
Vitreous floaters are a common result of age-related vitreous syneresis, or liquefaction, and are often associated with posterior vitreous detachment (PVD). Occasionally, floaters are associated with potentially blinding pathology, such as retinal tear, retinal detachment, vitreous hemorrhage, or inflammation.
With our daily focus on treating sight-threatening diseases, it can be easy to overlook how symptomatic floaters without ocular pathology impact our patients’ quality of life. Indeed, studies have shown that select patients can be significantly impacted by their floaters and are willing to trade some of their remaining years for resolution.1
As a retinal specialist, I see many patients afflicted by floaters. It is often difficult to satisfy patients when counseling them about their symptomatic floaters. We usually recommend observation and encourage neural adaptation, which does not work for every patient. Vitrectomy is an extremely effective way to remove floaters, but there are potential risks, including infection or retinal detachment, that could permanently compromise vision. Could YAG vitreolysis serve as an intermediary option, with potentially lower efficacy compared to vitrectomy but also potentially lower risk?
When I was asked to deliver a presentation in 2012 about floaters, I requested to speak about “real disease,” like age-related macular degeneration or diabetic retinopathy. Reluctantly accepting the proposed topic, I began researching floaters and realized that there was minimal research on the topic. Small-gauge vitrectomy was effective, but not ideal in phakic patients given the guaranteed risk of cataract. Also, there was up to a 10.9% risk of retinal detachment postoperatively.2 The data on YAG vitreolysis were very limited, contributing to its controversy in the ophthalmology community. Further, it had evolved in an unconventional way: a handful of people were performing it commercially, but without the necessary clinical trial data.
Given the impact of floaters on our patients’ quality of life and the dearth of effective treatments, YAG vitreolysis seemed ripe for investigation. My colleague Jeffrey Heier, MD, and I decided to design a prospective randomized controlled clinical trial to determine whether there was merit in this procedure.
Looking Into YAG Vitreolysis
Most ophthalmologists have not performed YAG vitreolysis because of the lack of data, potential risks, and lack of formal training in residency programs. I had never performed YAG vitreolysis before our pilot study. I practiced on a model eye and got tips from colleagues who had performed the procedure.
In our clinical trial, we dilated the pupil and applied proparacaine. I applied an Ocular Karickhoff 21 mm Vitreous Lens with goniosol, and then I administered the laser (Ultra Q Reflex; Ellex) to vaporize the Weiss ring and other significant floaters. I set the energy at 3 mJ and titrated to a level where I visualized gas bubbles, indicative of plasma formation. The number of laser pulses required to achieve this goal varied.
The procedure took some practice. I started with pseudophakic eyes for five cases until I became more comfortable with the visualization and focus. YAG vitreolysis is different than lasering other stationary ocular tissues such as the retina or iris, as the floater will move in three dimensions, requiring careful refocusing as one is lining up each shot.
First Clinical Trial
In the clinical trial, funded by the Center for Eye Research and Education, we selected 52 patients who had a symptomatic Weiss ring floater for more than 6 months.3 Patients were excluded if they had no PVD or if they had retinal tear, retinal detachment, uveitis, glaucoma, aphakia, cystoid macular edema, retinal vein occlusion, diabetic retinopathy, or a Weiss ring less than 3 mm from the retina or less than 5 mm from the crystalline lens (measured by B-scan ultrasound). The mean age was 61, most patients were women, and about three-quarters were phakic.
Patients were randomized 2:1 to one YAG vitreolysis session or sham laser treatment via filtered lens (36 patients and 16 patients, respectively). For the sham group, we used an Ocular Karickhoff 21 mm Vitreous Lens covered with a lens filter to block the YAG energy, which was delivered at the laser’s lowest setting. The patient could see the aiming beam and hear the clicking of the laser, but no energy reached the eye.
For the YAG vitreolysis procedure, we used the laser with a goal of vaporizing the Weiss ring and other floaters in the visual axis. There was some degree of fractionation and lysing of vitreous adhesions that allowed particles to drift peripherally. The mean was 218 shots (range 33-763), up to 7 mJ/shot, compared to sham, which was 150 shots (range 67-218), 0.3 mJ/shot.
In 6 months of follow-up, patients with YAG vitreolysis experienced no retinal tears, retinal detachments, elevated IOP, or other significant adverse events. One posterior chamber intraocular lens was pitted peripherally, similar to that seen with YAG capsulotomy, but it was not visually significant, and there was a retinal tear through lattice in a sham patient.
