive surgery procedure you are performing, optimizing the ocular surface is extremely important. Are there particular things that you have instituted, not just with SMILE, but in general in order to try to optimize the ocular surface?
Dr. Rebenitsch: We get a Placido-disc topography of every patient, and we use this to look for consistency of the mires. We also use the AcuTarget HD Analyzer to determine the OSI. Whenever there is any concern, we, of course, postpone surgery. We want to make sure that the patient’s refraction is absolutely ideal before progressing to surgery. In the case that the ocular surface is not healthy, we will treat it with Restasis (cyclosporine ophthalmic emulsion; Allergan), Xiidra (lifitegrast ophthalmic solution; Shire), steroids, and artificial tears and lubricants to make sure that we have the right refraction before we proceed. Postoperatively, in my experience, the presence of dry eye is reduced with SMILE than with some of the other procedures that we do. But, it’s just as important to optimize the ocular surface before SMILE as it is with any other procedure.
Dr. Piracha: To me, the biggest cause of not being a good candidate for laser refractive surgery is dry eyes. Other considerations that come into play in our decision-making process are thin corneas and irregular astigmatism, but dry eyes always seem to be the No. 1 reason why patients are not good candidates. This is the demographic in which SMILE has been extremely helpful. If the patient is borderline, I can do SMILE and feel comfortable about it. However, I might not have recommended LASIK for that same patient. Optimizing the surface is important, but also, I think more patients are candidates for refractive surgery now with SMILE versus LASIK.
Dr. Visco: I had a patient who was reluctant to undergo refractive surgery because he has very severe seasonal allergies. During his allergy episodes, he takes a lot of antihistamines, which would trigger extreme dry eye. He was particularly interested in the SMILE procedure. With a refraction of about -1.50 D, he was an ideal candidate, so we did the procedure and he is thrilled with his results. His ocular surface is great, and he has no symptoms of dry eye. It was really a gratifying feeling to know that we’re not going to make his situation any worse than he normally experiences when he gets his seasonal issues.
Dr. Bafna: I know you talk about the benefits of SMILE in patients with dry eye, but in your mind Greg, how does it minimize the impact as far as dry eyes is concerned?
Dr. Parkhurst: I agree with all that has been said about the diagnostic tools everyone uses. But we also do osmolarity analysis (TearLab Osmolarity System; TearLab) on patients to help us diagnose any abnormality in their osmolarity. We have also been using the LipiScan (formerly TearScience; now Johnson & Johnson Vision), which in contact lens wearers helps us to document any damage to their meibomian glands. By getting that preoperative test and demonstrating the damage their contact lenses are causing, it works as a conversion tool with the patient. Seeing these results may help them not only in preparation for what they need to do at home to reverse the damage, but it helps us drive adoption to a laser vision correction procedure like SMILE.
Dr. Bafna: Whenever you can incorporate tools like the LipiScan or the HD Analyzer that allow you to objectively demonstrate to your patients the quality of their ocular surface, it is a win-win situation. All of a sudden, it’s different than me just verbally telling the patient, “Your eyes are dry.” They can see the metrics, and then postoperatively, it’s so much easier for them to see and understand where they are at.
I almost find that patients are more apt to go ahead and use the treatments we are prescribing, because they want their scores to improve as much as possible. The impact of reduced dry eyes on vision directly correlates to patient satisfaction. From my perspective, if an ocular surface disorder is diagnosed beforehand, then it’s the patient’s fault. But if it’s something that is not communicated with the patient until after surgery, then it’s the surgeon’s fault at that point in time.
