CASE PRESENTATION
A 52-year-old woman underwent refractive lens exchange with implantation of a trifocal IOL in each eye. Surgery on the left eye was uncomplicated. During surgery on the right eye, mild diffuse zonular laxity was noted, and a capsular tension ring was inserted prior to IOL implantation. Postoperative recovery was largely unremarkable except that the patient continued to complain of photic phenomena for several months after surgery despite optimization of the ocular surface. Specifically, she reported mild halos in both eyes and glare in the right eye that made driving at night difficult. Treatment with topical brimonidine tartrate ophthalmic solution (Alphagan P, Allergan) improved but did not eliminate her symptoms.
Upon presentation, uncorrected distance visual acuity is 20/20 OU. Refraction is plano in each eye. An ocular examination that includes the posterior capsule and macula is unremarkable except for the following: the IOL is perfectly centered in the left eye, but in the right eye the center of the IOL is located 1 mm above the center of the pupil. Corneal topography and wavefront scans of the eyes are shown in Figures 1 and 2, and pupillometry is displayed in Figures 3 and 4.
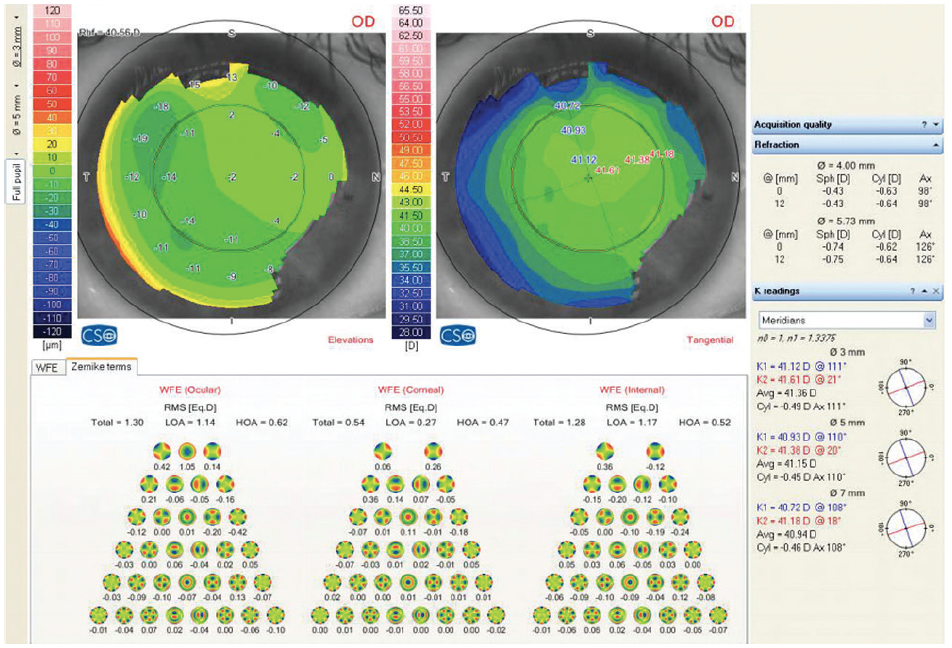
Figure 1. Corneal topography and wavefront scan of the right eye.
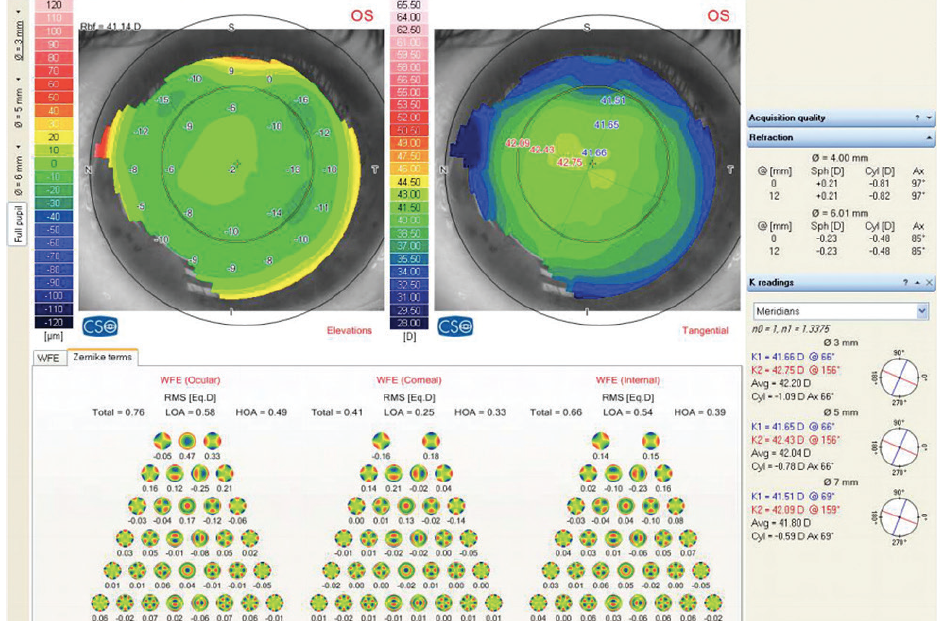
Figure 2. Corneal topography and wavefront scan of the left eye.
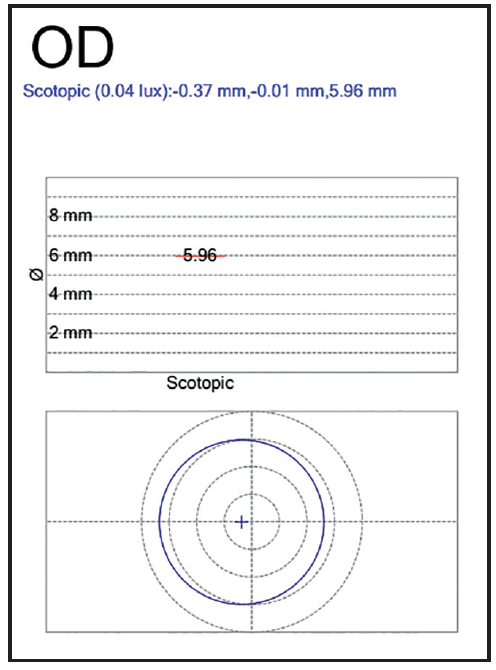
Figure 3. Scotopic pupillometry for the right eye.
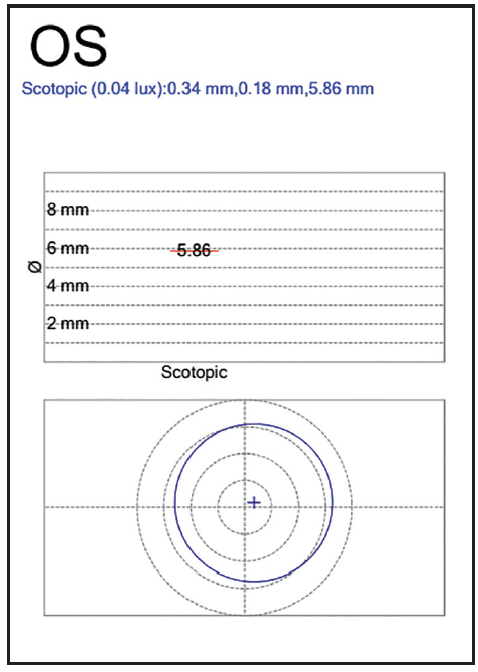
Figure 4. Scotopic pupillometry for the left eye.
How would you proceed?
—Case prepared by Allon Barsam, MD, MA, FRCOphth

