
The aging lens presents challenges, but it also creates opportunities for surgical vision correction. It may be helpful to think of the challenges and the opportunities it presents in terms of the stages of dysfunctional lens syndrome (DLS). As the lens ages and changes, some surgical options become less attractive while others become more so (see Stages of DLS). By matching the stages of DLS with the most appropriate surgical choices for the patients in that age range, we can ensure fruitful discussions with them and, hopefully, obtain the best possible visual outcomes.
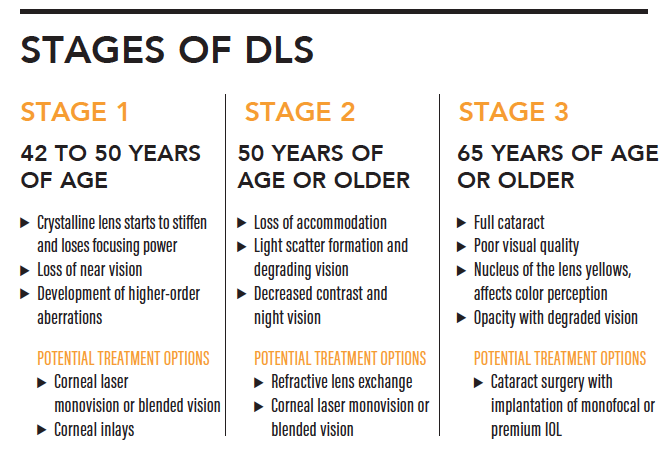
Source: Dysfunctional lens syndrome, a new way to educate patients. EyeNet. October 14, 2016. https://www.aao.org/eyenet/academy-live/detail/dysfunctional-lens-syndrome-educate-patients. Accessed January 30, 2020.
STAGE 1 DLS
One of the first signs of lens dysfunction is loss of near vision. Patients in their 40s may have great distance vision or great corrected distance vision, but they begin to notice that their vision at near is not what it used to be. The lens is still clear, but its function is deteriorating and accommodation is no longer working properly.
Before these changes set in—when patients are in their 30s and their eyes are working fine—lens-sparing options are typically discussed for those who are interested in refractive surgery. Most often the surgical course is corneal laser surgery (LASIK, PRK, or SMILE), but other available lens-sparing options including corneal inlays and phakic IOLs can also be used.
As patients enter stage 1 DLS, we must keep in mind that a lens-sparing procedure will be a static solution to a dynamic problem. That is, the cornea, the inlay, or the phakic IOL will stay the same over time, while the lens will continue to age and lose function. First, presbyopia will progress, and then cataract will begin to form in stages 2 and 3 DLS, increasing light scatter and affecting visual acuity.
When patients are in their early 40s, we may still sometimes offer lens-sparing solutions, such as LASIK, inlays, or phakic IOLs, with a mini-monovision approach to provide some near or intermediate vision. But these options become less attractive as patients enter their late 40s and 50s and progress further into DLS.
STAGE 2 DLS
Lens replacement technologies have continued to improve over time, and today we have many options to offer patients progressing into later stages of DLS. At these stages, we should start to lean more toward lens replacement options than lens-sparing ones.
One caveat is that high myopes have a heightened risk for retinal detachment after lens replacement.1 (Editor’s note: For more on the topic of retinal detachment risk, see the article by Steve Charles, MD, FACS, FICS.) Therefore, the risk-benefit ratio of lens replacement should be thoroughly discussed with any high myope who is considering such surgery. Conversely, hyperopes are good candidates for lens-based solutions at an earlier age because the risk-reward ratio is more favorable for them.
It is worth giving some consideration to modern phakic IOLs for patients in stage 1 and early stage 2 DLS. Some surgeons have shied away from phakic IOLs because of the risk of cataract development when they are implanted in older patients. The risk of cataract formation is relatively low when the phakic IOL is implanted in young patients, but the risk rises as the age of implantation passes the mid-40s.2-5 Another possible drawback, as suggested previously, is that a phakic IOL is a static fix for a moving target—the aging of the crystalline lens and the progression of presbyopia.
