
It is expected that 123 million people in the United States and 2.1 billion people worldwide will be affected by presbyopia in 2020, according to estimates by Market Scope. Nonsurgical options are available to address presbyopia, but they are inconvenient and can hinder patients’ daily activities. Thankfully, there has been significant research into surgical solutions for this condition that will eventually affect every sighted person.
There are two main ways to approach surgical treatment of presbyopia: lens-based techniques that address presbyopia directly, and cornea-based techniques that address the problem indirectly. This article focuses on cornea-based options; lens-based options are covered at length in an article by William F. Wiley, MD.
DIAGNOSTICS AND WORKUP
As my staff and I often tell our patients, “No two eyes are the same.” Therefore, our refractive surgery diagnostic processes must be robust, especially for patients in the presbyopic age group. A cornea-based approach to presbyopia correction requires a healthy tear film and cornea, a clear lens and vitreous, and a healthy macula.
In a workup of a patient interested in presbyopia correction, in addition to the typical refraction, slit-lamp examination, and posterior segment examination, we perform these tests:
- Analysis with the AcuTarget HD (Visiometrics) to objectively evaluate scatter and tear film breakup time;
- Epithelial mapping (Avanti, Optovue) to identify subclinical epithelial disease, ocular surface disease, and keratoconus;
- Topography (OPD-Scan III, Nidek) to detect ocular surface disease and keratoconus;
- Tomography (Pentacam, Oculus) to evaluate the patient’s candidacy for different laser vision correction options;
- Macular OCT (Avanti) to assess macular health and the patient’s candidacy for lens-based options; and
- Testing of tolerance to anisometropia with loose lenses and the phoropter.
If ocular surface disease is present preoperatively, it must be managed before surgery is considered. If there is a high degree of ocular scatter, a lens-based option is preferable to a cornea-based solution. Different degrees of ocular scatter indicating differing levels of dysfunctional lens syndrome (DLS) can be seen in Figures 1 and 2. If vitreous opacity or macular disease is present, we refer the patient to a retina colleague before any surgical recommendation is made.
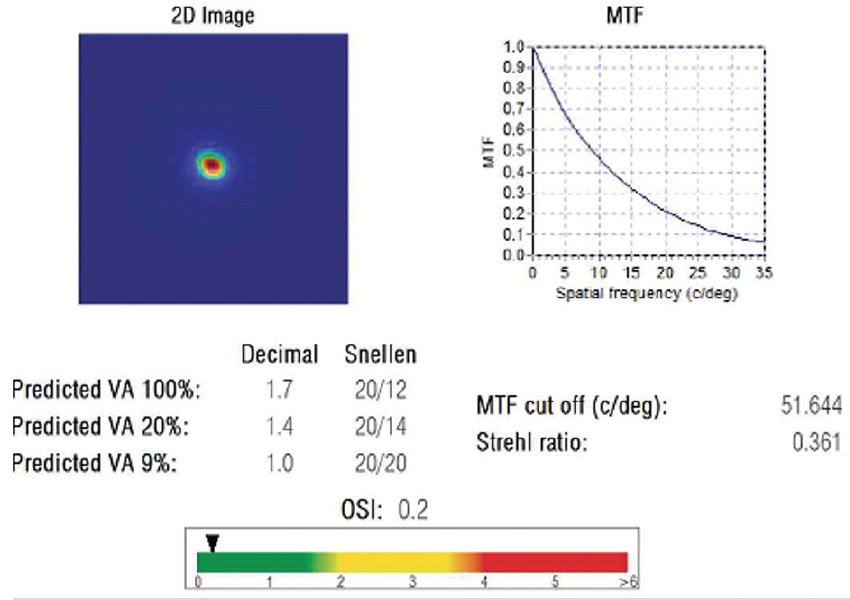
Figure 1. A report from the HD Analyzer for a patient in his 20s. Note the low ocular scatter index (OSI) in green and the high potential vision.
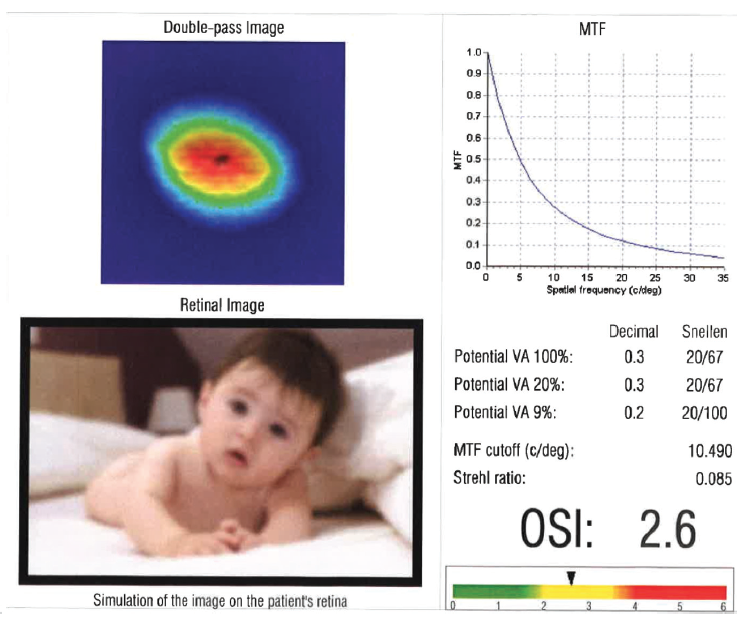
Figure 2. A report from the HD Analyzer for a 60-year-old patient. He has a corrected distance visual acuity of 20/20 but complains that his vision is just “not quite what it used to be.”