LEARN THROUGH EXAMPLES
Dr. Bafna: Let’s talk about a specific case that I had recently. A 34-year-old woman with rheumatoid arthritis (RA) who works at Home Depot was interested in refractive surgery. Her RA was well controlled with Arthrotec (iclofenac sodium/misoprostol; Pfizer) and Nexium (esomeprazole magnesium; AstraZeneca), but she was unable to wear soft contact lenses due to the irritation they caused. As far as her refraction, she had a moderate amount of myopia (about -5.00 D) in both eyes. Her pachymetry values were reasonable, about 535 µm in both eyes, and keratometry values were fairly unremarkable at +42.14 +43.11 @ 111º OD and +43.01 +43.68 @ 64º OS. From a diagnostic standpoint, the Pentacam (Oculus Optikgeräte) examination was fairly unremarkable as far as the tomography is concerned (Figure 1). We also did a topography, and once again it showed a fairly symmetrical pattern (Figure 1), with nothing standing out that would indicate she was a poor candidate for LASIK. But her OSI on the HD Analyzer revealed a lot of scatter (Figure 2). As you would expect in a patient with RA, this patient had very significant dry eye disease. So what are her options, and what would you discuss with her at the initial consult?
Case Example 1
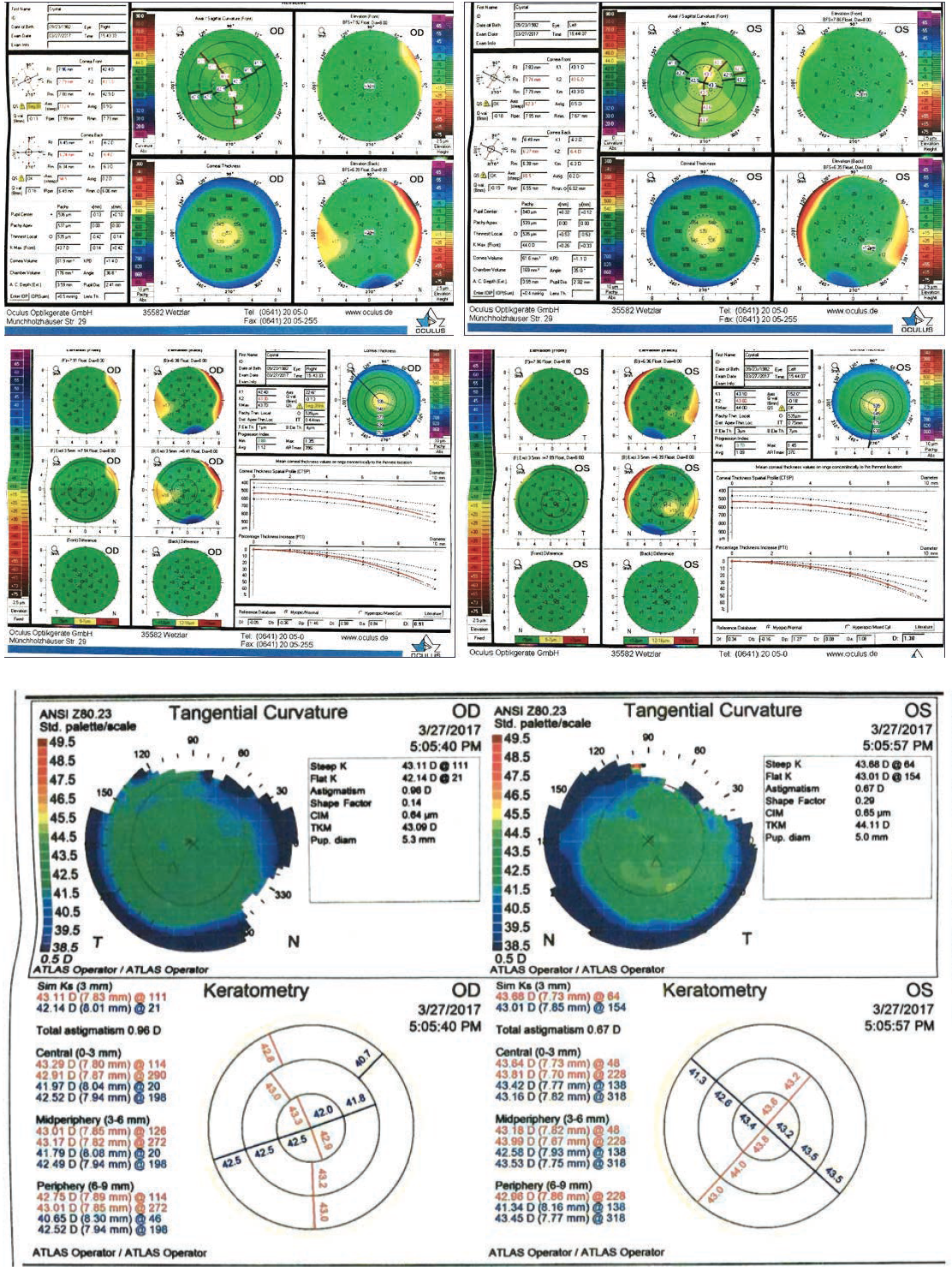
Figure 1. Preoperative examination with fairly unremarkable tomography (top four maps) and topography (bottom four maps).