ARTHUR B. CUMMINGS, MMED (OPHTH), FCS(SA), FRCS(ED)
On wavefront aberrometry, the right eye has lower-order aberrations (LOAs) measuring 1.14 µm and higher-order aberrations (HOAs) measuring 0.62 µm. The left eye has LOAs measuring 0.58 µm and HOAs measuring 0.49 µm. These measurements suggest that the right eye has a residual refractive error despite a subjective refraction of plano. The corneal HOAs are 0.27 µm for the right eye, and the LOAs are 0.47 µm. The corneal HOAs for the left eye are 0.25 µm, and the LOAs are 0.33 µm. The right eye therefore has higher amounts of wavefront error and corneal HOAs than the left eye.
If the IOL is otherwise stable, one could consider a customized corneal laser vision procedure to reduce the symptoms of glare in the right eye. This strategy would make particular sense if the cornea-derived ablation profile matches the wavefront-derived ablation profile. If the profiles did not agree, one would have to be careful not to induce too many corneal aberrations while correcting the ocular wavefront, but this will be less of an issue because the crystalline lens has already been extracted.
If the IOL is not stable, then the best approach would be to stabilize the lens and, in the process, recenter it. This could be done in various ways such as ab externo fixation with a loop suture or rotation of the IOL through 90º within the bag. This case is going to require extensive informed consent and a discussion of the risk-benefit ratios of the various approaches.

DAMIEN GATINEL, MD, PhD
The visual symptoms in the patient’s right eye are probably related to the superior decentering of the implant. Although the ocular wavefront can be instructive, it alone cannot provide all necessary information on optical quality. The comparative study of the two eyes revealed a slightly larger magnitude of HOAs in the right eye, but the complex interactions between the corneal and internal (IOL-related) aberrations must be taken into account.
It is also worth noting that an aberrometer uses infrared radiation; this wavelength is longer than those of the visible spectrum and is thus less able to account for the effects of diffraction. Most current aberrometers do not have sufficient resolution to capture the fine wavefront modulations produced by a diffractive trifocal IOL. In addition to decentering, it is possible that an associated excessive tilt of the optic is producing undesirable optical effects that contribute to the photic phenomena experienced by the patient. In this situation, it is important to focus on the patient’s visual symptoms.
One option is to suture one lens haptic to the sclera in order to move the IOL down and recenter it in the right eye. If this attempt failed, the surgeon could consider exchanging the lens for a multifocal IOL sutured to the sclera. Proper centration of the multifocal optic would be critical to prevent similar unwanted visual symptoms postoperatively.

WHAT I DID: ALLON BARSAM, MD, MA, FRCOphth
The patient was scheduled for wavefront-guided LASIK on the right eye. My plan was to correct all internal HOAs with the exception of spherical aberration. On the day of surgery, however, I was unable to obtain a homogeneous wavefront scan, presumably due to tear film instability. I therefore deferred treatment, and the patient is undergoing further optimization of the ocular surface. We will revisit laser treatment in the future.