In the United States, the principal phakic IOL is the Visian ICL (STAAR Surgical; Figure). In Europe, the next generation of the STAAR lens, the EVO Visian ICL, has been in use for several years, and US clinical trials of the lens are ongoing. The design of the EVO, which includes a central port that serves to circulate aqueous, helps to neutralize the risk of cataract development in regard to patient age that is seen with other phakic IOLs,5,6 such that it may be implanted in older patients with less worry of inducing cataract formation.
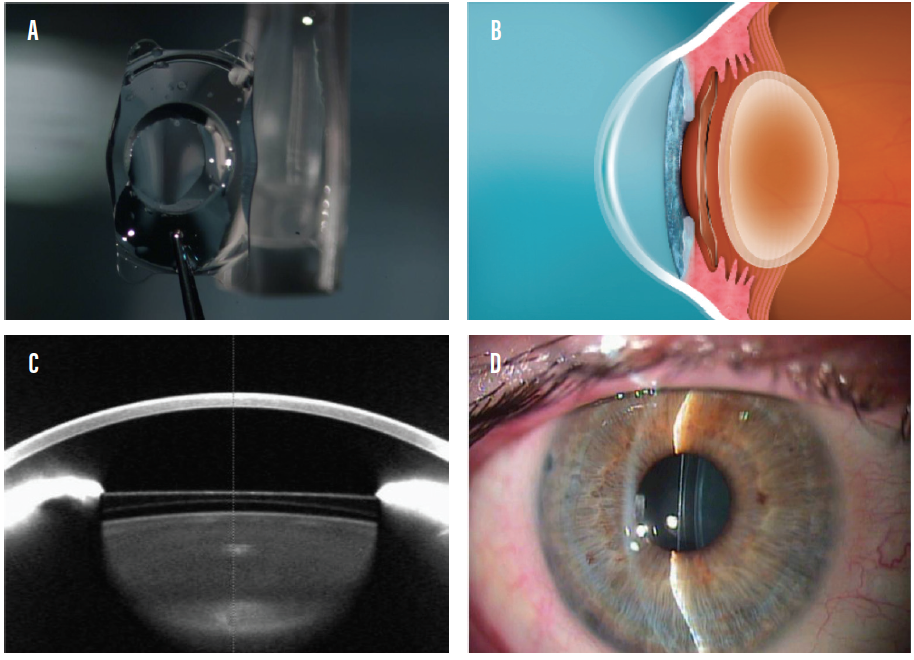
Figure. The Visian ICL (A) is a posterior chamber phakic IOL implanted in the eye and positioned behind the iris and in front of the natural lens (B–D).
If this lens becomes available in the United States, and if it proves to be as cataract-neutral in older patients as it seems, it may become a go-to refractive surgical option not only for young patients but also those in early DLS in their late 40s to 50s. Further, in the future, the EVO lens platform will be available with an extended depth of focus (EDOF) option, potentially making it an even more attractive solution for patients with stages 1 and 2 DLS.
STAGE 3 dls
In later stages of DLS, lens replacement becomes the principal refractive surgical option. The offerings in this category continue to expand. From oldest to newest, they include the following.
Basic lens replacement with a standard monofocal IOL. This can correct visual opacity, but it may not eliminate the patient’s need for glasses. Correction for distance and/or near vision may still be needed postoperatively. Monovision can help to provide patients with some intermediate or near vision, but patients might be dissatisfied if the refractive target isn’t reached in one or both eyes.
Premium monofocal IOLs. Toric IOLs can reduce astigmatism. Normally, these lenses would be targeted for distance correction or used with a monovision strategy.
Bifocal or multifocal IOLs. Patients usually obtain good near vision with bifocal and multifocal lenses, but their fixed focal points can leave gaps in near or intermediate vision. Today, new-generation bifocal IOLs that are available in a variety of add powers have replaced earlier generations, allowing surgeons and patients to create mix-and-match or customized vision options.
