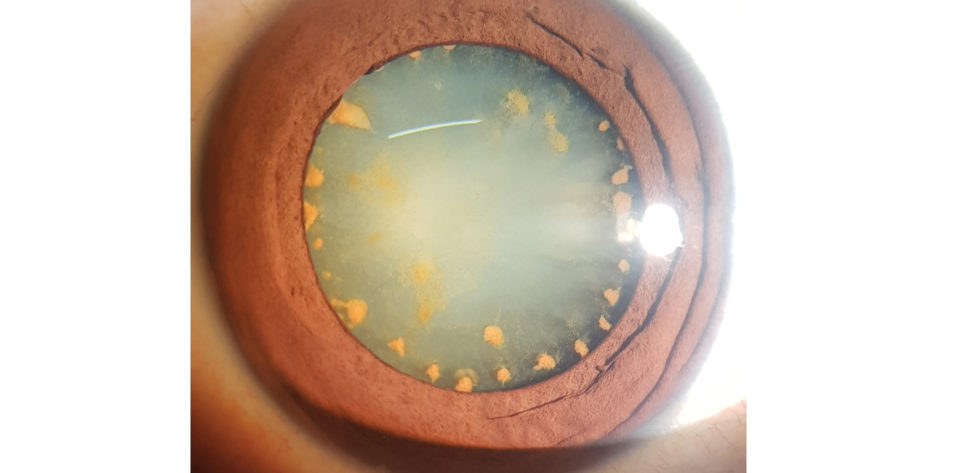
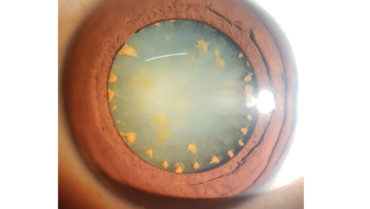
In 2018, a 17-year-old boy presented to the clinic with trauma to the left eye that occurred while he was cutting wood with an ax. On examination, his visual acuity was hand motion with good light projection in the left eye; +1 cells were observed in the anterior chamber, and reddish iris discoloration and a dense cataract with reddish rust deposits were also observed, suggestive of an intraocular foreign body (Figures 1–3). IOP was 14 mm Hg OS. The view of the fundus was hazy. Vitritis was evident on B-scan ultrasound. A posterior sub-Tenon steroid injection was administered. An x-ray of the orbit and ultrasound did not reveal a foreign body. The patient was treated with topical steroids and cycloplegics and later underwent cataract surgery with IOL implantation.
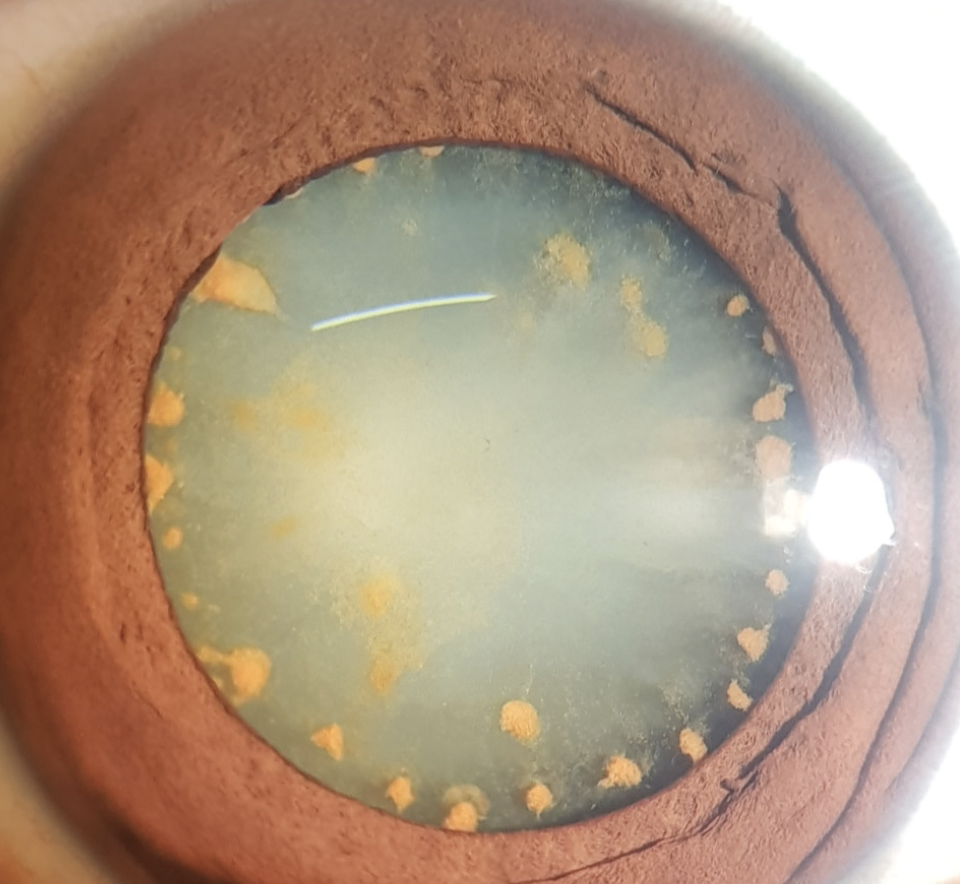
Figure 1. Diffuse slit-lamp illumination showing reddish iris discoloration and circumferential iron deposits on a cataractous lens.
