Many of the patients sitting in your waiting room right now are ideal candidates for a service you can provide—one that will change your patients’ lives and drive revenue in practice. So, why aren’t you offering it yet?
I believe strongly in the value of aggressively managing dry eye disease (DED). As a practice administrator, businessman, and consultant, I am constantly recommending adding DED services to my colleagues and friends. But DED programs shouldn’t be considered simply an add-on value; they should be created, dedicated, and offered the support required to become first-line offerings in ophthalmic and optometric practices. This advice is akin to the business concept of digging for oil in your own backyard. The beneficiary of this service is likely already in your waiting room, and the financial impact it can have on your practice is game-changing.
So, why is the advanced management of DED missing in so many practices?
We could all use a rising market right now
DED affects more than 40 million adults1,2 in the United States today, and this number is rising quickly. Some say the rise might be due to the increase in allergy-driven ocular ailments. Others suggest the overuse of digital technologies as the main driver. Perhaps we are just more sensitive to our visual discomfort than we have been in generations past, or all of the above. The market for DED is massive, and it is growing.
DED is affecting our cataract patients and may affect cataract outcomes.3 About 77% of eyes being screened for cataract surgery have positive corneal staining,4 an incidence rate much higher than anticipated. Additionally, 86% have some component of meibomian gland dysfunction (MGD).5 DED is more prevalent than most practices think, far less diagnosed than it could be, and even more infrequently adequately treated. This is an opportunity.
Identifying DED patients
Your lobby is very likely already full of patients dealing with DED. Half of patients with DED are asymptomatic, so it is important to screen all patients for DED.6 This can easily be done using a DED questionnaire, such as the Standard Patient Evaluation of Eye Dryness (SPEED) questionnaire.7 This subjective approach to identifying dry eye patients is helpful and meaningful. However, it is driven by what the patient says, not what the patient actually sees, so testing and consultation are needed alongside the questionnaire.
One of the challenges of diagnosing DED is first identifying symptoms and then assessing where they are on the spectrum of severity. Where they are placed on the spectrum of severity determines the best first step for treating the disease.
Treating DED patients
The type and severity of dry eye disease can dictate the use of innovative new tools, but it can also interrupt the flow of a practice, so it’s important to plan your diagnostic and treatment workflow to optimize your staff and clinic time. Choosing a path or protocol can help expedite decision-making for flow and efficiency.
Once this kind of flow and efficiency is established, more attention should be paid to the treatment of DED. This is where operational excellence can make or break the success of an implementation. Many practices believe that more technology is always better when treating the patient and answering the patient’s needs. In many cases this is true. However, an increase in choices can delay the decision-making by the provider and delay treatment options that could help a patient more quickly.
TearCare Background
TearCare delivers a personalized, open-eye experience that’s easy to incorporate
For practices yet to take the plunge into evacuating the meibomian glands, TearCare (Sight Sciences) is a good starting point. The TearCare system includes a small SmartHub that controls heat duration and temperature consistency, as well as SmartLids, which are wearable heating elements that universally adhere to any upper and lower lids. The TearCare SmartHub has a very small footprint and is portable. We use the provided clearance tool to manually express the softened meibum of both the upper and lower lids, so we can be attentive to every single meibomian gland. Disposable costs are reasonable, and using the TearCare device takes only about 20 to 30 minutes, including the heating period and gland clearance.
Many programs offer innovative and interventional DED treatments without DED standards of protocol and flow. What this can invite is a 'dry eye circus' instead of a dry eye center of excellence. A dry eye circus occurs when, amongst infinite options, it is not clear which one should be the best first-line treatment. Which treatment plan is best for the type and severity of the patient?
Access, Demand, payment landscape
Now that we have discussed the great need in the marketplace for DED therapy and potential value to a practice, let’s talk about access. The number of ophthalmologists has been decreasing every year for the past decade. Last year, Dr. Richard Edlow reported that the number of ophthalmologists has and continues to decline by 3.5% per year.
While the number of ophthalmologists is declining, demand for age-related services in eye care will grow by 7.5% per year every year for the next 10 years (Figure). In a few short years, there will be far too much demand to be met by those currently offering interventional DED treatment. Greater use of tablets and small screens will likely produce more patients that need you to fill the treatment gap that currently exists with advanced dry eye management availability. Just as phacoemulsification changed the practice of cataract surgery, we must approach dry eye technology in similar fashion, as the most dominant approaches today only address half the problem and do nothing to advance the financial wellbeing of our practices.