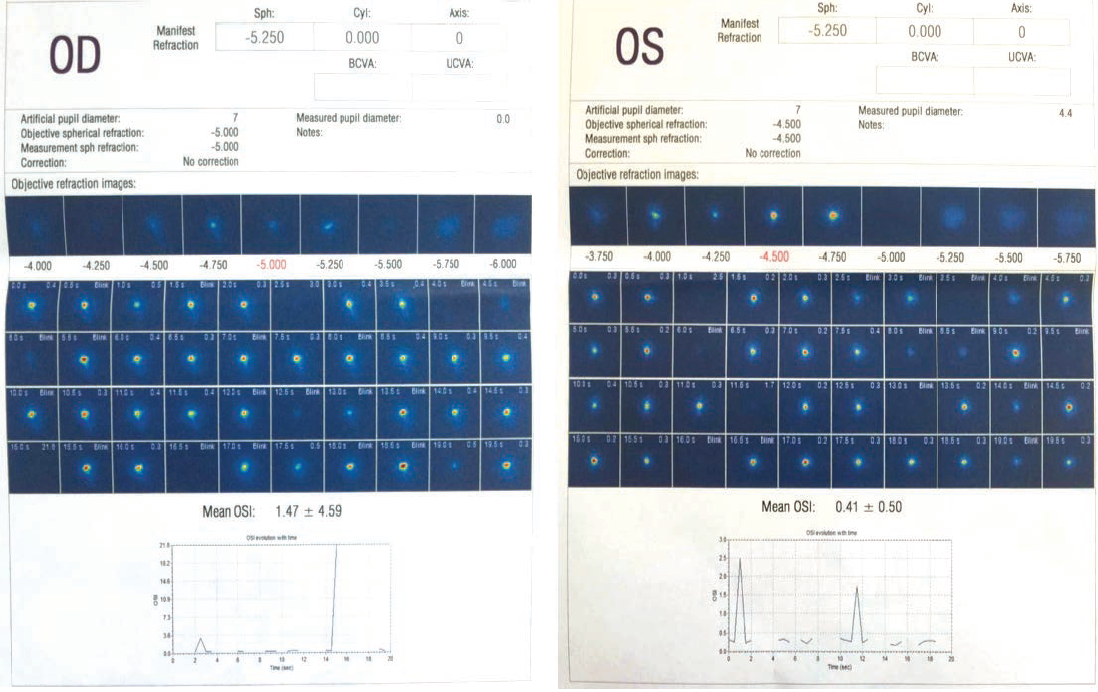
Figure 2. The HD Analyzer revealed a lot of scatter in both eyes.
Dr. Rebenitsch: Deferring refractive surgery is never a bad option. It sounds like she’s a motivated patient, and we want to make sure that we do the right thing for her. If I felt that the patient’s refraction was acceptable, and that her dry eyes were not significant enough to affect the preoperative measurements, I think that proceeding with surgery would make sense. I wouldn’t proceed with LASIK; PRK maybe, but SMILE would be the ideal procedure in this case. What we’ve found in our experience is that, at 6 months postoperative, LASIK and SMILE have approximately the same incidence of dry eyes, which is very minimal, but in the preceding months you have a much happier patient and an overall better outcome with SMILE.