Patients treated with YAG vitreolysis reported a mean of 54% subjective improvement at 6 months, compared to 9% in the sham group. Visual disturbance scores for the YAG patients showed significant improvement (Figure 1). On a scale from 0 (no floaters) to 10 (debilitating floaters), the YAG group’s median score improved from 6.4 to 3.3, while sham patients were unchanged. Using a 5-level scale, 53% of YAG patients said they had complete resolution or significantly better symptoms, whereas no sham patients rated their results that highly (Figure 2). Compared to sham patients using the Visual Functioning Questionnaire-25, YAG patients had better general and peripheral vision, with less role difficulties and dependency on others. There was no change in visual acuity for either group.
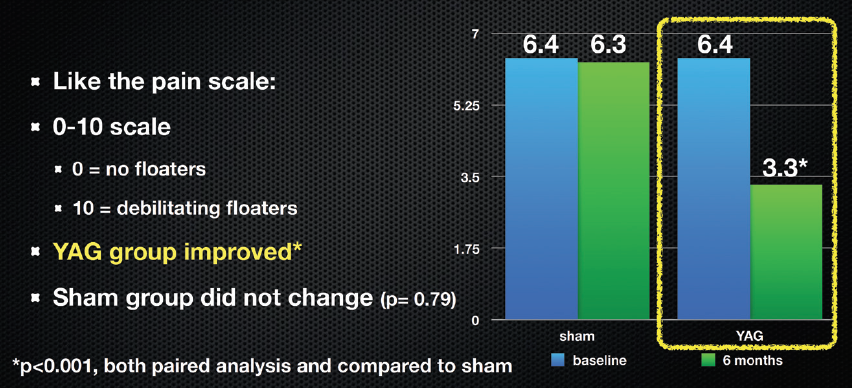
Figure 1. Visual disturbance score.
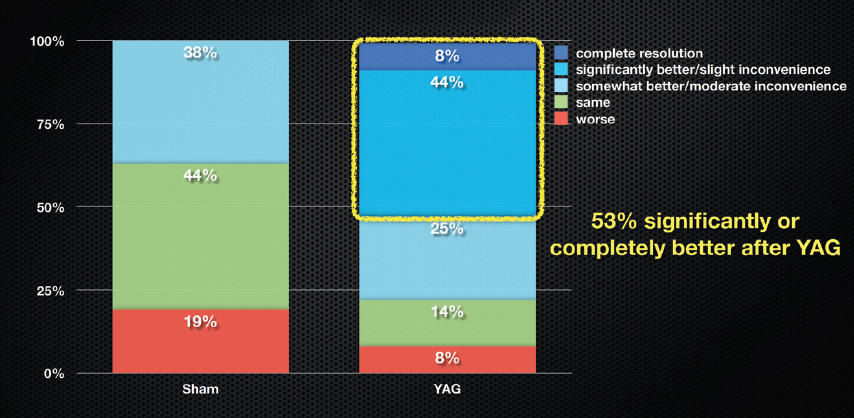
Figure 2. 5-level scale at 6 months.
Objectively, a masked investigator graded color photography of all eyes before and after treatment. The investigator found there was no change in floater appearance in the sham group, while 94% of YAG eyes were significantly or completely better after the procedure.
Subjective vs. Objective Results
The results of this pilot study show clinically significant outcomes from YAG vitreolyisis, but there was a sizeable discrepancy between subjective and objective outcomes. Why did only 53% of patients say their symptoms were significantly or completely improved, while 94% of eyes showed objective improvement in floater appearance (Figure 3)? Moreover, in the YAG group, 8 of 36 patients reported 0% subjective improvement, while objective comparison showed 7 of those same 8 patients had significant or complete improvement of floaters.
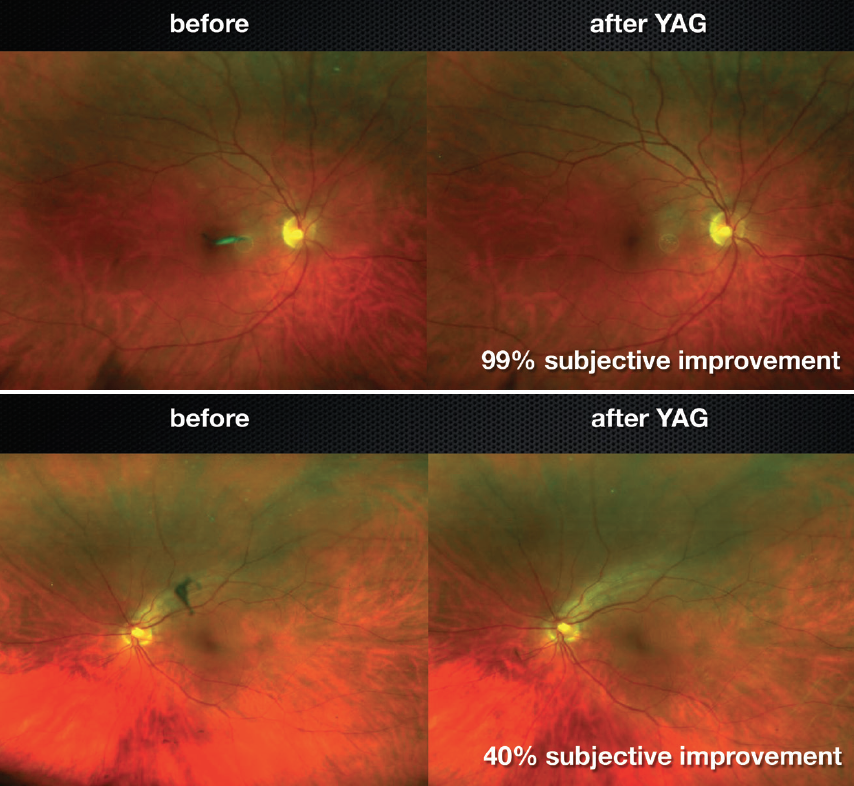
Figure 3. Both of these eyes had good objective improvement of their floaters; however, patients’ subjective evaluation of their improvement did not always match the objective result.
