Extended Depth of Focus Lens Implantation After Radial Keratotomy
Baartman BJ, Karpuk K, Eichhorn B, et al1
Industry support: Two of the authors received consultant and/or personal fees from various manufacturers while the study was conducted
ABSTRACT SUMMARY
This retrospective study evaluated the visual performance of 12 patients (24 eyes) with a history of radial keratotomy (RK) who underwent cataract surgery and the implantation of an extended depth of focus (EDOF) IOL (Tecnis Symfony, Johnson & Johnson Vision). IOL power calculations were performed using the Holladay II formula and keratometry values from the Lenstar (Haag-Streit). Intraoperative aberrometry was performed in all cases. Patients with glaucoma, macular disease, diabetic retinopathy, and corneal scarring and patients who received monofocal, toric, and multifocal IOLs were excluded.
Study in Brief
A retrospective chart review evaluated the performance of extended depth of focus (EDOF) IOLs in patients with cataracts and a history of radial keratotomy (RK). An elongated focal point and a broadened defocus curve may allow EDOF lenses to provide satisfactory UCVA to this population.
WHY IT MATTERS
It is notoriously difficult to calculate corneal power and estimate the effective lens position in post-RK eyes, and hyperopic refractive surprises after cataract surgery are not uncommon. As evidenced by their history of refractive surgery, however, these patients desire spectacle independence. This is the first report on the use of EDOF IOLs in patients who have undergone RK.
Refractive targets were plano for 15 eyes and -0.25 to -1.00 D for nine eyes. UCVA and spherical equivalent at the final follow-up visit were the primary outcome measures.
Mean UCVA was 0.56 ±0.35 (20/70) at baseline and 0.22 ±0.17 (20/33) at final follow-up. The average manifest refraction spherical equivalent was +1.68 D before surgery and -0.18 D at final follow-up. UCVA was 20/40 or better in 79% of patients; 62.5% of patients were within 0.50 D of target, 88.3% were within 1.00 D of target, and 16.7% were hyperopic at the time of final follow-up. Near acuity was J3 or better in 68.8% of patients and J4 to J6 in 31.3%.
Nine of 12 patients (75%) responded to a questionnaire administered 6 months after IOL implantation. Seven reported not requiring spectacles for distance vision, five reported not requiring spectacle correction for intermediate or near vision, and four were free of spectacles. Glare was the most prevalent of the dysphotosias experienced; four patients (44%) graded it as annoying, and one patient rated it debilitating. Seven patients (78%) were fairly or very satisfied with their visual outcomes.
DISCUSSION
Patients who have undergone refractive surgery seek a certain level of independence from contact lenses and spectacles. Those with a history of RK present with unstable corneas and high levels of optical aberrations. RK incisions disrupt both the anterior and posterior curvature ratios, which can make it difficult to calculate true corneal power and predict the effective lens position. Overestimating corneal power can lead to a hyperopic surprise.
There are few case reports and limited data on the use of multifocal lenses in patients with a history of RK primarily because of challenges in corneal power measurement and the prediction of effective lens position. Moreover, the implantation of IOLs that provide multifocality through multiple distinct focal points can decrease contrast sensitivity and cause dysphotopsias. EDOF lenses may provide a better option for these patients because they achieve multifocality through an elongated focal point. This combined with a broadened defocus curve may achieve acceptable UCVA across a larger range of residual refractive errors, as Baartman and colleagues note.
To this author’s knowledge, this is the first report on the use of an EDOF IOL in patients with a history of RK. The primary limitations of this study are its retrospective nature, the small numbers of patients and eyes, and the selectiveness of the patients’ preoperative characteristics. Additionally, patients with 16-cut RK or additional astigmatic keratotomy were not included. Moreover, the stability of keratometry measurements was not mentioned.