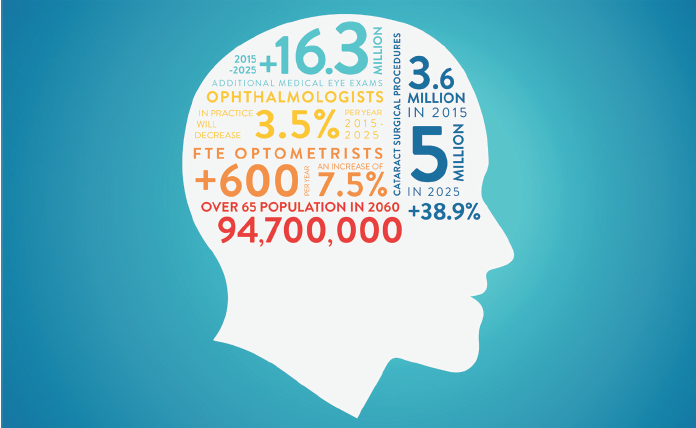
Figure. Ophthalmology and optometry in 2015 versus 2025.
When combining the decrease in reimbursement for many ophthalmic procedures to this same understanding of access and demand, it is easy to see the problem arising. Based on current projections, there will be fewer providers who will do more work for far less money in the future. To counter this trend, you need to strategically begin offering services that provide both therapeutic and economic upsides to your practice. MGD device-driven DED treatment is exactly this type of service.
DED treatment in action
At Vance Thompson Vision, we have been diligently working on developing a nomogram to better classify the diagnostic levels of DED (based on severity and progression), as well as an algorithm tool for eye care providers. This tool guides our treatment decisions while taking into consideration the diagnostic technologies now available. Our nomogram includes a three-part process: clinical indicators, treatment options, and engagement.
The first part (clinical indicators) includes the structured and standardized testing needed to diagnose patients into the correct stage of DED.
The second part (treatment options) then allows the clinician to better manage the patient by instituting the proper treatment regimen paired with the corresponding diagnostic tests.
Finally, the third part (engagement) helps to set the standard for having patients return for follow-up care. At Vance Thompson Vision there can be nearly $400 in additional office visit revenue annually when patients return for their scheduled DED follow-up appointments, in addition to the nearly $1,000 in revenue from incorporating a personalized option for MGD, like TearCare or a DED retail center.
CONCLUSION
Identifying, diagnosing, and treating DED can create sustained value for both your practice and your patients. DED is a long-term, chronic disease that affects tens of millions of people in the United States, compared to about 2 million suspected glaucoma patients in this country.1,4 DED can disrupt the quality of life for many patients. In fact, it is estimated that people spend up to $2 billion annually on DED products and treatments.1,5
Identifying those patients with signs and symptoms of DED early and educating these patients on the root causes of their DED is critical to increasing patient compliance with your selected treatment plan. Specifically targeting the root causes of each patient’s DED with products and treatments designed to improve patient clinical outcomes will make a difference in your patient’s well-being and quality of life.
DED is multifactorial, but 86% of the time it is MGD-related, driven by obstruction and inflammation. If you incorporate new testing modalities into your practice and follow a systematic protocol for management of the disease that includes inflammation control and obstruction removal, your decision-making will be less like 'practicing medicine' on your patients. You can potentially make your patients much happier and your practice more sustainable in the coming years.
1. Paulsen AJ, Cruickshanks KJ, Fischer ME, et al. Dry eye in the beaver dam offspring study: prevalence, risk factors, and health-related quality of life. Am J Ophthalmol. 2014;157(4):799-806.
2. Vespa J, Medina L, Armstrong DM. Demographic turning points for the United States: population projections for 2020 to 2060. census.gov. https://www.census.gov/content/dam/Census/library/publications/2020/demo/p25-1144.pdf. Published March 2018. Accessed July 6, 2020.
3. Ram J, Gupta A, Brar G, et al. Outcomes of phacoemulsification in patients with dry eye. J Cataract Refract Surg. 2002;28:1386-1389.
4. Trattler WB, Majmudar PA, Donnenfeld ED, et al. The prospective health assessment of cataract patients’ ocular surface (PHACO) study: the effect of dry eye. Clin Ophthalmol. 2017;11:1423-1430.
5. Lemp MA, Crews LA, Bron AJ, et al. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea. 2012;31(5):472-478.
6. Sullivan BD, Crews LA, Messmer EM, et al. Correlations between commonly used objective signs and symptoms for the diagnosis of dry eye disease: clinical implications. Acta Ophthalmol. 2014;92(2):161-166.
7. Ngo W, Situ P, Keir N, et al. Psychometric properties and validation of the standard patient evaluation of eye dryness questionnaire. Cornea. 2013;32(9):1204-1210.
7/20 TC-1110-US.v1