Dr. Parkhurst: In this patient, I would avoid PRK because there is not a good expectation of a positive wound response.
Dr. Bafna: That is true. There is too much variability from a wound-healing standpoint to consider PRK.
Dr. Parkhurst: The only other consideration I would add to the list is anterior chamber depth. Assuming this patient has a deep anterior chamber, I might think about a phakic IOL. Ultimately, my decision would come down to SMILE or a phakic IOL.
Dr. Visco: I would also have a concern doing a surface ablation procedure on someone with RA. The fact that she’s under good control, I think, would help me to choose SMILE for her as opposed to deferring refractive surgery.
Dr. Piracha: First, I’d be aggressive with the level of medications she can tolerate. If there are still any dry eye findings, I’d be cautious about doing corneal refractive surgery in general, especially since the future is not really known. She may be stable now, but her RA could get worse over time—and we all know that can happen. So, if the patient is not well-controlled while on medications, I would defer laser refractive surgery and opt for a phakic IOL.
Dr. Bafna: Dr. Piracha brings up an important point. The key is optimization of the ocular surface, and so in this patient we went ahead and started her on Xiidra, artificial tears, and omega 3s, and we reassessed the ocular surface over time. In the long run, there is nothing wrong with waiting to perform surgery. In fact, it can be advantageous, because it can help ensure that the measurements are similar over time. When we realized that they were remaining consistent, we decided to proceed with SMILE.
So on day 1 postoperatively, her bilateral BCVA was 20/20. (One thing to point out is that, with LASIK, patients generally do extremely well on the day 1 visit. But at around 1 week, it is common to see some superficial punctate keratitis (SPK) or irritation. This can happen because, since patients are doing great, they don’t use their artificial tears frequently enough. I have found a distinct difference in terms of how often I find SPK or irritation after SMILE compared with LASIK, with it happening less frequently after SMILE. Patients who have undergone SMILE are extremely comfortable.) In this particular patient, at about 3 months postoperatively, her BCVA was 20/15 bilaterally, and she was extremely happy.
This case was a definite situation in which proceeding with something like LASIK or PRK may not have ended as well.
Dr. Rebenitsch: Can I make a comment? There’s a large retrospective study out of the United Kingdom1 that showed LASIK was safe in patients who were under control for RA and other autoimmune diseases. I think it can be inferred from this study that SMILE would be okay in these patients as well.
Dr. Bafna: Great point, Dr. Rebenitsch. Various studies about corneal sensitivity have been performed, comparing SMILE versus LASIK (Figure 3).1 According to the results of these studies, with both procedures, there is an overall reduction of corneal sensitivity; however, that reduction is much lower after SMILE than it is after LASIK. Additionally, patients tend to bounce back to their baselines much more rapidly with SMILE as opposed to LASIK. Even up to 1 year out, the LASIK patients have not quite gotten to the same baseline level sensitivity as the SMILE patients. They will get there, but it will take more time. So, both procedures do affect the ocular surface, and both can cause dry eye, but the rapidity by which the patient rebounds from the symptoms is much quicker with SMILE.
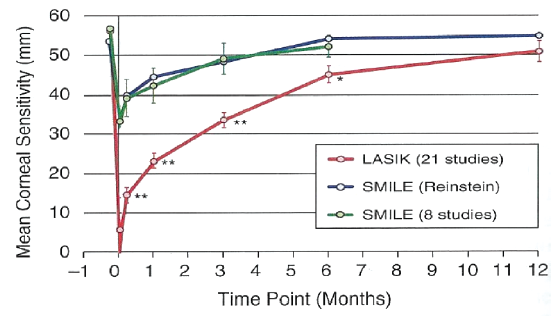
Figure 3. Tensile strength in SMILE (blue and green) and in LASIK (red).