Spectacle Independence in Patients With Prior Radial Keratotomy Following Cataract Surgery: a Case Series
Agarwal S, Thornell E2
Industry support: No
ABSTRACT SUMMARY
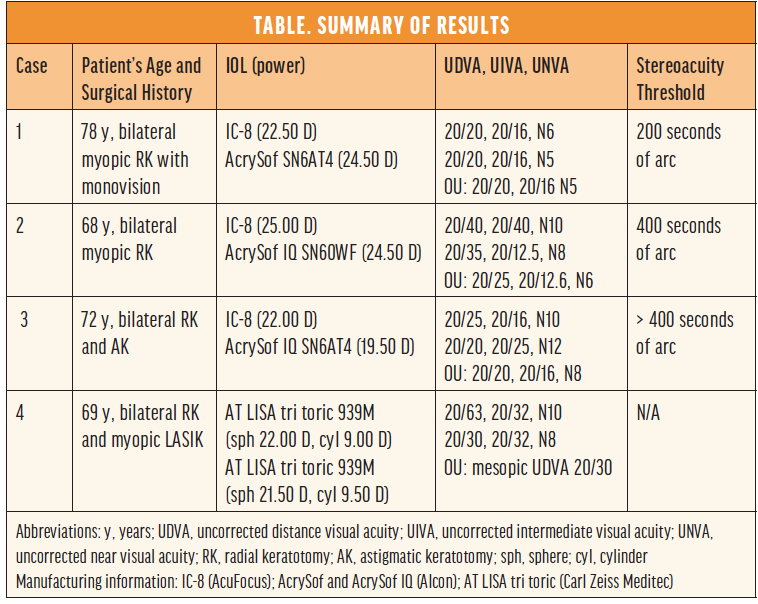
A small (N = 4 patients) retrospective case series evaluated whether the unilateral implantation of a pinhole IOL (IC-8, AcuFocus) or the bilateral implantation of a trifocal toric IOL (AT LISA tri toric IOL, model 939M, Carl Zeiss Meditec) allowed patients with a history of keratorefractive procedures to achieve spectacle independence.
Study in Brief
A small retrospective case series found that a pinhole IOL and a toric trifocal IOL achieved satisfactory results and reduced spectacle dependence in patients who had a history of keratorefractive procedures.
WHY IT MATTERS
A limited number of studies have examined the use of presbyopia-correcting lenses in patients with a history of radial keratotomy. This study suggests that successful results can be achieved but that a one-size-fits-all strategy is inappropriate.
Lens power was calculated with the Barrett True K formula. Refractive targets were set at -0.75 D for eyes that received a pinhole IOL and between 0 and ±0.50 D for eyes that received a standard monofocal or trifocal IOL.
In the IC-8 group, there was no significant difference (P > .05) in the average modulation transfer function between the eyes that received the pinhole technology and the eyes that received a monofocal lens. Contrast sensitivity was maintained in this group, whereas the patient who received trifocal lenses experienced a reduction. Most patients achieved good uncorrected distance, intermediate, and near visual acuity (Table).
DISCUSSION
Most of the challenges of IOL implantation in post-RK eyes are caused by central corneal flattening that leads to underestimations of corneal power and a progressive hyperopic shift. A slightly myopic target of -0.75 D was therefore used in eyes that received a pinhole IOL. Owing to its extended depth of focus, this lens can tolerate up to 1.50 D of cylindrical error. This lens also ameliorates the effect of peripheral higher-order aberrations. According to Agarwal and Thornell, the patient who received the trifocal lenses experienced fluctuating refractions postoperatively.2
Agarwal and Thornell conclude that pinhole and trifocal toric IOLs may be considered for patients with a history of keratorefractive procedures who desire some level of spectacle independence after cataract surgery. A limitation of this study is its small size.
1. Baartman BJ, Karpuk K, Eichhorn B, et al. Extended depth of focus lens implantation after radial keratotomy. Clin Ophthalmol. 2019;13:1401-1408.
2. Agarwal S, Thornell E. Spectacle independence in patients with prior radial keratotomy following cataract surgery: a case series. Int Med Case Rep J. 2020;13:53-60.