Pathologies causing corneal catastrophes often involve the iris. Sometimes there is comorbid pathology, and sometimes the cornea (or the corneal surgery) is the culprit. The use of an iris prosthesis can achieve a favorable outcome in some of these situations. Each in the following series of particularly interesting cases involved the cornea in a different way.
CASE NO. 1: MERMAID TRAUMATIC ‘K-TASTROPHE’
A 19-year-old woman was sleeping soundly in her college dorm during a storm. The ferocity of the gales and a nearby lightning strike shook the house just enough that a metal mermaid sculpture fell from its perch on a shelf over the bed. The sculpture penetrated the left cornea, resulting in the loss of the crystalline lens and much of the iris (Figures 1 and 2). After primary repair, the patient was photophobic, and the eye was aphakic and had marked irregular astigmatism from the central corneal scar (Figure 3). She developed a sensory exotropia with diplopia that persisted with an aphakic contact lens.
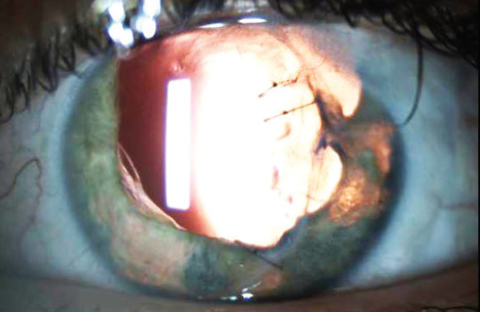
Figure 1. Preoperative image of the affected eye.

Figure 2. Preoperative midface image. Note the iris damage and small-angle exotropia.
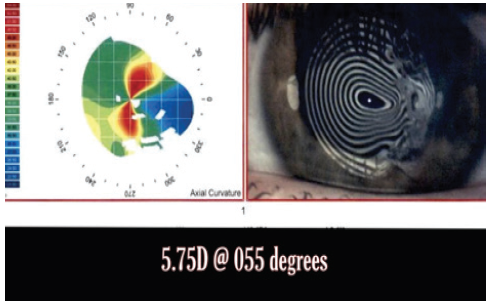
Figure 3. Corneal topography of the affected eye.
She underwent a reconstructive procedure, including the peeling of Salzmannoid changes at the penetrating paraxial corneal scar; the placement of the maximal number of limbal relaxing incisions; vitrectomy; and the placement of a sutured PMMA posterior chamber IOL and a sutured, custom, flexible iris prosthesis (CustomFlex ArtificialIris, VEO Ophthalmics). Happily, 20/20 uncorrected distance visual acuity was restored, and her light sensitivity and glare resolved completely. Amazingly, the sensory exotropia that had persisted with contact lens wear disappeared entirely after surgery (Figure 4). These visual and functional gains were sustained at the most recent follow-up visit, which occurred 5 years after surgery.

CASE NO. 2: POST-LASIK IATROGENIC ‘K-TASTROPHE’
In 1999, a 46-year-old man underwent bilateral LASIK procedures that left him with intolerable halos and poor vision, worse in the left eye. The patient underwent penetrating keratoplasty for ectasia in the left eye in 2008 and a deep anterior lamellar keratoplasty in the right eye in 2011. In 2018, a blow from an elbow ruptured the left globe and caused a significant (6.5 clock hours) loss of iris tissue. This resulted in poor vision, profound photophobia, glare that became worse with progressive cataract formation, a progressive extreme myopic shift, and resultant anisometropia. Topography confirmed 4.50 D of mostly regular astigmatism in the graft.
In May 2021, the patient underwent phacoemulsification with placement of a toric IOL and a custom, flexible iris prosthesis in the bag. Postoperatively, the photic symptoms resolved immediately. Three days after surgery, his UCVA was 20/25-1, and his BCVA was 20/25+2 with a manifest refraction of plano +0.50 x 092º. The combination of a high-powered toric IOL and artificial iris produced the happy outcome. The patient is thrilled with his visual recovery and the cosmetic appearance of his eye (Figure 5).

Figure 5. Image taken 1 day after combined phacoemulsification, IOL placement, and in-the-bag placement of a customized iris prosthesis in the left eye. Only a thin nasal rim of native iris is present.