Dr. Parkhurst: Many of the nerves on the surface of the cornea come in from nasal and temporal. Specifically in the case of SMILE where we are making a superior incision, we are able to bypass more of those nerves by coming from the vertical meridian. Based on that, you are disrupting less innervation by making a SMILE incision than you are by making a LASIK flap.
Dr. Piracha: Absolutely. The smaller incision in SMILE versus a LASIK flap makes a huge difference.
Dr. Bafna: I think that’s part of reason why people experience decreased corneal sensitivity after refractive surgery. However, if you do perform SMILE, there will be less loss of corneal sensitivity as compared with LASIK. The overall advantages of SMILE, in my mind, are that it is biomechanically more stable than LASIK, it has the potential for less dry eyes, and that it eliminates the concern for flap-related risks.
Let’s discuss another case. A 35-year-old man employed as an account manager for an HBAC company came to our practice inquiring about refractive surgery. His past medical history was unremarkable, and he was used to wearing soft contact lenses. On refraction, he had a moderate to high level of myopia (-6.25 D in the right eye, -6.75 D in the left). But what stood out was that pachymetry was around 486 µm in the right eye and 493 µm in the left. Keratometry was fairly unremarkable, at +44.37 +46.95 @ 88º OD and +46.38 +47.08 @ 81º OS, and he had a fairly symmetrical corneal tomography (Figure 4) and topography (Figure 4).
Case Example 2
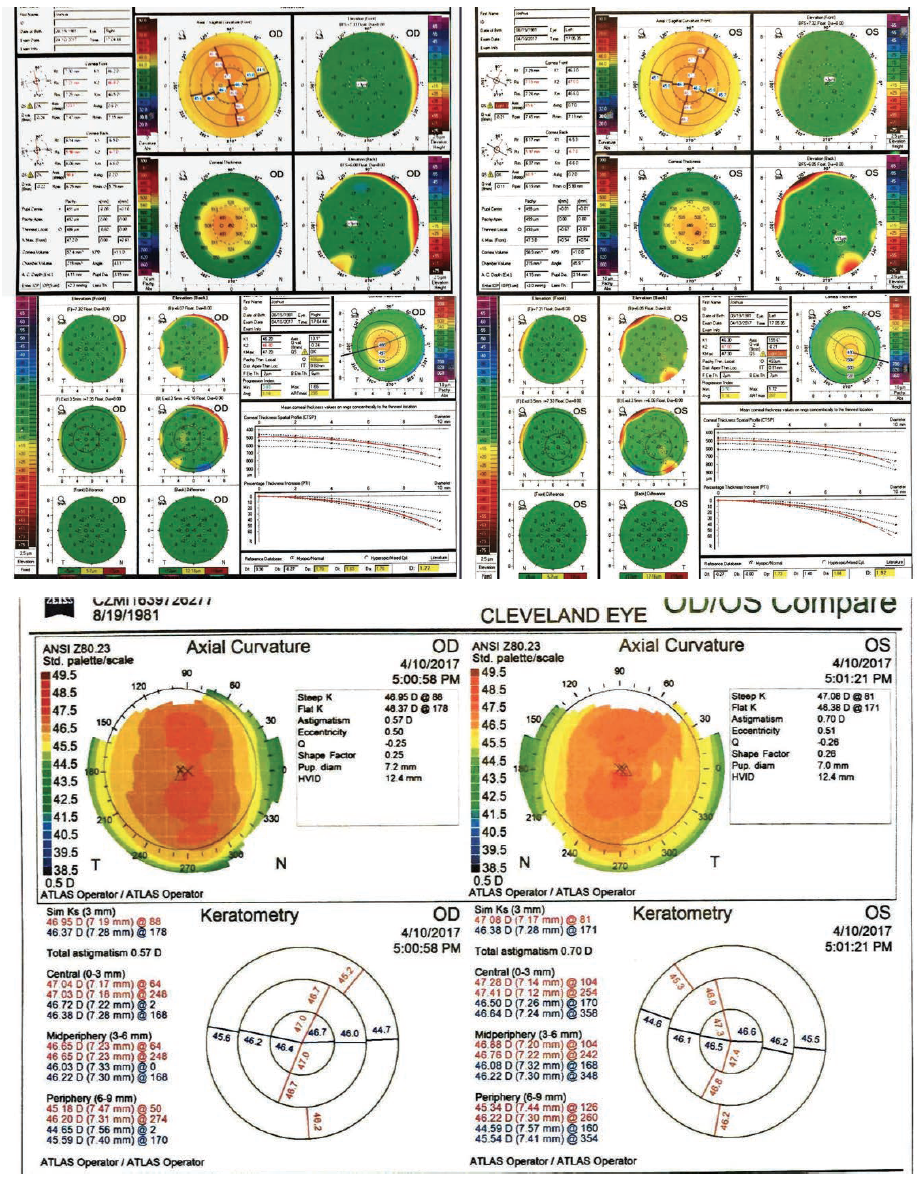
Figure 4. Preoperative examination with fairly unremarkable tomography (top four maps) and topography (bottom four maps).