Assuming all of the aforementioned tests show normal, healthy function, we recommend moving forward with a cornea-based option.
LASER VISION CORRECTION
LASIK has been called the most effective elective procedure. Objectively it is one of the most thoroughly researched surgical procedures, and patient satisfaction rates hover around 99%.1 Other forms of laser vision correction can provide similar results, whether they are performed on the surface of the eye as in PRK or within the stroma as in SMILE.
Monovision laser vision correction was one of the first approaches to the surgical management of presbyopia. In the early days, surgeons often targeted a refraction of -2.00 D or even greater in the near eye. Unfortunately the disparity created would greatly decrease an older patient’s stereopsis and result in a double hump in the binocular defocus curve, with a dead spot in the middle. With this knowledge, surgeons currently generally recommend less anisometropia, usually termed blended vision, rather than monovision.
Durrie et al showed that a target of -1.50 D can provide optimal near and distance visual acuity for most patients, and this is often used as a starting point when testing a patient interested in presbyopia correction.2 Younger patients can be targeted for mini-monovision as low as -0.75 D, whereas older patients may require a near target of -1.75 D or more. In our practice, we use the phoropter to find the greatest amount of anisometropia that a given patient can tolerate and still retain subjective stereopsis.
It is important to keep in mind that neural adaptation to blended vision requires time. Functional MRI studies have shown that it can take up to 15 months for full neural adaptation to multifocal IOLs. Adjusting to blended vision can take just as long for some people, although the process is much faster for most.
For patients who do not initially adjust well to any anisometropia in the phoropter but who are motivated to be less dependent on spectacles, we consider a contact lens trial or a lens-based option. We counsel patients that most can adjust, given enough time, but we offer a free enhancement for distance visual acuity if a patient is ultimately unable to adapt to blended vision.
CORNEAL INLAYS
At present, only one corneal inlay is approved by the FDA: the Kamra (CorneaGen). This device increases depth of focus through the use of pinhole optics—similar to an f-stop on a camera. The inlay has been shown to improve monocular distance and near visual acuity as well as stereopsis in comparison with traditional monovision.3
The Kamra is designed to be placed in a corneal pocket over the visual axis. The central 1.8-mm aperture allows parallel light rays to pass through while the rest of the inlay blocks more peripheral rays. There are 8,400 holes in the inlay that allow nutrient flow through the device, and its polyvinylidene difluoride material has been shown to be inert to the cornea.3
Of course there is nuance to every procedure. For the Kamra to provide optimal visual results, the eye must have a healthy tear film, cornea, posterior media, and macula. Two additional things are necessary:
- The surgeon must use a slightly myopic refractive target, usually around -0.75 D. Laser vision correction can be used to achieve this result; and
- The inlay must be placed posteriorly in the stroma due to the lower density of keratocytes there. We place ours at 250 µm from the endothelium.
Rejection of the device is rare with posterior placement given the lower density of keratocytes,4,5 but it is crucial to monitor patients for the development of haze or a refractive shift in the first year. Follow-up over time is required.
THE FUTURE
Two concepts for the surgical correction of presbyopia that have yet to reach the mainstream deserve mention here.
Several surgical solutions have been proposed to increase depth of focus by increasing spherical aberration. The most well-known among these options may be the Presbyond Laser Blended Vision software (Carl Zeiss Meditec, not available in the United States). The benefit of this approach is that it should provide better stereopsis by improving distance visual acuity while maintaining acceptable near visual acuity. Spherical aberration can also be modified in an off-label fashion using the Contoura planning software (Alcon), but this is not recommended due to the complexity of the resulting change in sphere and the difficulty of reversing the effect once the ablation is performed.
Another concept, laser-induced refractive index changing (LIRIC; Clerio Vision) is a femtosecond laser–based technology in development that may provide not only refractive change but also possibly increased depth of focus through the induction of multifocality or spherical aberration. Given that no incision is made into the cornea, in the future this technology may provide the benefits of laser vision correction while minimizing the risks.
SUMMARY
Surgical management of presbyopia is a developing field. Three years ago, my colleagues and I began to focus on presbyopia in our clinic. Today, surgical management of presbyopia accounts for nearly half of our practice volume, and that figure continues to grow. The need among our patients is significant, and the satisfaction we can deliver now is greater than ever.
1. Sandoval HP, Donnenfeld ED, Kohnen T, et al. Modern laser in situ keratomileusis outcomes. J Cataract Refract Surg. 2016;42(8):1224-1234.
2. Durrie DS. The effect of different monovision contact lens powers on the visual function of emmetropic presbyopic patients (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2006;104:366-401.
3. Vukich JA, Durrie DS, Pepose JS, Thompson V, van de Pol C, Lin L. Evaluation of the small-aperture intracorneal inlay: Three-year results from the cohort of the U.S. Food and Drug Administration clinical trial. J Cataract Refract Surg. 2018;44(5):541-556.
4. Patel S, McLaren J, Hodge D, Bourne W. Normal human keratocyte density and corneal thickness measurement by using confocal microscopy in vivo. Invest Ophthalmol Vis Sci. 2001;42(2):333-339.
5. Moarefi MA, Bafna S, Wiley W. A review of presbyopia treatment with corneal inlays. Ophthalmol Ther. 2017;6(1):55-65.