CASE NO. 3: INCARCERATED LENS ‘K-TASTROPHE’
A 7-year-old girl sustained a ruptured right globe when pointed scissors penetrated the apical cornea, iris, and lens (Figure 6). The primary repair excised extraocular iris tissue and closed the jagged corneal laceration. Upon referral 1 year later, the patient presented with markedly reduced vision and complaints of glare and photophobia in the affected eye. On examination, BCVA was 20/125. The cataractous lens was incarcerated in the well-healed corneal wound (Figure 7). A large inferior zonular dialysis was present, and the hyaloid face was exposed. The iris was atrophic and mydriatic. Topography showed remarkably regular corneal astigmatism (Figure 8).
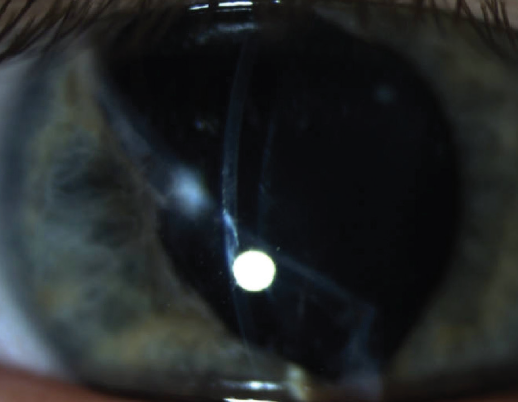
Figure 6. Slit-beam image showing full-thickness periapical scar.
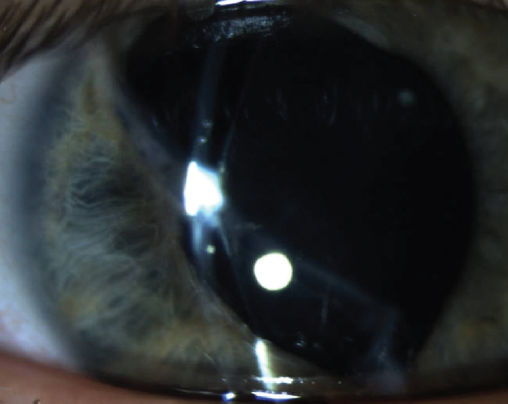
Figure 7. Slit-lamp image demonstrating incarceration of the lens in the corneal wound.
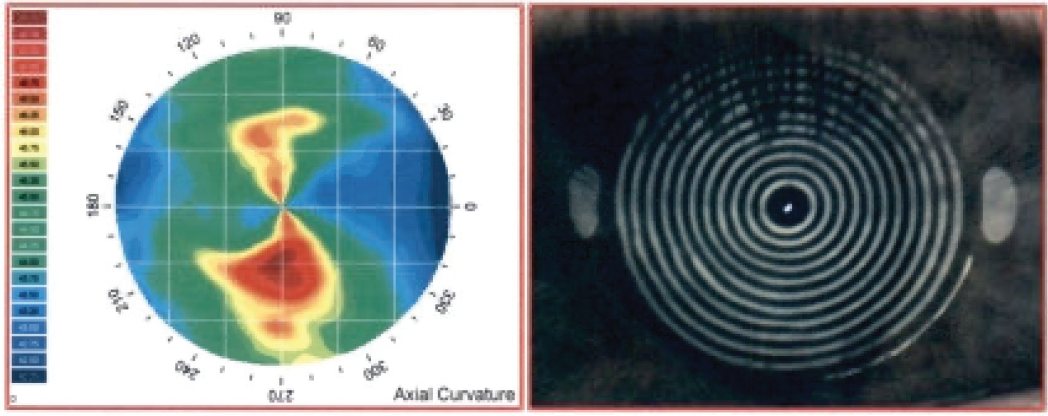
Figure 8. Topography of the same eye seen in Figures 6 and 7 showing incredibly regular astigmatism in the setting of such a large scar.
The patient underwent an internal lamellar dissection of the posterior cornea in the areas where the lens was incarcerated, which freed the lens from the cornea while maintaining an intact lens capsule. A capsulorhexis incorporated the adherent posterior corneal lamellae, and cataract surgery was performed in combination with the placement of a Cionni Capsular Tension Ring (Cionni CTR, Morcher), an IOL in the bag, and a custom, flexible iris prosthesis. Adequate pressure in the anterior chamber was maintained, and no vitreous prolapse was encountered.
