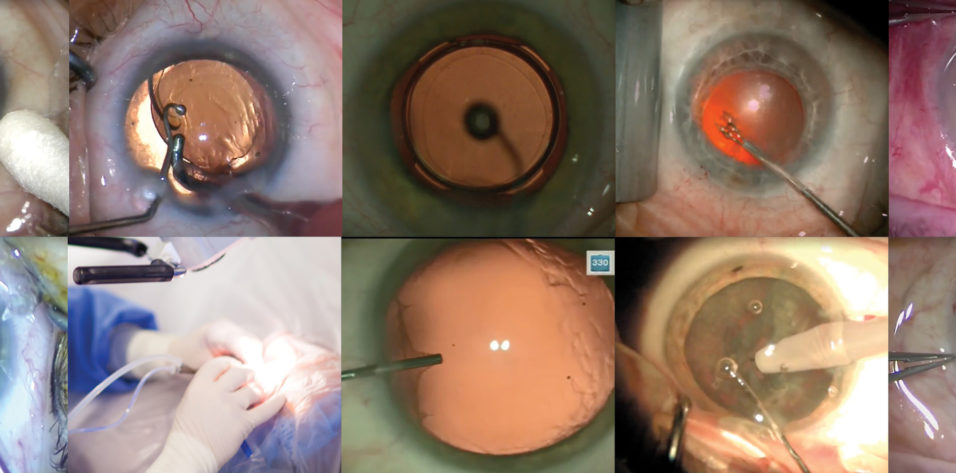
A routine cataract surgery case can vary significantly among ophthalmic surgeons as a reflection of regional preferences, hospital or ambulatory surgery center support, and surgeon experience. Regardless of technique, however, the time duration of routine cataract surgery is typically fairly predictable, allowing efficient scheduling. High-volume surgeons often separate complex cataract cases from routine cases in order to maximize productivity and optimize flow in the OR.
My specialty surgery practice includes cornea, refractive, cataract, glaucoma, and laser procedures, along with comprehensive dry eye care. I segregate routine and refractive cataract surgeries from other procedures in the ambulatory surgery center for efficiency and staff focus. Among the routine cataract surgery cases, my staff and I attempt to avoid inclusion of eyes with traumatic, mature, brunescent, or zonulopathic cataracts; poorly dilated pupils; and patients deemed uncooperative for topical anesthesia. Refractive cataract surgery cases may involve the femtosecond laser, intraoperative aberrometry, toric IOLs, and presbyopic-correcting IOLs. These cases, along with combined cataract and MIGS procedures, may also be included among the routine cases.
STANDARD PROTOCOL
My routine cataract surgery, as demonstrated in the accompanying Eyetube video (bit.ly/bowden0220) and outlined here, starts with the appropriate time-out to confirm the patient, correct eye, and procedures, and it continues with IOL verification by the surgeon, anesthesiologist, and surgical team. The patient is then prepped, draped, and positioned under the OPMI Lumera surgical microscope (Carl Zeiss Meditec). I position myself for a temporal surgical approach. I am a tall surgeon, and I prefer to position the footpedals side by side for left eyes and widely spread for right eyes. The patient is placed in a reverse Trendelenberg bed position to minimize abdominal pressure on the diaphragm and to provide increased space for my leg position.
The surgery commences with the sideport incision; I place my left hand 90º to the left of the primary incision and use a 1-mm keratome to create the sideport (Figure 1). I use a 2.7-mm keratome for the primary incision, a size that corresponds with the appropriate irrigation sleeve of the Stellaris Elite Vision Enhancement System (Bausch + Lomb) phaco handpiece, the I/A tip, and the cartridge used for IOL insertion.
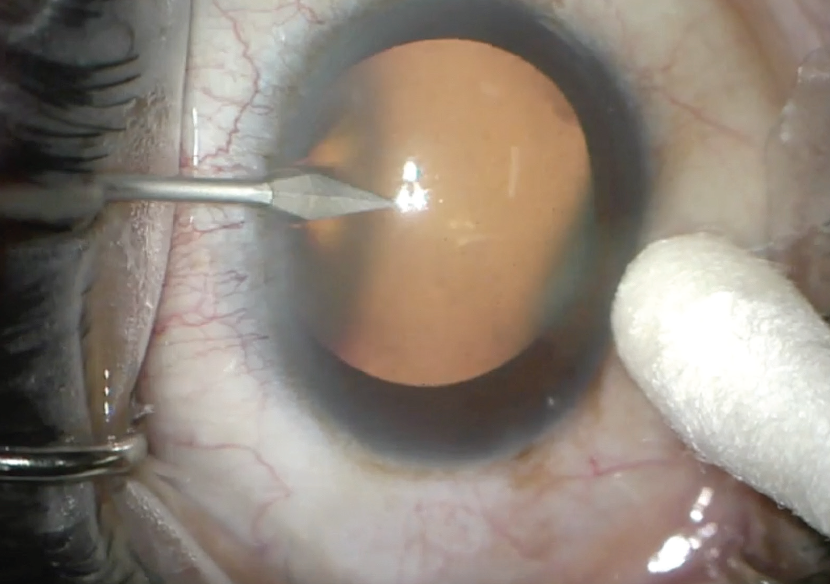
Figure 1. A 1-mm keratome is used to make a sideport incision.