I’m going to add one more comment before I ask what you would have done in this patient, and that is, in general, if someone has less than 500 µm of tissue and they’re biomechanically stable, we tend to go more toward surface ablation as opposed to LASIK. But another choice in this case is bilateral SMILE, and a third option, which Dr. Parkhurst mentioned earlier, is a phakic IOL, depending upon the anterior chamber depth.
Dr. Visco: At least for me, for this patient, even with the normal topography, his pachymetry is out of my comfort zone. I would probably not do a corneal procedure. I would defer corneal surgery and look at an implantable contact lens option.
Dr. Piracha: I wouldn’t be totally confident in SMILE yet because of the deeper residual stromal thickness. Likewise, LASIK requires 50 µm more stroma. So I personally would go with bilateral surface ablation. PRK, in my mind, is still a little safer option. At the patient’s age of 35, I’m not as worried about progression or ectasia, and therefore I think surface ablation may be a little bit safer in this case.
Dr. Rebenitsch: I would argue, at least in theory, that SMILE could leave the cornea biomechanically more stable than PRK, because the anterior fibers are left intact. I think a phakic IOL is a wonderful option. I’m also of the philosophy that a thinner cornea does not, by definition, make it an abnormal cornea. I wouldn’t be excited about doing LASIK in this case, but I would have no problem doing SMILE.
Dr. Bafna: If you look at some of the work that Dan Z. Reinstein, MD, MA(Cantab), FRCSC, DABO, FRCOphth, FEBO, has done out of the United Kingdom,2,3 the strength of the anterior stromal fibers is greater than the posterior stroma itself. And so, in general, the total stromal tensile strength is higher with SMILE than it is with LASIK. Dr. Reinstein has done some biomechanical analyses with Willian J. Dupps, MD, MS, PhD, in Cleveland. They have found that, from a biomechanical perspective, SMILE leaves the cornea stronger than even PRK. More studies are coming out to support this finding. I think that such evidence is financing a paradigm shift, from a mindset of working on the surface in questionable cases to perhaps considering SMILE. In general, SMILE tends to leave the cornea stronger than other procedures.
So in this case, we went ahead and performed SMILE. The patient did extremely well, and just like the last case I presented, he was 20/20 in both eyes. At 1 month, he was still 20/20 bilateral. Again, this is a case where ultimately you’re not going to know what the right decision was, from a biomechanical standpoint, until a few years down the road, but that’s why it’s called the art of medicine.
Dr. Piracha: Plus with other options such as crosslinking and also Intacs (Addition Technology), you know that you can take care of that patient long term, and you can inform him or her that there are other options available if something should happen in the long term. So I feel more comfortable today offering advanced surface ablation and SMILE than I would have, say, 5 years ago.