EDOF lenses. Designed to decrease the night-vision problems associated with multifocal IOLs and to provide a broader, continuous range of correction, EDOF IOLs are a newer option in our armamentarium. Some surgeons are now combining an EDOF lens in one eye with a multifocal in the other.
Adjustable IOLs. The Light Adjustable Lens (RxLAL, RxSight) is a relatively new option that gives patients the opportunity to try out their vision in the early postoperative weeks, allowing the surgeon to adjust the lens power for premium monovision or other vision-correction strategies. This is a great option for patients with previous refractive surgery, for whom traditional lens power calculation can be a significant challenge. An EDOF option will soon be available for the RxLAL so that, once the patient’s vision is confirmed to be satisfactory, an additional depth of focus treatment can be added to enhance vision further. Other adjustable IOLs as well as exchangeable IOL platforms are likely to be available in the future.
Trifocal IOLs. Many patients do quite well with bifocal or multifocal IOLs, but some find that they are still wearing glasses for computer, desktop, or other intermediate activities; they note that, despite investing a significant amount of money in premium IOL surgery, they still are not spectacle independent. Trifocality is an exciting new possibility that can help to address these concerns. Several trifocal technologies are available internationally, but in the United States the only available lens is the AcrySof IQ PanOptix (Alcon).
EXPANSION IN IOLS, EXPANsion in THE MARKET
The expansion in the range of IOL options outlined here is one of many factors that may give surgeons more confidence to enter the premium IOL market. Despite all the many advances we have seen in recent years, the premium IOL market still accounts for less than 10% of the overall IOL market.7 Many surgeons are sitting on the sidelines, reluctant to adopt some of these high-technology options because they might not be comfortable offering premium IOL technologies.
One barrier to a greater adoption rate is that some surgeons do not have access to an excimer laser or feel confident in being able to address refractive surprises. Others may not be comfortable doing a lens exchange for a dissatisfied premium lens patient. For these surgeons, new options such as the RxLAL or a trifocal IOL may address these concerns. For others, improved diagnostics and better IOL power calculation formulas such as the Barrett II may offer improved confidence.
Think about the resources we have available today for lens replacement surgery: highly nuanced IOL solutions, improved diagnostic modalities that can provide increased confidence in our lens choices, better IOL power calculation formulas, and intraoperative aberrometry and guidance to help nail the refraction. In the near future, we may have more adjustable and exchangeable IOL technologies that will allow patients to upgrade their lens choices as they do today with their phones.
With so many technologies at our beck and call, the options for lens replacement—and the results we can offer to our patients—have never been greater.
1. SS, Mikkelsen KL, La Cour M. Risk of pseudophakic retinal detachment in 202,226 patients using the fellow nonoperated eye as reference. Ophthalmology. 2013;120:2573-2579.
2. Chen LJ, Chang YJ, Kuo JC, Rajagopal R, Azar DT. Metaanalysis of cataract development after phakic intraocular lens surgery. J Cataract Refract Surg. 2008;34(7):1181-1200.
3. Hassaballa MA, Macky TA. Phakic intraocular lenses outcomes and complications: Artisan vs Visian ICL. Eye (Lond). 2011;25(10):1365-1370.
4. Moshirfar M, Imbornoni LM, Ostler EM, Muthappan V. Incidence rate and occurrence of visually significant cataract formation and corneal decompensation after implantation of Verisyse/Artisan phakic intraocular lens. Clin Ophthalmol. 2014;8:711-716.
5. Gimbel HV, LeClair BM, Jabo B, Marzouk H. Incidence of implantable collamer lens-induced cataract. Can J Ophthalmol. 2018;53(5):518-522.
6. Packer M. The Implantable Collamer Lens with a central port: review of the literature. Clin Ophthalmol. 2018;12:2427-2438.
7. 2017 Annual US cataract surgeon survey report. Market Scope. Published May 2017. https://market-scope.com/products-page/cataract-reports/2017-annual-us-cataractsurgeon-survey-report. Accessed April 4, 2018.