The anterior chamber is irrigated with 1% lidocaine (Xylocaine MPF, Accutome), followed by injection of the dispersive OVD EndoCoat (Johnson & Johnson Vision). With adequate pupil dilation, a bent 25-gauge cystotome is used to create a 5-mm continuous curvilinear capsulorhexis (Figure 2), relying on Purkinje images to guide centration while the patient gazes into the coaxial microscope light. Next, gentle hydrodissection of the lens nucleus is performed with a Chang cannula, and I attempt to obtain 1 clock hour of rotation (Figure 3).
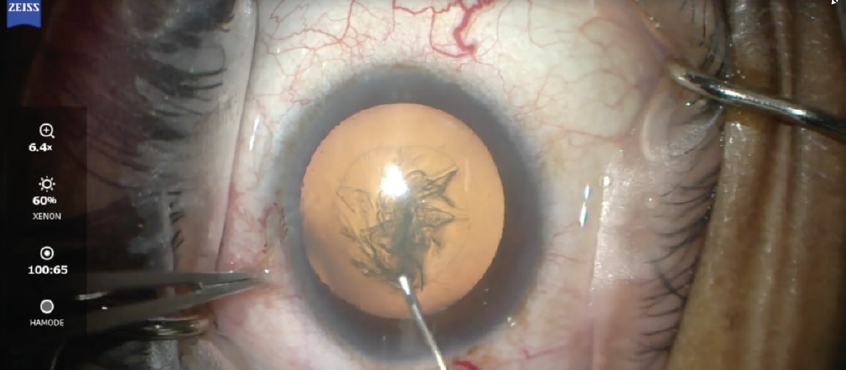
Figure 2. A bent 25-gauge cystotome is used to create a 5-mm continuous curvilinear capsulorhexis.
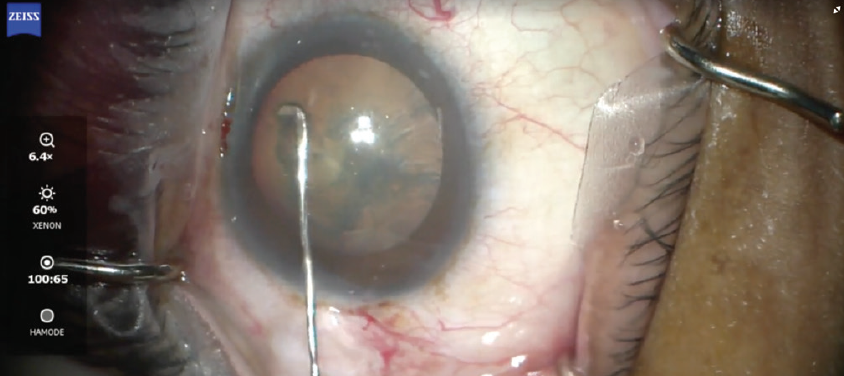
Figure 3. Gentle hydrodissection of the lens nucleus is achieved with a Chang cannula.
When femtosecond laser nuclear fragmentation has been performed, the nucleus is rocked to permit gas bubble escape. During phacoemulsification, I use a quick-chop or divide-and-conquer technique for nucleus disassembly. Frequently I use a combination of the two methods, guided by the nuclear density. When feasible, phacoaspiration is also incorporated with the high vacuum settings of the Stellaris unit.
With a 30º phaco tip, the Venturi pump system of the Stellaris Elite is efficient for phacoemulsification. I always take care to maximize tip occlusion by finger-tip rotation of the handpiece. I have found that a high vacuum level (up to 500 mm Hg) permits excellent nuclear followability and tip occlusion, allowing safe and efficient nuclear removal in the pupillary zone at the iris plane. The Adaptive Fluidics feature of the Stellaris provides exceptional chamber stability.
I routinely employ a bimanual phaco technique, using the Koch chopper via the sideport incision to assist the phaco-chop technique and guide nuclear fragments to the phaco tip. The Stellaris Elite I/A tip is a useful tool to facilitate cortical removal via stripping and aspiration. The posterior capsule is polished with a Terry silicone tip squeegee. When a Crystalens (Bausch + Lomb) or Trulign toric (Bausch + Lomb) is implanted, the anterior capsule is polished with a Singer Sweep Polisher (Accutome). The capsular bag is then expanded with a cohesive OVD (ProVisc, Alcon).
IOL INSERTION
My monofocal IOL of choice for patients who do not elect a lens technology upgrade is the SofPort LI61SE three-piece IOL (Bausch + Lomb). After successful placement of the lens in the capsular bag, I remove the ProVisc from the capsular bag with the I/A tip and hydrate the corneal incisions using balanced saline solution with a 30-gauge cannula to ensure a watertight closure.
After the drape is removed, I place any OVD that remains in the syringe over the cornea and instill topical moxifloxacin, bromfenac, and prednisolone drops. Lastly, I place a plastic protective shield over the operated eye.
After a brief observation in the postoperative suite, the patient is discharged. Patients receive detailed instructions on the appropriate eye drop regimen as well as on other activity instructions. For routine cases, my typical postoperative regimen includes Bromsite (bromfenac ophthalmic solution 0.075%, Sun Ophthalmics) three times daily for 6 weeks, Lotemax SM (loteprednol etabonate ophthalmic gel 0.38%, Bausch + Lomb) three times daily for 3 weeks and then twice daily for 3 weeks, and Vigamox (moxifloxacin HCl ophthalmic solution 0.5%, Alcon) three times daily for 1 week.
CONCLUSION
As we all know, routine cataract surgery can sometimes go sideways, and it is important for surgeons to be vigilant and prepared for complications or untoward events. The routine outlined here has worked well for me. A flexible and coordinated team approach to routine cases can be a rewarding experience for the surgeon and the patient.