TALKING POINTS
Dr. Bafna: Let’s shift gears and talk about the most effective talking points to share with prospective SMILE patients. Dr. Visco, what do you make sure to communicate to patients during the consultation?
Dr. Visco: The first talking point that we have in our practice is that we call the procedure a small-incision, LASIK-like experience, because I think patients can easily understand that. They know what LASIK is, and they also understand what small incision means. So, smaller incision to them means that their eye will not be as scratchy for as long as it is with LASIK. And it also potentially implies that the procedure might be safer because the incision is not as large.
Dr. Bafna: That’s a great analogy. We use the term laparoscopic a lot of times for the same reasons. It resonates with the patient.
Dr. Visco: Another thing we do when describing the anatomy of the procedure is that we describe the incision as a pocket instead of a flap. We have found they better grasp this terminology as well—the surgery is done internally, inside a pocket, as opposed to lifting a flap and exposing the inner cornea. So I think that simplifying the concepts for patients is really useful in having a productive conversation about SMILE.
Dr. Piracha: As a comprehensive refractive surgery practice, we aim to offer all the best technologies to our patients. Our approach is that external marketing will bring patients in for evaluations, but once they are there, we feel confident that we have all the options available to provide the best treatment for each individual, whether that be a custom corneal treatment versus SMILE versus PRK. This allows us to choose the right procedure for each individual.
With that said, we do not say that one procedure is better than the other. Rather, we convey that one procedure may be better for that individual than another. LASIK is still a fantastic procedure today, and I had LASIK about 20 years ago and it was a fantastic procedure then. But now SMILE is another fantastic option we have to offer patients, and we think it is important to choose the procedure that’s best for each individual.
Dr. Rebenitsch: In my practice, we have tried to get away from using the term incision when talking to patients. Instead we say it’s a very small opening. To us physicians, the distinction in terminology doesn’t really matter, but to our patients, the word opening sounds a lot more gentle than incision.
Dr. Bafna: I like that word. That’s a good call—or as Dr. Visco said using the word pocket.
Dr. Parkhurst: SMILE fits with our brand, which revolves around the premise that refractive surgery is about patient benefit rather than individual technology. But I think that’s one of the big things that the refractive surgery specialty needs collectively moving forward; we should not talk about technology—like iDesign (Johnson & Johnson Vision) or Contoura (Alcon)—anymore but just about the benefits of getting your vision corrected. And so, again, having all the tools in our toolbox so that we can select the right procedure for the patient fits the way we’ve been doing things. SMILE is an important part of that. I feel like we would have had a hole in our toolbox if we didn’t have SMILE.
Dr. Visco: I agree. As opposed to specifically marketing one procedure to the public, we market refractive surgery and laser vision correction as a whole product, with SMILE being one of the many procedures we have to offer.
Dr. Bafna: Ultimately, the goal of our patients is always improvement in vision, regardless of the methodology. The bottom line is that they are coming to you and asking for your advice on what you feel is the most appropriate vision correction surgery procedure for them. I agree that we shouldn’t be marketing this procedure or that procedure, but rather marketing refractive surgery and vision correction as a whole. The message that we need to share with patients is, “I’m going to go ahead and help you to achieve what it is you want to achieve. We’ve got all these tools in our toolbox, and we are going to select the most appropriate tool for you.”
THE REFRACTIVE SURGERY MARKET
Dr. Bafna: Dr. Parkhurst, from your perspective, what are some of the top reasons why refractive surgery hasn’t grown over the past few decades as we had hoped? I know you’re strongly involved with the Refractive Surgery Alliance (RSA), so from that perspective what do you feel are some of the main factors in play?
Dr. Parkhurst: There are several factors. But the good news is that 2017 was different. Laser vision correction was up by 20% in many RSA practices around the country.4 So something’s happening to move the market, and I think that SMILE is part of that, I think messaging is part of that, and I think learning from past mistakes is part of that. I think one of the fundamental reasons that the refractive surgery market hasn’t grown too much prior to last year is actually bad messaging and marketing. We’ve had great procedures, but we haven’t done a good job communicating it to the public. There are also optometric barriers that we’re trying to break down. There are many, many things. But the good news is that change is happening, and we’re seeing it now.