Postoperatively, 20/20 BCVA was restored, and the photic symptoms resolved. This result was maintained at 5 years (Figure 9). This case demonstrates the advantages of partial lamellar internal corneal excision compared to traditional synechiolysis.1
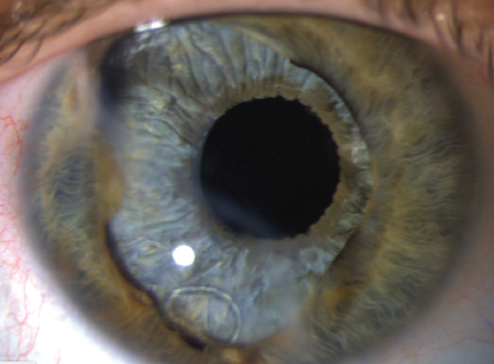
Figure 9. Final result after surgery. Note the Cionni CTR fixation element coursing around the capsulorhexis, in front of the iris device.
CASE NO. 4: QUARTET ‘K-TASTROPHE’
A 64-year-old man presented for cataract surgery and iris repair. The patient had undergone radial keratotomy 18 years earlier. Two years before referral, a bungee cord injury caused one radial keratotomy wound to open, causing total expulsion of the iris along with zonular dialysis (catastrophe number one). A few months later, he developed a retinal detachment (catastrophe number two). Following the repair of the retinal detachment by vitrectomy, the patient developed a dense black cataract (catastrophe number three). He was brought to the OR for planned phacoemulsification with the placement of a sutured Cionni CTR, an IOL, and a custom, flexible iris prosthesis.
After phacoemulsification was complete but before placement of the CTR, a dark round shadow in the red reflex emerged from the nasal periphery, revealing a progressive suprachoroidal hemorrhage (catastrophe number four, Figure 10). Surgery was halted, the hemorrhage was drained, the globe was actively pressurized, and a CTR was eventually placed (without fixation). The placement of an IOL and artificial iris device was aborted.
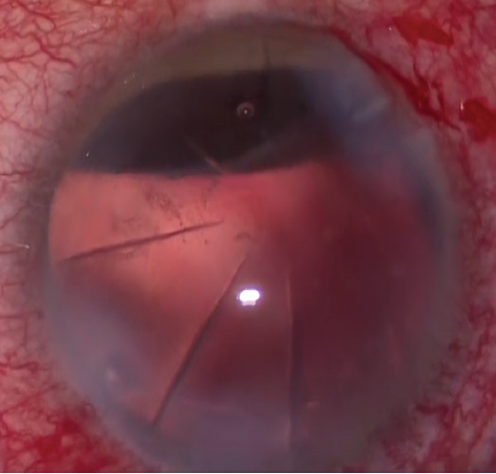
Figure 10. Note the dark suprachoroidal mound nasally in the red reflex.
The patient was managed conservatively for several months, during which time gradual resorptionof the choroidal heme was observed. He then returned to the OR. The capsular bag was reopened, an IOL was placed in the bag, an ePTFE suture was placed through the fixation element eyelet, the CTR was secured to the scleral wall, and an iris prosthesis was placed in the bag (Figure 11).
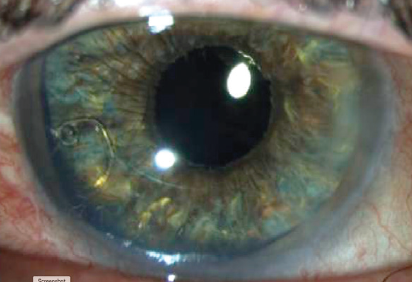
Figure 11. Image taken after secondary Cionni CTR fixation, IOL implantation, and in-the-bag placement of a customized iris prosthesis.
Amazingly, 20/20 UCVA was restored, and the glare and photophobia resolved completely.
CONCLUSION
Each of these patients had significant iris damage and photic symptoms, yet they all achieved a happy result with anterior segment reconstruction using a customized iris prosthesis.
1. Hamad JB, Sivaraman KR, Snyder ME. Lamellar dissection technique for traumatic cataract with corneal incarceration. Cornea. 2021;40(3):393-397.