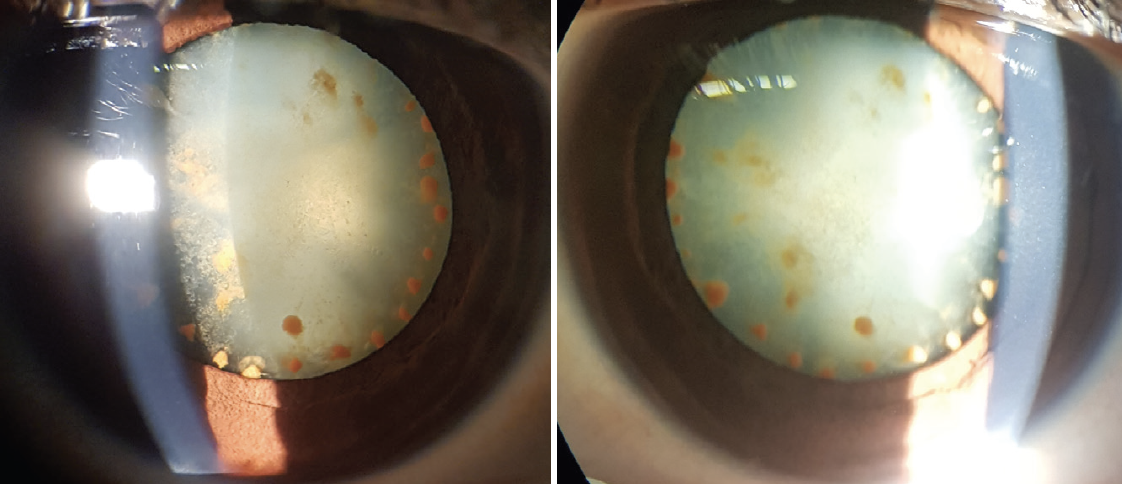
Figure 2. Oblique illumination showing the density of the cataract and highlighting the lenticular rusting.
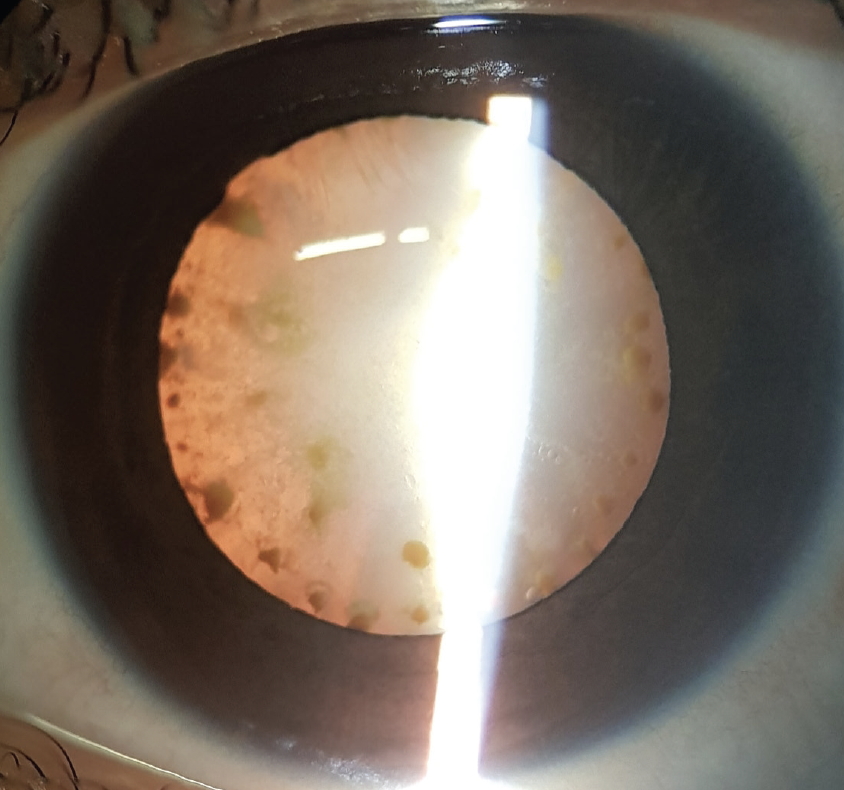
Figure 3. Retroillumination showing iron deposits against a good fundal glow.
At a recent follow-up examination, the anterior chamber of the left eye was quiet, the patient’s BCVA was 20/30 OS, and the IOP was 14 mm Hg OS. Trabecular meshwork hyperpigmentation and a mild epiretinal membrane were identified. The peripheral retina, however, showed glistening golden dots along with pigmentary changes and old vascular sheathing. An OCT scan of the retina in the left eye showed retinal nerve fiber layer thinning both superiorly and inferiorly and ganglion cell complex loss inferotemporally.
The patient is not currently administering any antiinflammatory drops and is satisfied with his care.
Conclusion
No iron foreign body was detected or localized. It is possible that the foreign body was minute and fully disintegrated. The patient’s symptoms were managed well with steroids.