Although we do not know for certain why this discrepancy exists, we developed a few hypotheses. I might not have managed expectations appropriately. A related problem could be that some patients may have high visual demands and unrealistic expectations. Some people are simply more bothered by floaters than others. The natural extension of that dissatisfaction could be low satisfaction with a procedure that does not deliver complete relief from floaters.
It is possible that even when YAG vitreolysis reduces floater appearance on color photos, patients remain bothered by other vitreous opacities not apparent on photographs. Finally, different types of floaters may respond differently to YAG vitreolysis. Though all of our patients had a Weiss ring, many had various additional vitreous opacities. We might find that subjective results are related to the specific type of floaters we treat.
Conclusions and Future Study
This first reported randomized controlled trial for YAG vitreolysis showed that a single session produced moderate improvement in symptoms and no retinal detachment in the 6-month follow-up period.
Weaknesses of the study include its small size, single-center model, and short follow-up. In addition, we only performed one YAG treatment session, rather than the two or three treatments doctors often perform in the real world to address residual floaters. We designed the study this way because if we had sham patients back for a second session, they would likely realize they were receiving sham laser, and thus the study would be unmasked. It is possible that we would see higher satisfaction if we were able to offer more than one treatment session. We also excluded eyes without PVD and Weiss rings, and thus the results are not applicable to other floater types.
To learn more about the potential benefits of YAG vitreolysis, we need to see larger multicenter studies that include a variety of floater types and follow patients for a longer duration. It would help its acceptance in the ophthalmic community if the procedure had a specific billing code for YAG vitreolysis of symptomatic floaters. It would be interesting to see YAG vitreolysis studied head-to-head with vitrectomy. I think it is likely that it would show that vitrectomy is the more effective treatment, but it carries a higher risk of complications, including infection, cataract, and retinal detachment.4 We did not see that level of risk with YAG vitreolysis in this small study. It is possible that once we accumulate more data, we could find that YAG vitreolysis to be a reasonable treatment option to fill the gap between observation and vitrectomy, perhaps improving symptoms enough to allow patients to avoid vitrectomy.
My colleagues and I are considering checking in with our study patients at 2 to 3 years post-treatment to see if the results endure and if there are any new adverse events. We are also considering a larger clinical trial. Our small pilot study has, fortunately, inspired further studies by others. Clinical trials evaluating YAG vitreolysis are ongoing in Japan, and ophthalmologists in Germany and France are planning to reproduce our prototype on a larger scale.
As we see more data over the next few years, I am hopeful that we can incorporate the data into a meta-analysis and draw more significant conclusions. This may contribute to a paradigm shift in how we approach and treat patients with floaters. We have been taught to dismiss the problem in the hopes patients will adapt, but we are entering an era where we appreciate how floaters affect quality of life, and we may find that we have a treatment that could benefit them in YAG vitreolysis.
Ultra Q Reflex is a trademark of Ellex. © Ellex 2018. All other brands/ products are the trademarks of their respective owners.
1. Zou H, Liu H, Xu X, Zhang X. The impact of persistent visually disabling vitreous floaters on health status utility values. Qual Life Res. 2013;22(6):1507-1514.
2. de Nie KF, Crama N, Tilanus MA, et al. Pars plana vitrectomy for disturbing primary vitreous floaters: clinical outcome and patient satisfaction. Graefes Arch Clin Exp Ophthalmol. 2013;251(5):1373-1382.
3. Shah CP, Heier JS. YAG laser vitreolysis vs sham YAG vitreolysis for symptomatic vitreous floaters: a randomized clinical trial. JAMA Ophthalmol. 2017;135(9):918-923.
4. Sommerville, DN. Vitrectomy for vitreous floaters: analysis of the benefits and risks. Curr Opin Ophthalmol. 2015;26:3:173-176.