Dr. Bafna: Dr. Piracha, do you feel that SMILE is helping to eliminate the barriers to refractive surgery and helping patients make the decision to undergo refractive surgery?
Dr. Piracha: The two big barriers we always hear about are fear and cost. The price of SMILE and of LASIK is pretty much the same. Patients may have fear of LASIK because of some of the stories they’ve heard in the past, and they may be more open and willing to have SMILE. Maybe it sounds less scary to them to not have the flap. So that, to me, has addressed the fear issue that some patients may have, holding them back from proceeding.
Dr. Visco: During the economic downturn in 2007/2008, the floor kind of fell out from under the refractive surgery market. And so now, slowly, consumer confidence is building back up. We have momentum, and we also have the people, the millennials, our potential patients. The LASIK market is mature at this point, but with the introduction of SMILE we have a new driver—just like we did back in the early days of LASIK in 2004/2005—that is helping to bring people into the practice. But, in a mature market, our old messaging doesn’t work anymore. The marketing strategy has to be different. SMILE is not mature. SMILE is new. So, we’re going through another cycle.
Dr. Bafna: I think a lot of people wonder about cannibalizing the LASIK market by incorporating SMILE. From my perspective, the number of LASIK procedures is remaining constant. It is almost as if a new subset of patients is being created by SMILE.
Dr. Rebenitsch: Marketing is an art, and I think that we’ve become much better at it by becoming more positive. The RSA has helped to develop marketing guidelines, and we believe that has helped us improve our refractive surgery numbers. SMILE also helps, because it’s made it easier for patients and for physicians. Again, happier patients grow the market.
THE FUTURE
Dr. Bafna: Are there any upcoming technological developments with SMILE that you guys are excited about? I know in the United States we are excited about astigmatism treatments. As I understand, those data will be submitted to the FDA in the first quarter of 2018. Internationally there are a few other things that we’re aware of that may be coming down the pipeline.
Dr. Rebenitsch: Hyperopia will also be an important indication for SMILE. If you look at Reinstein’s work,2,3 the idea is that hyperopic SMILE has a larger optical zone than hyperopic LASIK, and so it could expand the indications beyond what we can treat now with LASIK. The results are promising, and I really hope they are as good as we think.
Dr. Parkhurst: A lot of places around the world are making two small side incisions instead of one larger one. So, I think that’s going to be an advantage. I think there’s a pretty big future for SMILE.
Dr. Bafna: Exactly, especially within the United States. Even though SMILE is an approved procedure, what we can use it for is a little bit different than what the surgeons outside the United States can do. Even with what we’ve got at this point in time, SMILE is definitely a procedure that can deliver fantastic outcomes, great results, and a pleasant surgical experience for our patients.
I’d like to thank our panelists for joining us today for this lively discussion. We are all eager to see what the future holds for refractive surgery, in general, and for SMILE, specifically.
1. Schallhorn, J, et al. Outcomes and complications of excimer laser surgery in patients with collagen vascular and other immune-mediated inflammatory diseases. J Cataract Refract Surg. 2016;42:1742–1752.
2. Reinstein DZR, Archer TJ, Gobbe M. Small incision lenticule extraction (SMILE) history, fundamentals of a new refractive surgery technique and clinical outcomes. Eye Vis (Lond). 2014;1:3.
3. Reinstein DZR, Archer TJ, Randleman JB. Mathematical model to compare the relative tensile strength of the cornea after PRK, LASIK, and small incision lenticule extraction. J Refract Surg. 2013;29(7):454-460.
4. Parkhurst G. SMILE: Another opportunity to make LVC great again. https://crstoday.com/articles/2017-nov-dec/smile-another-opportunity-to-make-lvc-great/. Accessed February 20, 2018.







